Sam Van Boxstael, Catherine Vandepitte, Philippe E. Gautier, and Hassanin Jalil
FACTS
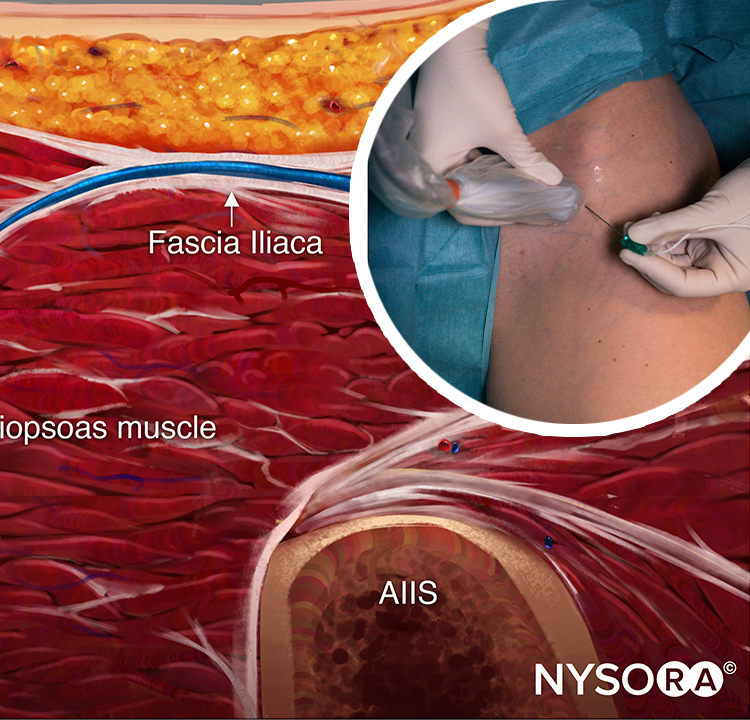
- Indications: Relief of painful adductor muscle contractions, to prevent adduction of the thigh during transurethral bladder surgery, additional analgesia after major knee surgery, and may provide postoperative analgesia after hamstring tendon harvest for anterior cruciate ligament (ACL) reconstruction (Figure 1).
- Transducer position: medial aspect of the proximal thigh.
- Goal: Local anesthetic spread in the interfascial plane in which the nerves lie or around the anterior and posterior branches of the obturator nerve.
- Local anesthetic: 5 mL into each interfascial space or around the branches of the obturator nerve.

FIGURE 1. Expected distribution of obturator nerve sensory and motor block.
GENERAL CONSIDERATIONS
Ultrasound (US)-guided obturator nerve block is simpler to perform and more reliable than surface landmark–based techniques. There are two approaches to performing a US-guided obturator nerve block. The interfascial injection technique relies on injecting local anesthetic solution into the fascial planes that contain the branches of the obturator nerve. With this technique, it is not important to identify the branches of the obturator nerve on the sonogram, but rather to identify the adductor muscles and the fascial boundaries within which the nerves lie. This is similar in concept to other fascial plane blocks (eg, the transversus abdominis plane [TAP] block in which local anesthetic solution is injected between the internal oblique and transverse abdominis muscles without the need to identify the nerves). Alternatively, the branches of the obturator nerve can be visualized with US imaging and blocked after eliciting a motor response.
ULTRASOUND ANATOMY
The obturator nerve forms in the lumbar plexus from the anterior primary rami of the L2–L4 roots and descends to the pelvis on the medial side of the psoas muscle. In most individuals, the nerve divides into an anterior branch and posterior branch before exiting the pelvis through the obturator foramen. In the thigh, at the level of the femoral crease, the anterior branch is located between the fascia of the pectineus and adductor brevis muscles. The anterior branch lies further caudad between the adductor longus and adductor brevis muscles. The anterior branch provides motor fibers to the adductor longus, brevis and gracilis muscles; and cutaneous branches to the medial aspect of the thigh. The anterior branch has great variability in the extent of sensory innervation of the medial thigh.
