Manoj K. Karmakar
INTRODUCTION
Lumbar plexus block (LPB) produces anesthesia of the major components of the ipsilateral lumbar plexus, the femoral nerve (FN), lateral femoral cutaneous nerve (LFCN), and the obturator nerve (OBN). LPB is used as a sole technique or in combination with a sciatic nerve block for anesthesia or analgesia in patients having hip or lower extremity surgery. It is also referred to as psoas compartment block (PCB) or posterior lumbar plexus block (PLB). The term PCB was originally coined by Chayen and colleagues. They believed that branches of the lumbar plexus and parts of the sacral plexus were located close to each other in a “compartment” between the psoas major and quadratus lumborum muscles at the level of the L4 vertebral and could be identified using “loss of resistance.” However, the lumbar plexus is located within the substance of the psoas muscle and local anesthetic is injected into a fascial plane within the posterior aspect of the psoas muscle during an LPB.
LPB is traditionally performed using surface anatomical landmarks and peripheral nerve stimulation. The main challenges with accomplishing LPB with anatomical landmarks and peripheral nerve stimulation relate to the depth at which the lumbar plexus is located. Small errors in estimation of landmark or angle of needle insertion can lead to the block needle being directed away from the plexus, resulting in inadvertent deep needle insertion or renal or vascular injury.
Therefore, real-time monitoring of the needle and local anesthetic injection during an LPB is desirable and may improve the accuracy and safety of the technique. While fluoroscopy and computed tomography can be used to improve precision during an LPB, they are impractical in a busy operating room environment, costly, and, more importantly, associated with exposure to radiation. Ultrasound (US) is increasingly being used to guide peripheral nerve blocks, and it is only logical that ultrasound-guided (USG) LPB is of interest because of the ever-increasing availability of US machines, which produce high-quality images, in the operating room. US has been used to preview the relevant anatomy, measure the depth to the transverse process, guide the block needle to the posterior aspect of the psoas muscle or the lumbar plexus in real time, and monitor needle–nerve contact10 or spread of local anesthetic during an LPB. Understanding the sonoanatomy of the lumbar paravertebral region is a prerequisite to using US for LPB. This chapter briefly describes the techniques used to perform lumbar paravertebral sonography, the relevant sonoanatomy, and the practical considerations for using US for LPB.
GROSS ANATOMY
The lumbar plexus is formed by the union of the anterior primary rami of L1, L2, and L3 and the greater part of L4 (Figure 1) within the substance of the psoas muscle (Figures 2, 3, 4, and 5). It also receives a variable contribution from T12 (subcostal nerve) and L5 (see Figure 1). The lumbar plexus is located in an intramuscular fascial plane or “compartment,” also referred to as the psoas compartment, within the posterior one-third of the psoas muscle (Figure 6) and is very closely related to the lumbar transverse processes.
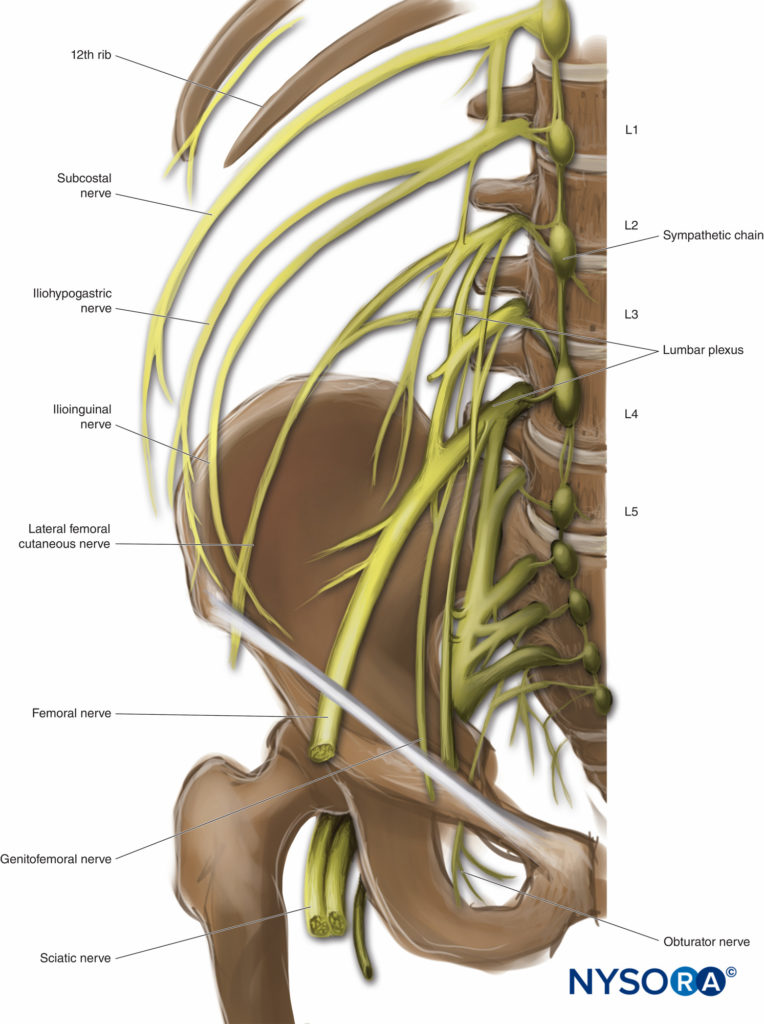
FIGURE 1. Lumbar plexus and its three major components: the lateral femoral cutaneous, obturator, and femoral nerves. Note the close anatomical relation of the lumbar plexus to the transverse processes of the vertebra and the lumbar sympathetic chain.
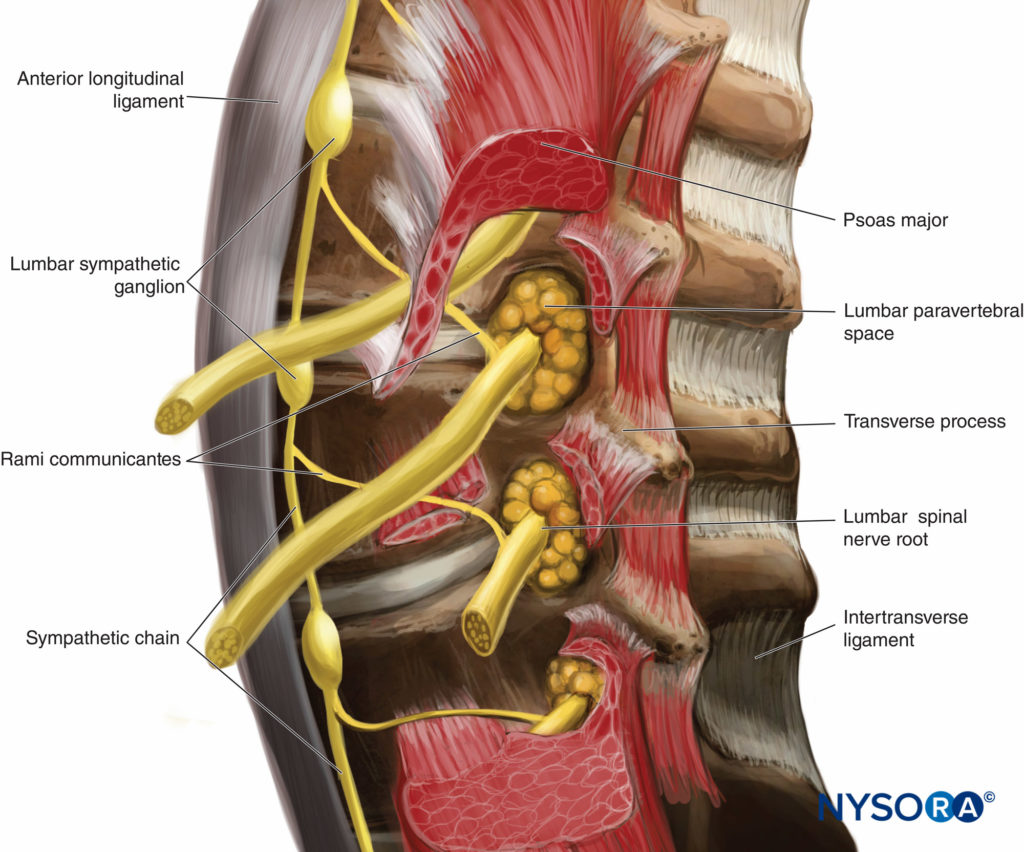
FIGURE 2. Location of the lumbar nerve roots within the substance of the psoas muscle and its relation to the transverse process of the lumbar vertebrae. Also note the formation of the lumbar paravertebral space between the larger (fleshy) anterior part of the psoas muscle, which originates from the anterolateral surface of the vertebral body, and the thinner (accessory) posterior part of the muscle, which originates from the anterior aspect of the transverse processes.
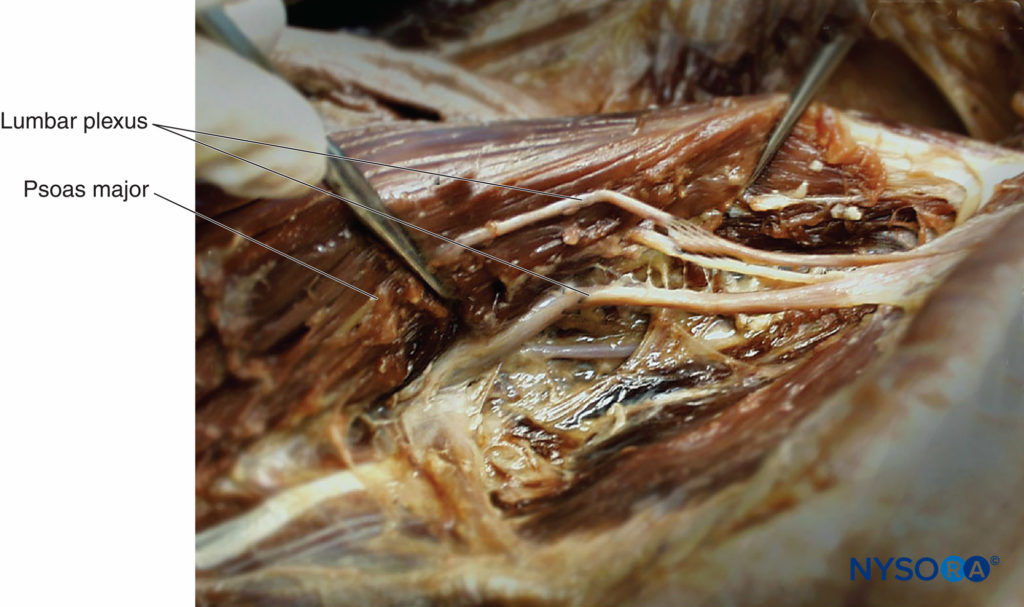
FIGURE 3. Human cadaver dissection image showing the lumbar plexus nerves within the substance of the psoas muscle. The psoas muscle has been split longitudinally to expose the lumbar plexus nerves within the posterior aspect of the muscle.
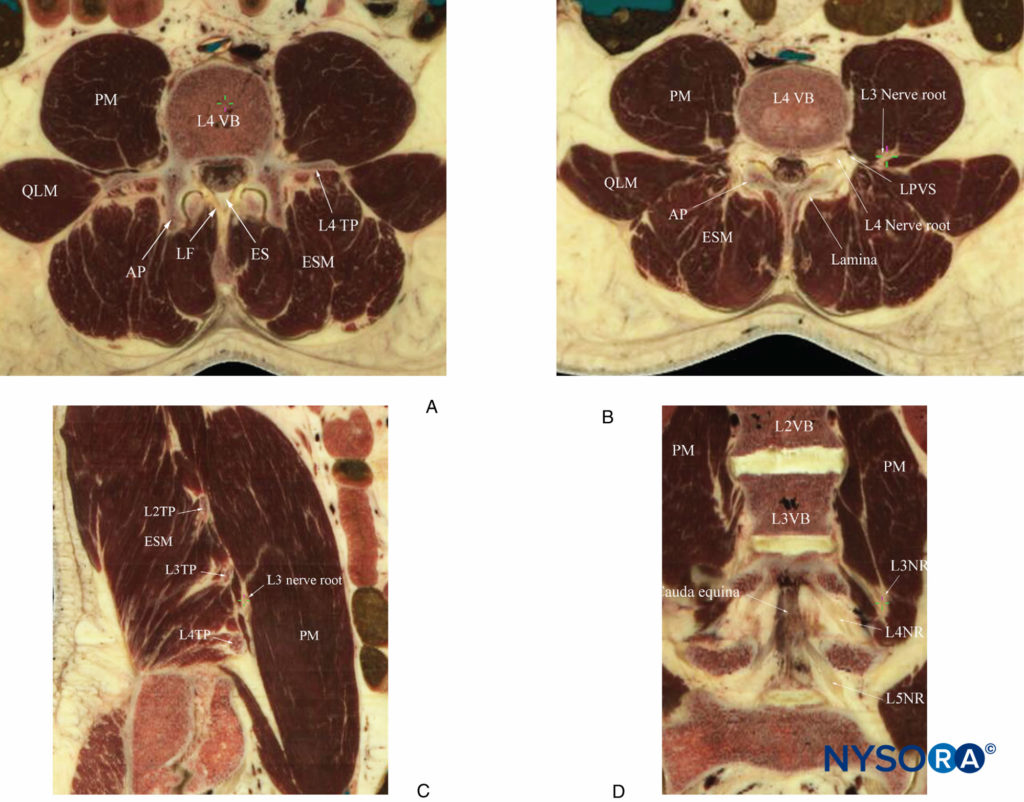
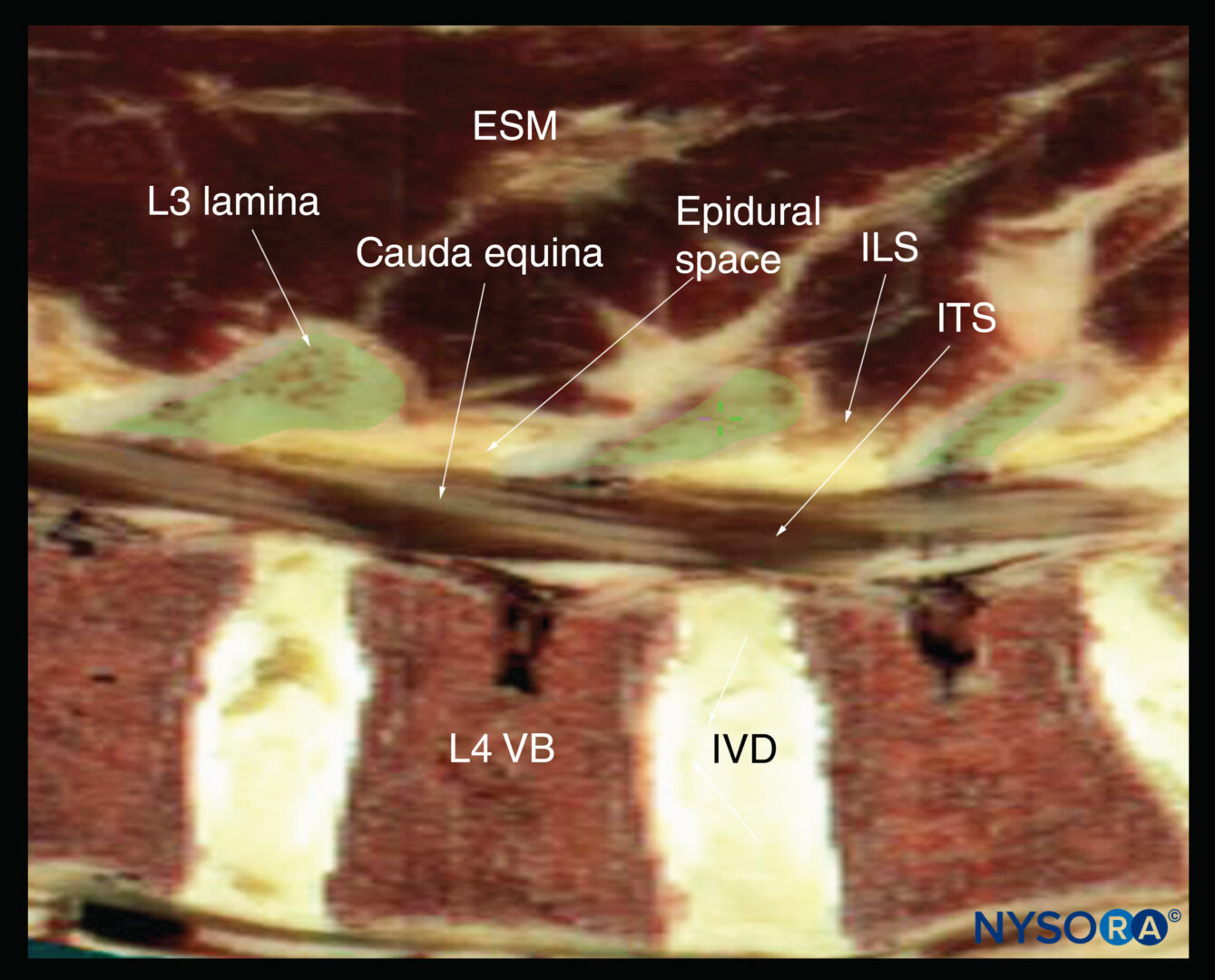
FIGURE 4. Multiplanar cadaver anatomical sections showing the anatomical relation of the lumbar nerve root and lumbar plexus to the psoas muscle (PM). (A) Cross-section through the L4 vertebral body and transverse process, corresponding to the level at which the paramedian transverse oblique scan at the level of the transverse process (PMOTS-TP) is performed. (B) Cross-sectional cadaver anatomical section from just inferior to the L4 transverse process and through the lower part of the L4 vertebral body, corresponding to the level at which the paramedian transverse oblique scan through the intertransverse space and at the level of the articular process (PMOTS-AP) is performed. (C) Sagittal cadaver anatomical section showing the relation of the lumbar plexus to the transverse process (TP) and PM. (D) Coronal cadaver anatomical section showing how the lumbar nerve roots, after they exit the intervertebral foramen, take a steep caudal course and enter the substance of the PM more caudally. The “reference-marker” of the Java application is seen as a “green cross-hair,” which represents the same anatomical point in the multiplanar cadaver anatomical sections. AP, articular process; ES, epidural space; ESM, erector spinae muscle; LF, ligamentum flavum; LPVS, lumbar paravertebral space; NR, nerve root; QLM, quadratus lumborum muscle; TP, transverse process; VB, vertebral body.