The posterior branch lies between the fascial planes of the adductor brevis and adductor magnus muscles (Figures 2 and 3). The posterior branch is primarily a motor nerve for the adductors of the thigh; however, it also may provide articular branches to the medial aspect of the knee joint. The articular branches to the hip joint usually arise from the obturator nerve, proximal to its division and only occasionally from the individual branches (Figure 4). In 8–30% of patients, an accessory obturator nerve arises from L3 and L4, travels with the femoral nerve, and gives branches to the hip joint
A helpful mnemonic to remember the order of the adductor muscles, from anterior to posterior, is as follows: Alabama: Adductor Longus, Adductor Brevis, Adductor MAgnus.
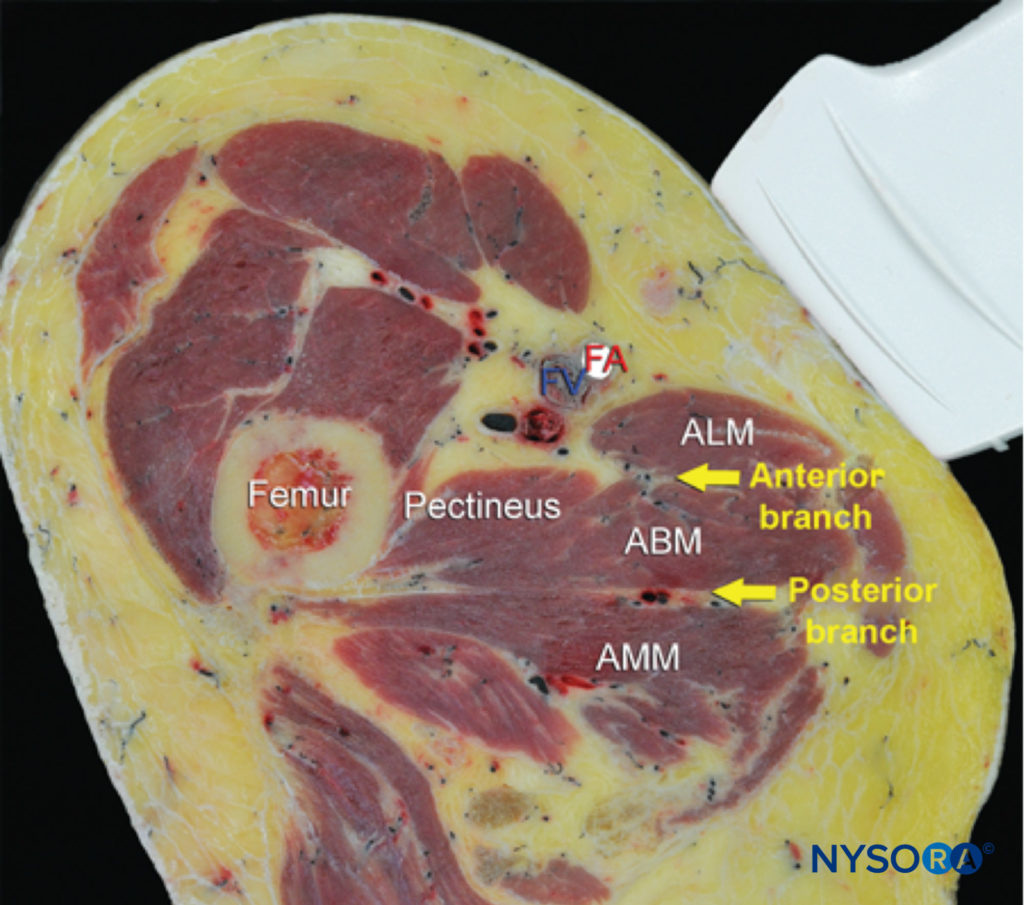
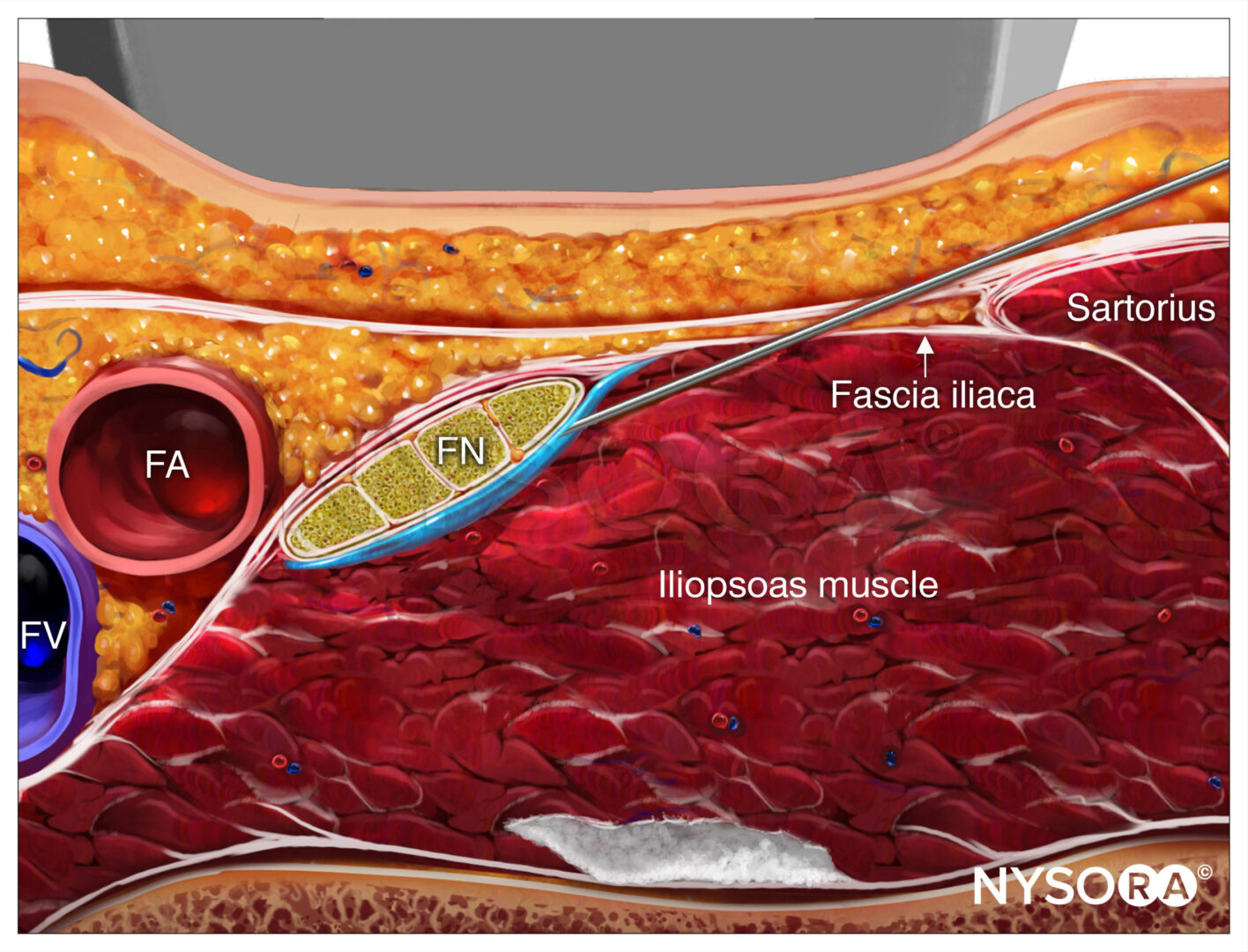
FIGURE 2. Cross-sectional anatomy of relevance to the obturator nerve block. Shown are the femoral vessels (the femoral vein [FV] and femoral artery [FA]), pectineus muscle, adductor longus muscle (ALM), adductor brevis muscle (ABM), and adductor magnus muscle (AMM). The