The larger anterior (fleshy) part of the psoas muscle originates from the anterolateral surface of the vertebral body and the intervertebral disc, while the thinner posterior (accessory) part of the psoas muscle originates from the anterior aspect of the transverse processes (see Figure 2).
The two parts of the muscle fuse to form the main bulk of the psoas muscle, but close to the vertebral bodies, they are separated by a fascia or space (see Figure 2) that contains the lumbar nerve root, branches of the lumbar artery (Figures 6 and 7), and the ascending lumbar vein. This wedgeshaped space close to the intervertebral foramen is called the lumbar paravertebral space (LPVS) (see Figures 4,5 and 6). After it exits the intervertebral foramen, the lumbar nerve root enters the LPVS (see Figures 4,5 and 6), after which, instead of entering the psoas muscle at the same vertebral level, it takes a steep caudal course (see Figures Figures 4,5 and 6) and enters the psoas compartment at the vertebral level below (see Figures Figures 4,5 and 6). This explains why the L3 contribution to the lumbar plexus lies opposite the L4 intervertebral foramen and the L4 nerve root (see Figures 4 and 5). It is not known if the LPVS is continuous with the psoas compartment at the same vertebral level, but the occurrence of epidural spread after a lumbar plexus block suggests that it is. Once the plexus is formed, it is visualized as a triangular shape, narrow cranially and wider at its caudal portion (see Figure 5). The nerves that originate from the plexus also exhibit a fanned-out distribution, with the LFC being outermost, the OBN innermost, and the FN in between. The positions of the LFC and FN within the psoas compartment are relatively consistent, but the position of the OBN is variable and may even lie in a fold of the psoas muscle separate from that enclosing the other two nerves (Figure 8). The depth from the skin to the lumbar plexus also varies with gender and body mass index (BMI).
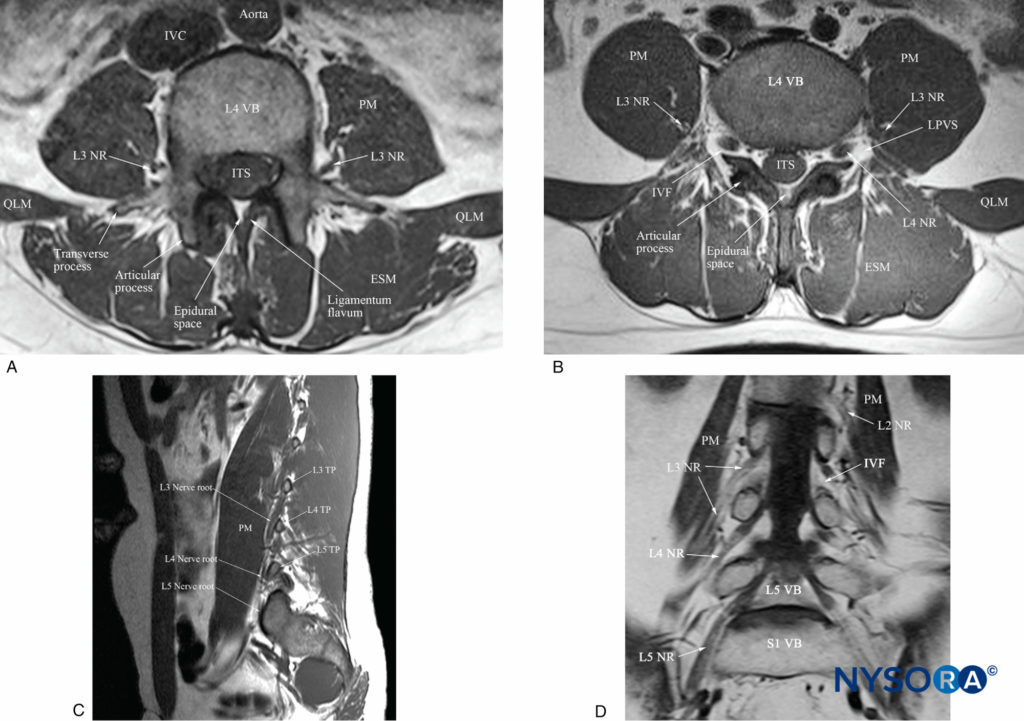
FIGURE 5. Multiplanar T1-weighted magnetic resonance imaging (MRI) images showing the anatomical relation of the lumbar nerve root and lumbar plexus to the psoas muscle (PM). (A) Transverse view at the level of the L4 vertebral body and the transverse process, corresponding to the level at which the paramedian transverse oblique scan at the level of the transverse process (PMOTS-TP) is performed. (B) Transverse view from just below the L4 transverse process and through the lower half of the body of the L4 vertebra and the articular process (inferior), corresponding to the level at which the paramedian transverse oblique scan at the level of the articular process (PMOTS-AP) is performed. Note the hypointense L4 nerve root as it exits the intervertebral foramen (IVF) and enters the hyperintense fatfilled lumbar paravertebral space (LPVS). Also seen in the posterior aspect of the psoas muscle is the L3 nerve of the lumbar plexus, which is surrounded by a layer or hyperintense fat and situated within an intramuscular compartment (the “psoas compartment”). (C) Sagittal view of the lumbar paravertebral region at the L3–L5 vertebral level showing the steep caudal course of the lumbar nerve roots. (D) Coronal view at the L3–L5 vertebral level showing the steep caudal course of the lumbar spinal nerves after they emerge from the IVF. ESM, erector spinae muscle; ITS, intrathecal space; IVC, inferior vena cava; LPVS, lumbar paravertebral space; NR, nerve root; QLM, quadratus lumborum muscle; VB, vertebral body.
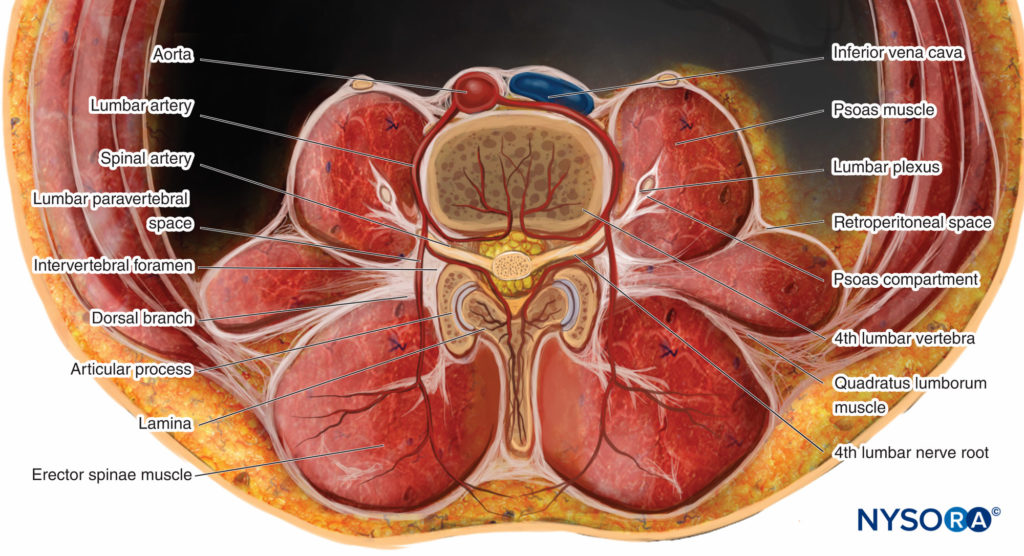
FIGURE 6. Transverse anatomy of the lumbar paravertebral region at the L4 vertebral level. Note the origin and branching of the lumbar artery.
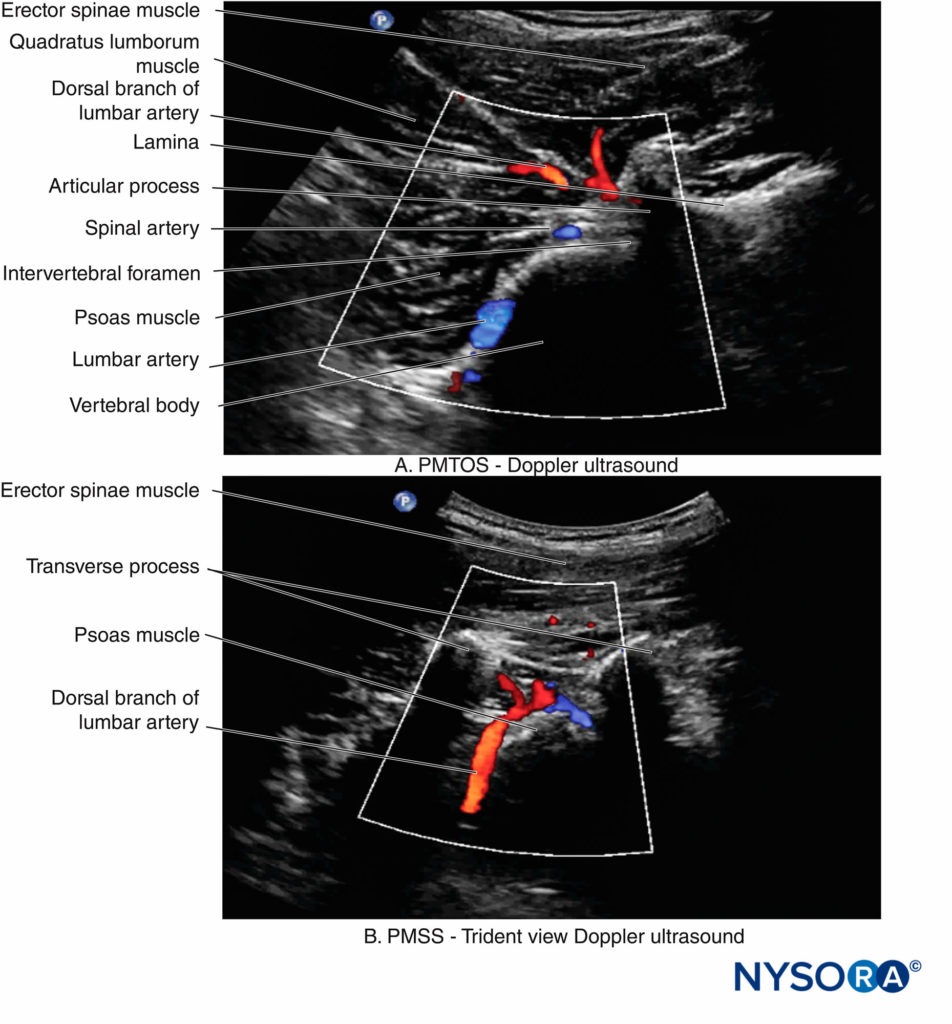
FIGURE 7. Color Doppler US images of the lumbar paravertebral region in the (A) transverse and (B) sagittal scan planes. Note the dorsal branch of the lumbar artery on the posterior aspect of the psoas muscle in both the transverse and sagittal sonograms and the spinal artery in the transverse sonogram. PMSS, paramedian sagittal scan; PMTOS, paramedian transverse oblique scan.
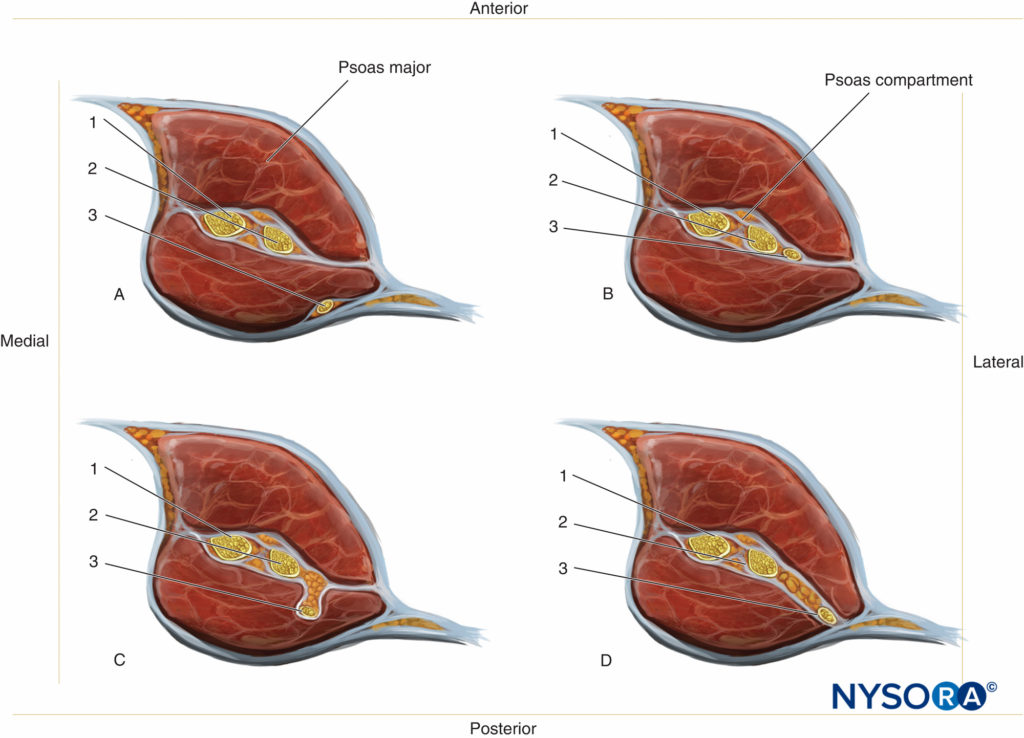
FIGURE 8. Position of the (1) lateral femoral cutaneous nerve; (2) femoral nerve; and (3) obturator nerve in the psoas compartment. Note that while the positions of 1 and 2 are fairly consistent, the position of 3 can vary and may even lie in a separate intramuscular fold (c) or compartment separate from the psoas compartment.
For a more comprehensive review of the lumbar plexus distribution, see Functional Regional Anesthesia Anatomy.
SONOANATOMY FOR LUMBAR PLEXUS BLOCK
General Considerations
The depth of the lumbar plexus necessitates the use of lowfrequency US (5–10 MHz) and curved array transducers to image the lumbar paravertebral anatomy. Low-frequency US provides good penetration but lacks spatial resolution at the depths (5–9 cm) at which the anatomy relevant for LPB is located. The lack of spatial resolution often compromises the ability to locate the lumbar plexus nerves within the psoas muscle. However, recent improvements in US technology, the image processing capabilities of US machines, the availability of compound imaging and tissue harmonic imaging (THI), and the use of new US scan protocols have all contributed to improved imaging of the lumbar paravertebral region.