anterior branch of the obturator nerve is seen between the ALM and ABM, whereas the posterior branch is seen between the ABM and AMM. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
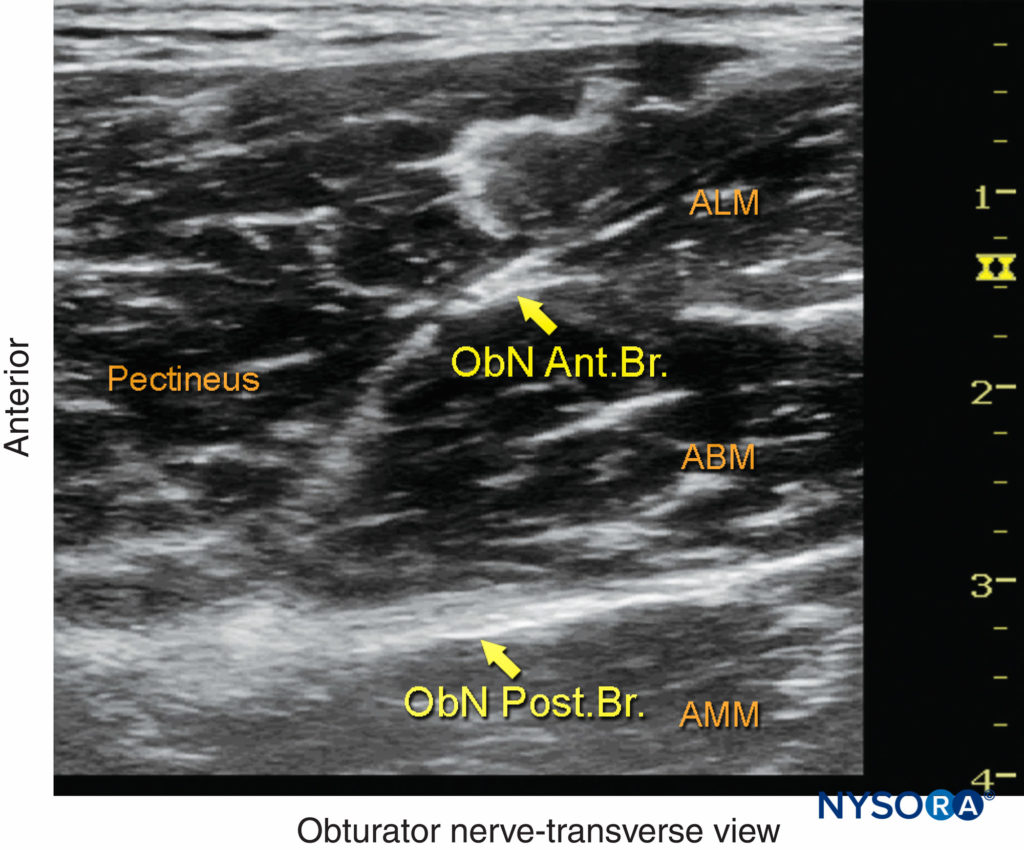
FIGURE 3. The anterior branch (ant. br.) of the obturator nerve (ObN) is seen between the adductor longus muscle (ALM) and the adductor brevis muscle (ABM), whereas the posterior branch (post. br.) is seen between the ABM and the adductor magnus muscle (AMM). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, Inc.; 2011.)
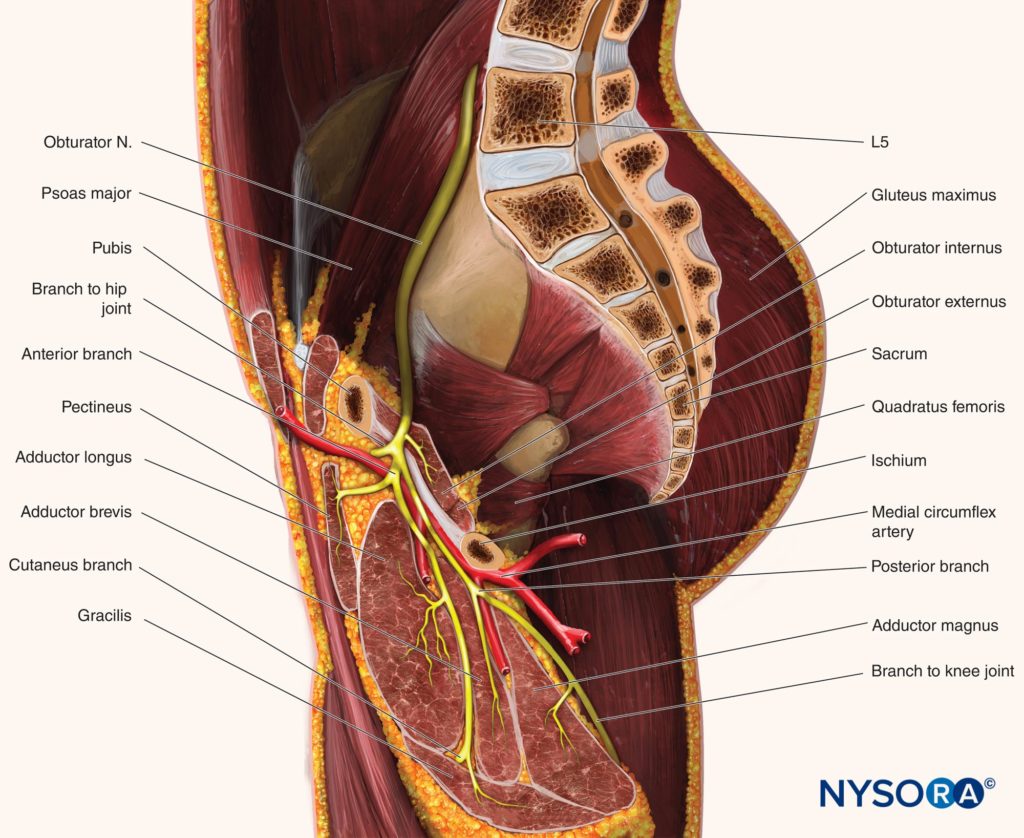
FIGURE 4. The course and divisions of the obturator nerve and its relationship to the adductor muscles.
NYSORA Tips
A psoas compartment (lumbar plexus) block is required to reliably block the articular branches of the obturator nerve to the hip joint because they usually depart proximal to the level at which the obturator nerve block is performed in the proximal thigh.
For a more comprehensive review of the lumbar plexus, see Functional Regional Anesthesia Anatomy
DISTRIBUTION OF ANESTHESIA
Because there is great variability in the cutaneous innervation to the medial thigh, demonstrated weakness of adductor muscle strength is the only reliable method of documenting a successful obturator nerve block (Figure 1).
However, the adductor muscles of the thigh may have co-innervation from the femoral nerve (pectineus) and the sciatic nerve (adductor magnus).
Adductor motor strength is decreased by about 25% following femoral nerve block and 11% following sciatic nerve block. For this reason, complete loss of adductor muscle strength is uncommon despite a successful obturator nerve block.
NYSORA Tips
A simple method of assessing adductor muscle strength (motor block) is to instruct the patient to adduct the blocked leg from an abducted position against resistance. Weakness or inability to adduct the leg indicates a successful obturator nerve block.