Ultrasound Scan Techniques
Ultrasound scan for LPB can be performed in the transverse or sagittal axis (Figures 9 and 10) and with the patient in the lateral, sitting, or prone position. A disadvantage of performing LPB with the patient in the prone position is that this position impairs visualization of the quadriceps muscle contraction that is used as an endpoint for needle placement. The author prefers to perform the US scan with the patient in the lateral decubitus position with the side to be blocked uppermost (see Figure 9). The following anatomical landmarks are identified and marked on the skin of the nondependent side of the back: the posterior superior iliac spine, iliac crest, lumbar spinous processes (midline; see Figure 9) and intercristal line (see Figure 9).
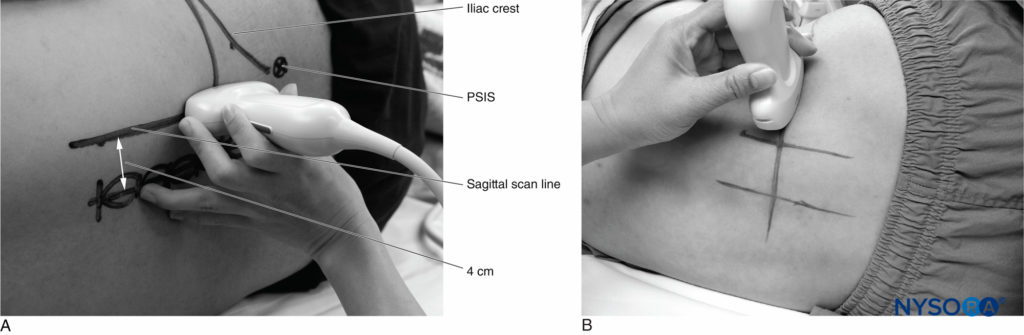
FIGURE 9. Position of the patient and US transducer during (A) a paramedian sagittal (PMSS) and (B) a paramedian transverse oblique (PMTOS) scan of the lumbar paravertebral region. For the PMSS, the US transducer is placed over the “sagittal scan” line, which is a line 4 cm lateral and parallel to the midline (paramedian), at the level of the iliac crest. For the PMTOS, the US transducer is placed laterally to the sagittal scan line and over the intercristal line. Note how the transducer is angled medially for the PMTOS. PSIS, posterior superior iliac spine.
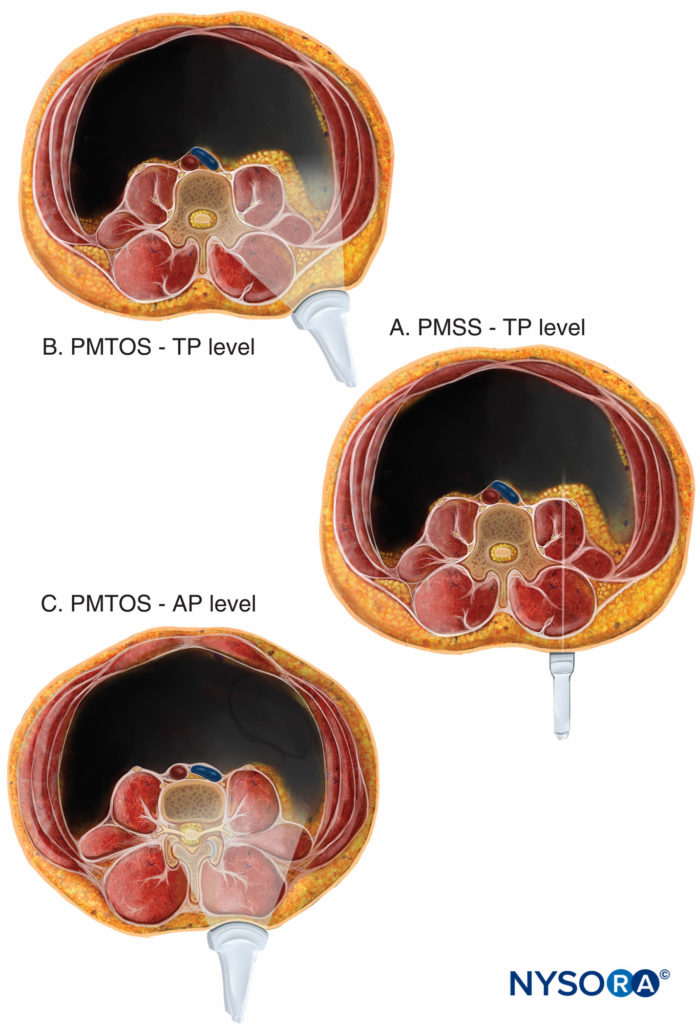
FIGURE 10. Plane of US imaging during a sagittal and transverse scan of the lumbar paravertebral region for lumbar plexus block. An image of a US transducer and the plane of the US beam has been superimposed onto transverse anatomical sections of the lumbar paravertebral region to illustrate how the US beam is insonated during (A) paramedian sagittal scan at the level of the transverse process (PMSS-TP); (B) paramedian transverse oblique scan at the level of the transverse process (PMTOS-TP); and (C) paramedian transverse oblique scan at the level of the articular process (PMTOS-AP).
Thereafter, a line parallel to the midline, which intersects the intercristal line at a point 4 cm lateral to the midline (paramedian), corresponding to the point at which the block needle is inserted during a landmark-based LPB, is also marked (sagittal scan line; see Figure 9). The target vertebral level for the US scan (L3/4/5) is then identified as previously described. This involves visualizing the lumbosacral junction (L5–S1 gap) on a sagittal sonogram and then counting cranially to locate the lamina and transverse processes of the L3, L4, and L5 vertebrae.
A liberal amount of ultrasound gel is applied to the skin over the lumbar paravertebral region for acoustic coupling. To simplify image orientation, irrespective of the side imaged, the orientation marker of the US transducer is directed cranially during a sagittal scan and laterally (outward) during a transverse scan. For a sagittal scan (Figures 9, 10, 11, and 12), the US transducer is positioned over the sagittal scan line (see Figure 9a) with its orientation marker directed cranially. For a transverse scan (Figures 9,10, 13, and 14), the US transducer is positioned 4 cm laterally to the midline along the intercristal line and just above the iliac crest (see Figure 9b). The transducer is also directed slightly medially (paramedian transverse oblique scan [PMTOS]; see Figure 9b) so as to produce a transverse oblique view of the lumbar paravertebral region (see Figures 13 and 14).
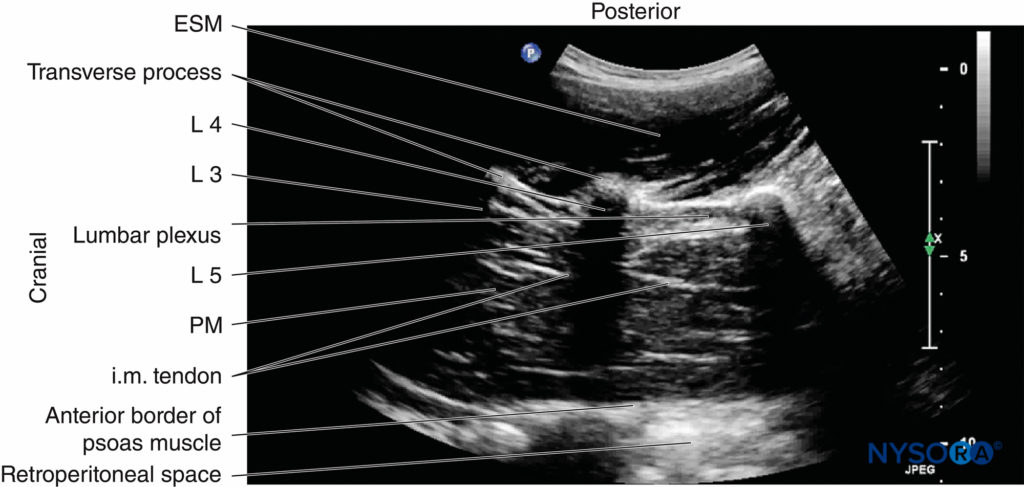
FIGURE 11. Sagittal sonogram of the lumbar paravertebral region showing the lumbar plexus as a hyperechoic structure in the posterior aspect of the psoas muscle (PM) between the L4 and L5 transverse processes. Also note the hyperechoic intramuscular tendons within the bulk of the psoas muscle. ESM, erector spinae muscle; i.m. tendon = intramuscular tendon.