EQUIPMENT
The equipment recommended for an obturator nerve block includes the following:
- Ultrasound machine with linear (or curved) transducer (5–13 MHz), sterile sleeve, and gel
- Standard block tray
- A 10-mL syringe containing local anesthetic solution
- A 10-cm, 21- to 22-gauge, short-bevel, insulated needle
- Peripheral nerve stimulator (optional)
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
With the patient supine, the thigh is slightly abducted and laterally rotated. The block can be performed either at the level of femoral (inguinal) crease medial to the femoral vein or 1–3 cm inferior to the inguinal crease on the medial aspect (adductor compartment) of the thigh (Figure 5).

FIGURE 5. Transducer position to image the obturator nerve. The transducer is positioned medial to the femoral artery, slightly below the femoral crease. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, Inc.; 2011.)
GOAL
The goal of the interfascial injection technique for blocking the obturator nerve is to inject local anesthetic solution into the interfascial space between the pectineus and adductor brevis muscles to block the anterior branch and the adductor brevis and adductor magnus muscles to block the posterior branch.
When using US guidance with nerve stimulation, the anterior and posterior branches of the obturator nerve are identified and stimulated to elicit a motor response prior to injecting local anesthetic solution around each branch.
TECHNIQUE
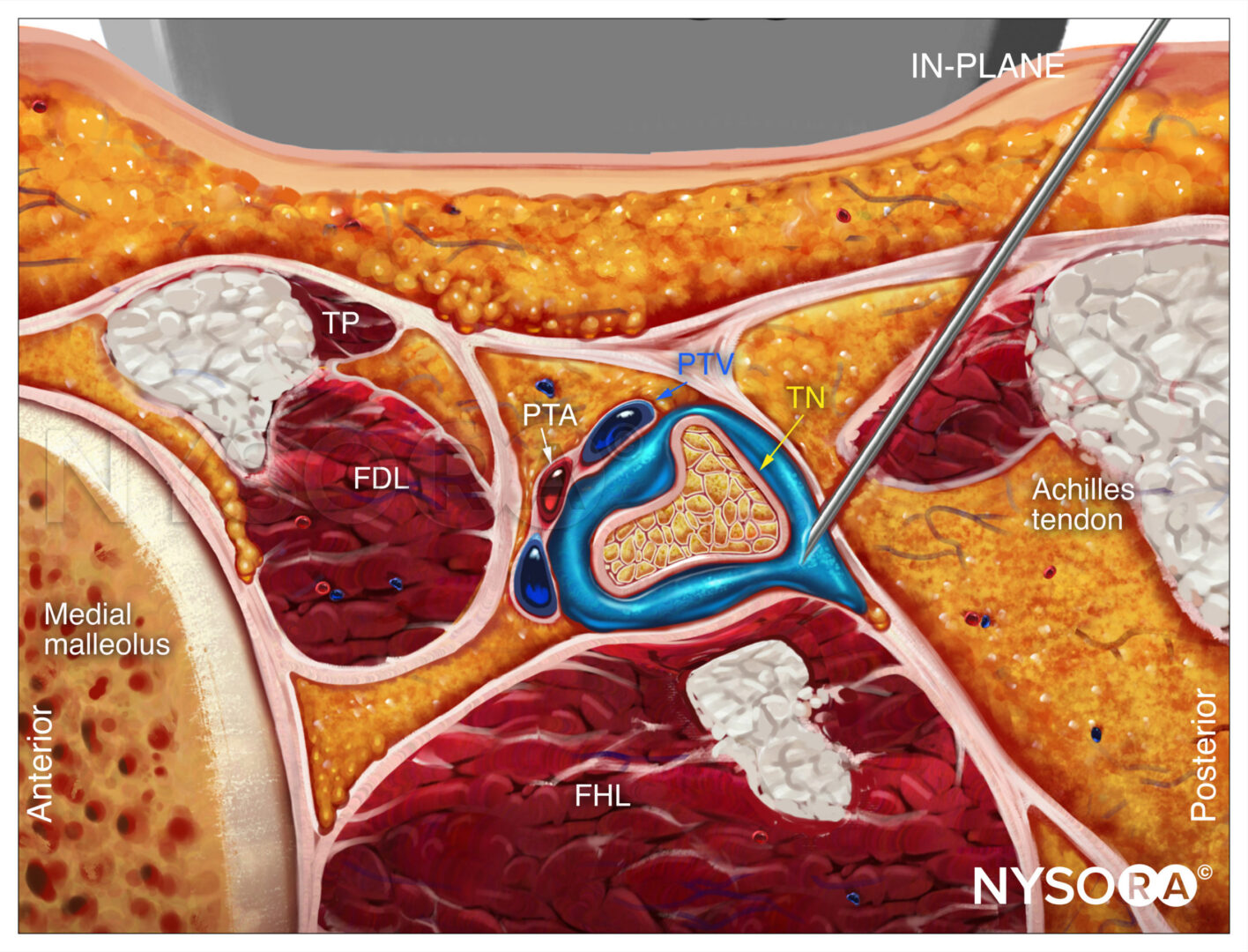
The interfascial approach is performed at the level of the femoral crease. With this technique, it is important to identify the adductor muscles and the fascial planes in which the individual nerves are enveloped. Color Doppler can be used to visualize the obturator arteries located near the nerve branches in order to avoid puncturing them, although they are not always visible.
The US transducer is placed to visualize the femoral vessels. The transducer is advanced medially along the crease to identify the adductor muscles and their fasciae. The anterior branch is sandwiched between the pectineus and adductor brevis muscles, whereas the posterior branch is located in the fascial plane between the adductor brevis and adductor magnus muscles. The block needle is advanced to initially position the needle tip between the pectineus and adductor brevis (Figure 6a).
At this point, 5–10 mL of local anesthetic solution is injected.
The needle is advanced farther to position the needle tip between the adductor brevis and adductor magnus muscles, and another 5–10 mL of local anesthetic solution is injected (Figure 6b). It is important for the local anesthetic solution to spread into the interfascial space and not be injected into the muscles. Correct injection of local anesthetic solution into the interfascial space results in an accumulation of the injectate between the target muscles. The needle may have to be repositioned to allow for precise interfascial injection.
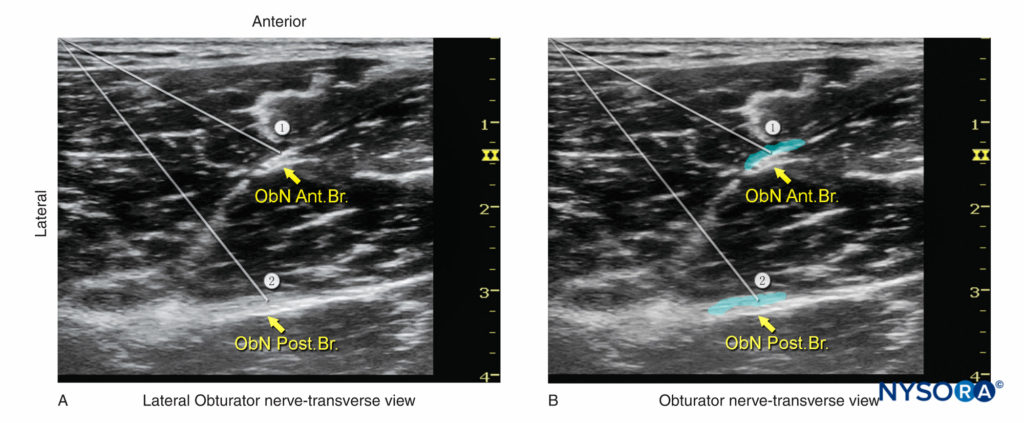
FIGURE 6. (A) Needle paths (1, 2) required to reach the anterior branch (ant. br.) and posterior branch (post. br.) of the obturator nerve (ObN). (B) Simulated dispersion of local anesthetic (blue-shaded areas) to block the anterior and posterior branches of the obturator nerve. In both examples, an in-plane needle insertion has been used. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, Inc.; 2011.)