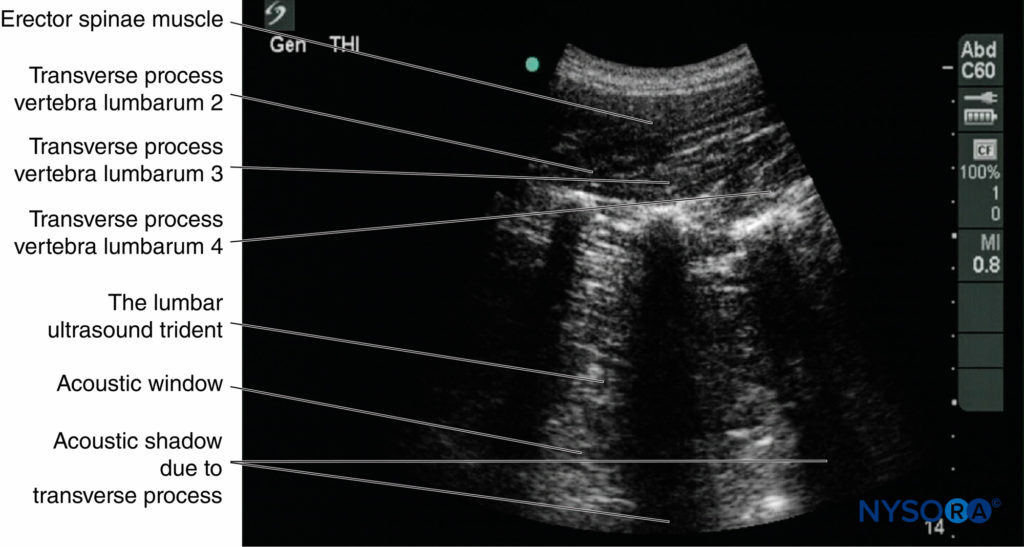
FIGURE 12. Sagittal sonogram of the lumbar paravertebral region showing the acoustic shadows of the lumbar transverse processes (L3, L4, and L5), which produce a sonographic pattern called the “trident sign.” The psoas muscle is seen in the intervening acoustic window.
During a PMTOS, the US beam can be insonated either at the level of the transverse process (PMTOS-TP; see Figures 10b and 13 or through the intertransverse space at the level of the articular process (PMTOS-AP: see Figures 10c and 14). Alternatively, a transverse scan can be performed by placing the US transducer more anteriorly in the flank and above the iliac crest (Figures 15, 16, 17, 18, and 19), as described by Sauter and colleagues with the “shamrock method.”
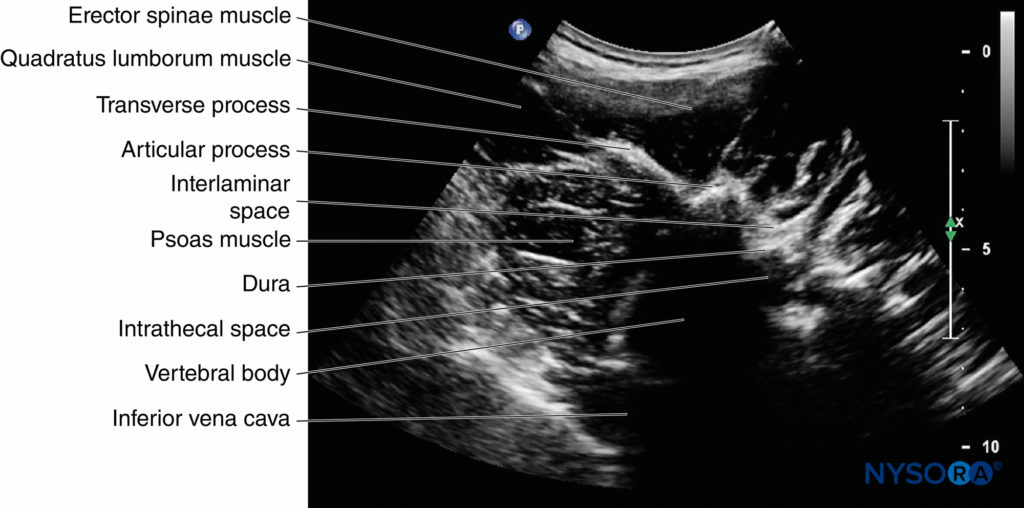
FIGURE 13. Paramedian transverse oblique scan of the lumbar paravertebral region at the level of the transverse process (PMTOS-TP). Note how the acoustic shadow of the transverse process obscures the posterior part of the psoas muscle and the intervertebral foramen and how parts of the spinal canal and neuraxial structures (dura and intrathecal space) are seen through the interlaminar space.
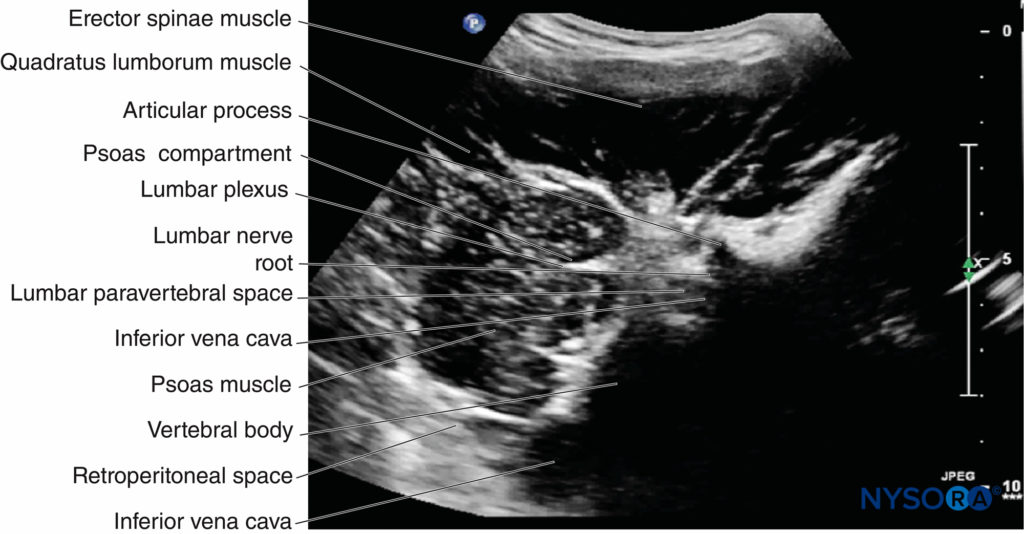
FIGURE 14. Paramedian transverse oblique scan of the right lumbar paravertebral region through the lumbar intertransverse space and at the level of the articular process, showing the lumbar plexus as a discrete hyperechoic structure within a hypoechoic intramuscular space (the psoas compartment) in the posteromedial aspect of the psoas muscle.
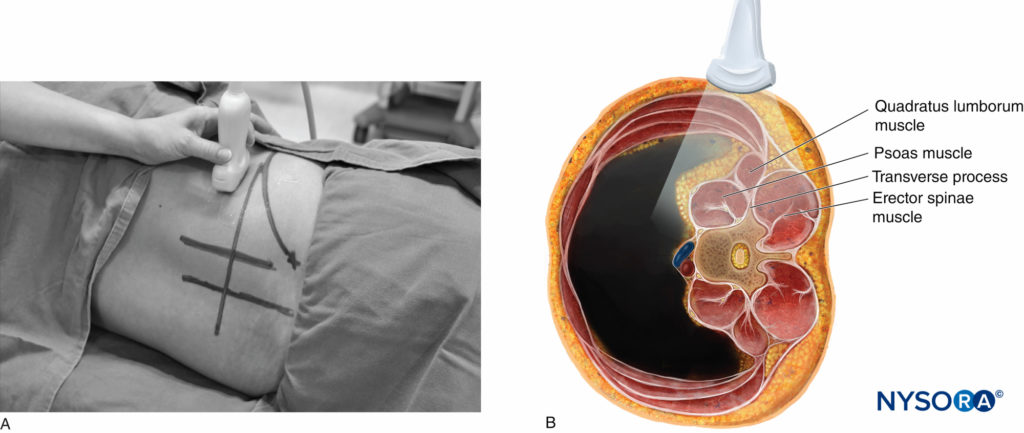
FIGURE 15. (A) Position of the patient (lateral decubitus) and US transducer during a transverse scan at the flank for the Shamrock method. (B) US transducer and plane of US beam superimposed onto a transverse anatomical section of the lumbar paravertebral region, illustrating how the US beam is insonated (axis of scan) and structures are visualized during the scan.
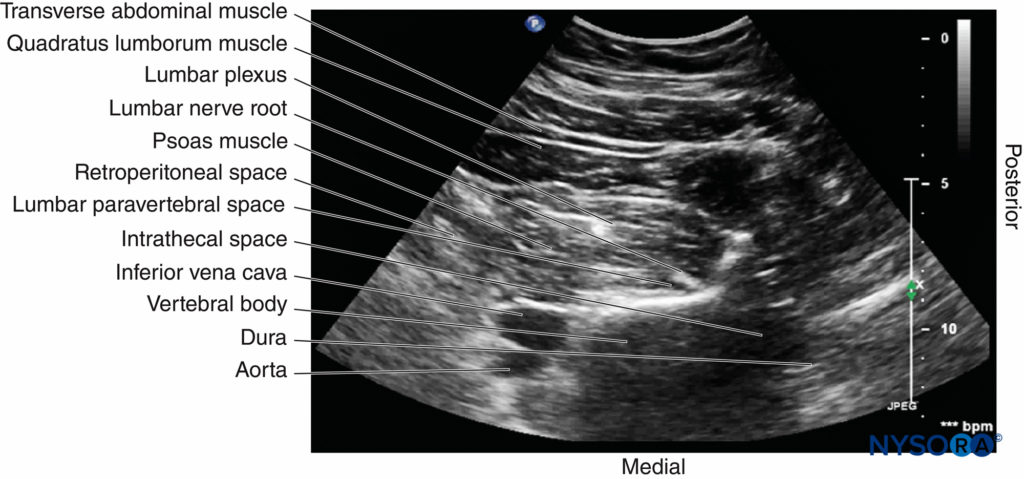
FIGURE 16. Transverse sonogram of the lumbar paravertebral region during the Shamrock method, with the US beam insonated at the level of the transverse process.
Sagittal Sonoanatomy
On a sagittal sonogram, the lumbar transverse processes are identified by their hyperechoic reflection and an anterior acoustic shadow (see Figures 11 and 12), which is typical of bone. The acoustic shadow of the transverse processes produces a sonographic pattern referred to as the “trident sign” (see Figures 11 and 12) because of its similarity in shape to a trident (in Latin, tridens or tridentis).
The psoas muscle is visualized through the acoustic window (see Figures 11 and 12) of the trident as multiple longitudinal hyperechoic striations against a hypoechoic background typical of muscle (see Figure 11). The lumbar plexus nerves are seen as longitudinal hyperechoic structures in the posterior aspect of the psoas muscle (see Figure 11) One should note that not all hyperechoic shadows or striations within the psoas muscle are nerves because the psoas muscle contains intramuscular tendons, which also produce hyperechoic shadows (Figure 20).
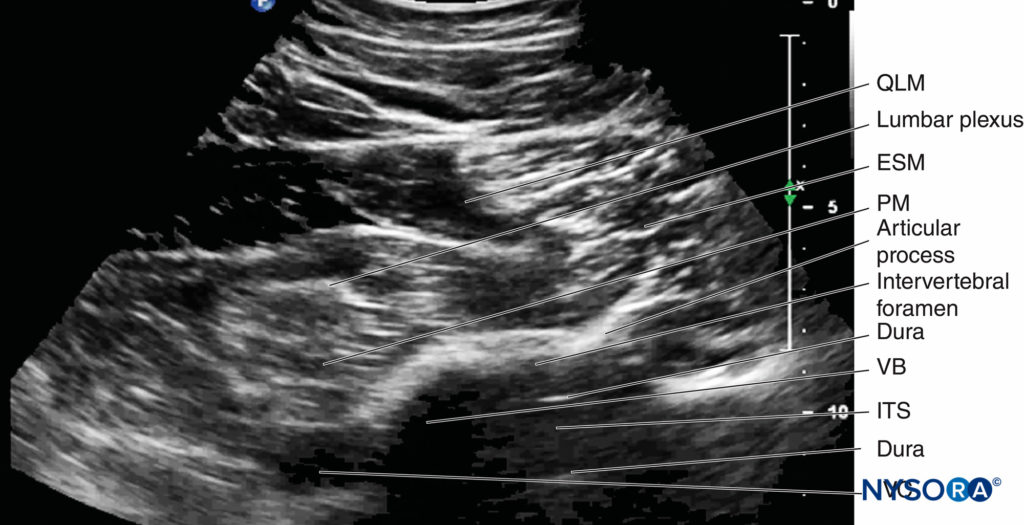
FIGURE 17. Transverse sonogram of the lumbar paravertebral region during the shamrock method, with the US beam insonated through the intertransverse space and at the level of the articular process of the vertebra. ESM, erector spine muscle; ITS, intrathecal space; IVC, inferior vena cava; PM, psoas muscle; QLM, quadratus lumborum muscle; VB, vertebral body.
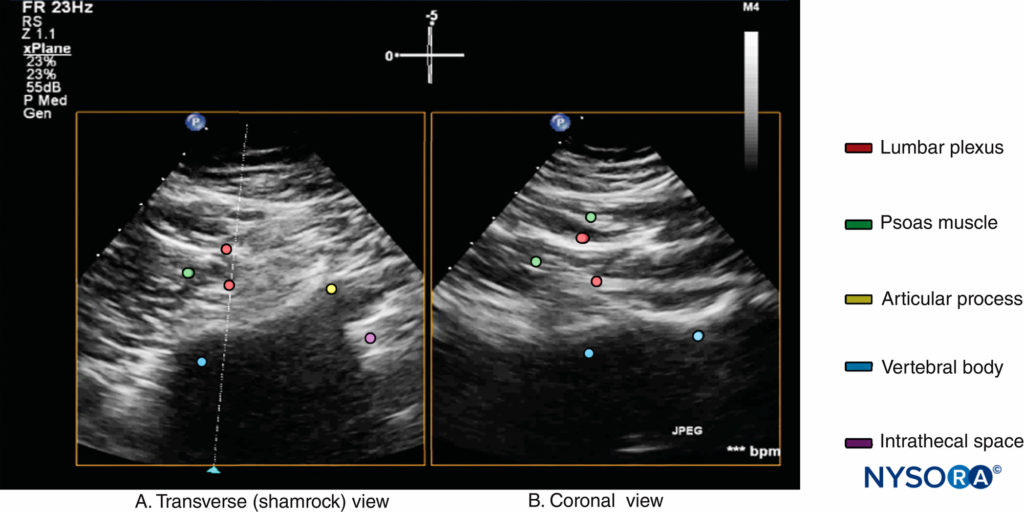
FIGURE 18. Biplanar US image of the lumbar paravertebral region obtained with the shamrock method, with the US beam insonated through the lumbar intertransverse space and at the level of the articular process. Note that the transverse axis (A) is the primary data acquisition plane and that the corresponding orthogonal image along the secondary data acquisition plane (dotted line with blue arrowhead in [a]) is a coronal view (B) showing the lumbar plexus nerves within the psoas muscle.