Alternatively, the cross-sectional image of obturator nerve branches can be obtained by scanning 1–3 cm distal to the inguinal crease on the medial aspect of thigh. The nerves appear as hyperechoic, flat, thin, fusiform-shaped structures invested in the fascia of the adductor muscles. The anterior branch is located between the adductor longus and adductor brevis muscles, whereas the posterior branch is located between the adductor brevis and adductor magnus muscles. An insulated block needle attached to the nerve stimulator is advanced toward the nerve with either an out-of-plane or in-plane trajectory. After eliciting contraction of the adductor muscles, 5–7 mL of local anesthetic is injected around each branch of the obturator nerve (see Figure 6b).
Continue reading: Obturator Nerve Block – Landmarks and nerve stimulator technique
REFERENCES
- Sakura S, Hara K, Ota J, Tadenuma S: Ultrasound-guided peripheral nerve blocks for anterior cruciate ligament reconstruction: effect of obturator nerve block during and after surgery. J Anesth 2010;24:411–417.
- Akkaya T, Comert A, Kendir S, et al: Detailed anatomy of accessory obturator nerve block. Minerva Anestesiol 2008;74:119–122.
- Akkaya T, Comert A, Kendir S, et al: Detailed anatomy of accessory obturator nerve block. Minerva Anestesiol 2008;74:119–122.
- Akkaya T, Ozturk E, Comert A, et al. Ultrasound-guided obturator nerve block: a sonoanatomic study of a new methodologic approach. Anesth Analg 2009;108:1037–1041.
- Anagnostopoulou S, Kostopanagiotou G, Paraskeuopoulos T, Chantzi C, Lolis E, Saranteas T: Anatomic variations of the obturator nerve in the inguinal region: implications in conventional and ultrasound regional anesthesia techniques. Reg Anesth Pain Med 2009;34:33–39.
- Bouaziz H, Vial F, Jochum D, et al: An evaluation of the cutaneous distribution after obturator nerve block. Anesth Analg 2002;94:445–449.
- Macalou D, Trueck S, Meuret P, et al. Postoperative analgesia after total knee replacement: the effect of an obturator nerve block added to the femoral 3-in-1 nerve block. Anesth Analg 2004;99:251–254.
- Marhofer P, Harrop-Griffiths W, Willschke H, Kirchmair L: Fifteen years of ultrasound guidance in regional anaesthesia: part 2—recent developments in block techniques. Br J Anaesth 2010;104:673–683.
- McNamee DA, Parks L, Milligan KR: Post-operative analgesia following total knee replacement: an evaluation of the addition of an obturator nerve block to combined femoral and sciatic nerve block. Acta Anaesthesiol Scand 2002;46:95–99.
- Sakura S, Hara K, Ota J, Tadenuma S: Ultrasound-guided peripheral nerve blocks for anterior cruciate ligament reconstruction: effect of obturator nerve block during and after surgery. J Anesth 2010;24:411–417.
- Sinha SK, Abrams JH, Houle T, Weller R: Ultrasound guided obturator nerve block: an interfascial injection approach without nerve stimulation. Reg Anesth Pain Med 2009;34:261–264.
- Snaith R, Dolan J: Ultrasound-guided interfascial injection for peripheral obturator nerve block in the thigh. Reg Anesth Pain Med 2010;35: 314–315.
- Soong J, Schafhalter-Zoppoth I, Gray AT: Sonographic imaging of the obturator nerve for regional block. Reg Anesth Pain Med 2007;32: 146–151.
- Taha AM: Brief reports: ultrasound-guided obturator nerve block: a proximal interfascial technique. Anesth Analg 2012;114:236–239.