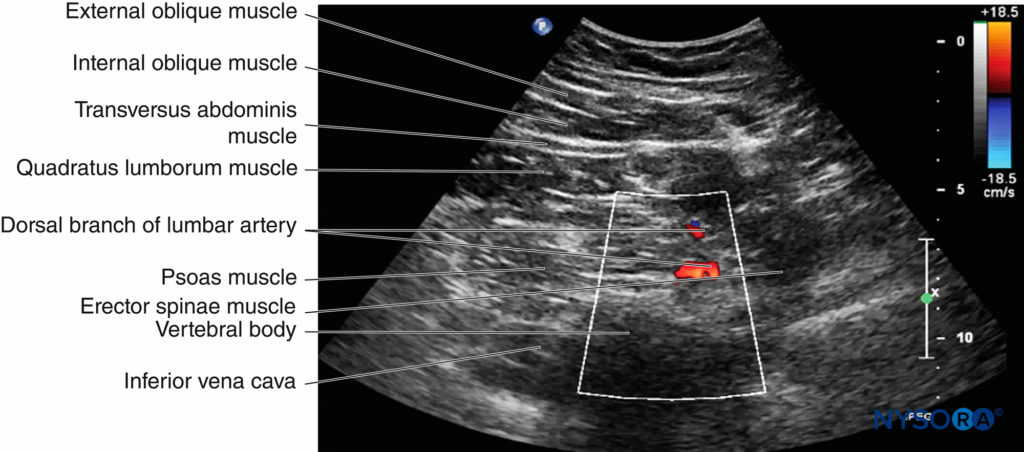
FIGURE 19. Color Doppler image of the lumbar paravertebral region obtained with the shamrock method. Note the Doppler signal in the posterior aspect of the psoas muscle from the dorsal branch of the lumbar artery.
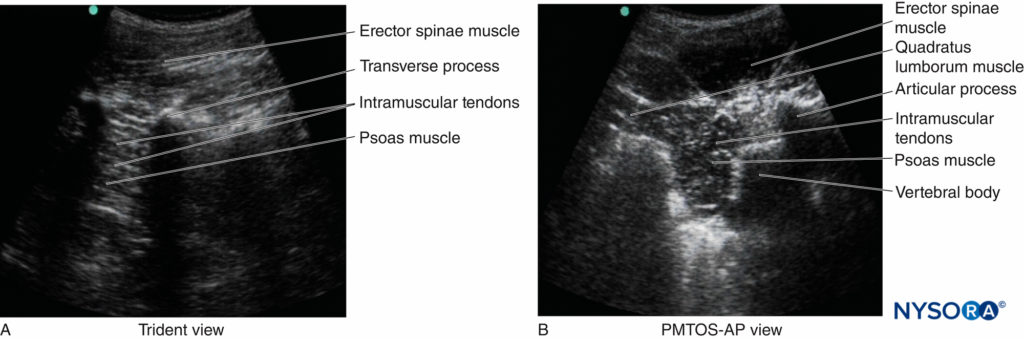
FIGURE 20. Sonograms showing intramuscular tendons within the psoas muscle. They are seen as (A) hyperechoic striations in a sagittal sonogram or (B) as multiple hyperechoic speckles in a transverse sonogram. PMTOS-AP, paramedian transverse oblique scan at the level of the articular process.
Nevertheless, the nerves of the lumbar plexus can be differentiated from the intramuscular tendons as they are thicker than the muscle fibers, take an oblique course through the psoas muscle (see Figure 11), and are better visualized after local anesthetic injection. A laterally positioned US transducer will produce a “suboptimal” sagittal sonogram without the US “trident,” but with the lower pole of the kidney, which lies anterior to the quadratus lumborum muscle and can reach the L3–L4 level in some patients.
Transverse Sonoanatomy
Kirchmair and colleagues were the first to describe the detailed transverse sonoanatomy of the lumbar paravertebral region relevant for LPB. However, they were unable to delineate the lumbar plexus in the cadavers and volunteers they examined, which they attributed to a loss of spatial resolution due to the use of low-frequency US. The author’s group has recently demonstrated that it is possible to accurately delineate the lumbar nerve root, lumbar paravertebral space, lumbar plexus, and psoas compartment using a paramedian transverse oblique scan (describe earlier).
On a typical PMTOS-TP (see Figure 10b), the erector spinae muscle, transverse process, psoas major muscle, quadratus lumborum muscle, and anterolateral surface of the vertebral body are clearly visualized (see Figure 13).
The psoas muscle appears hypoechoic, but multiple areas of hyperechogenicity are also interspersed within the central part of the muscle (see Figure 13). These hyperechoic speckles represent the intramuscular tendon fibers of the psoas muscle and are more pronounced below the level of the iliac crest.
The inferior vena cava (IVC; on the right side) and the aorta (on the left side) are also identified anterior to the vertebral body (see Figure 13) and are useful landmarks to look out for while performing a PMTOS. The lower pole of the kidney, which can extend to the L3–L4 level, is closely related to the anterior surfaces of the quadratus lumborum and psoas muscles and frequently seen as an oval structure that moves synchronously with respiration in the retroperitoneal space (Figure 21). The acoustic shadow of the transverse process obscures the posterior aspect of the psoas muscle during a PMTOS-TP (see Figure 13). Therefore, the lumbar nerve root and lumbar plexus are rarely visualized through the PMTOS-TP scan window. However, the spinal canal, with the dura and the intrathecal space, may be visualized during a PMTOS-TP (see Figure 13) due to the US signal entering the spinal canal through the interlaminar space (see Figure 13). Being able to visualize the neuraxial structures during a lumbar paravertebral scan may be useful in documenting epidural spread after an LPB.
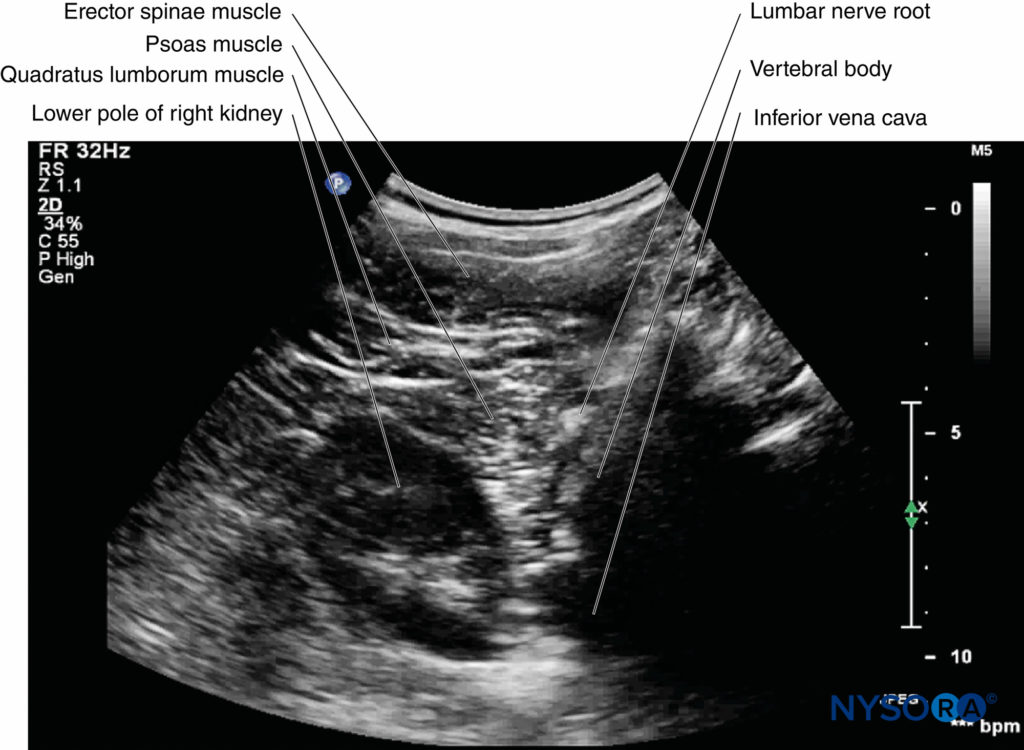
FIGURE 21. Paramedian transverse oblique scan of the right lumbar paravertebral region through the intertransverse space and at the level of the articular process (PMTOS-AP). The lumbar nerve root is seen emerging from the intervertebral foramen. Also note that the lower pole of the right kidney is seen anterior to the psoas muscle in this sonogram.
In contrast, during a PMTOS through the lumbar intertransverse space and at the level of the articular process (PMTOS-AP) (see Figure 10c), apart from the erector spinae, psoas, and quadratus lumborum muscles, the intervertebral foramen, articular process, and lumbar nerve root are clearly delineated (see Figure 14). The LPVS is also seen as a hypoechoic space adjacent to the intervertebral foramen (see Figure 14), and the lumbar nerve root can be seen exiting the foramen to enter the paravertebral space (see Figure 14).
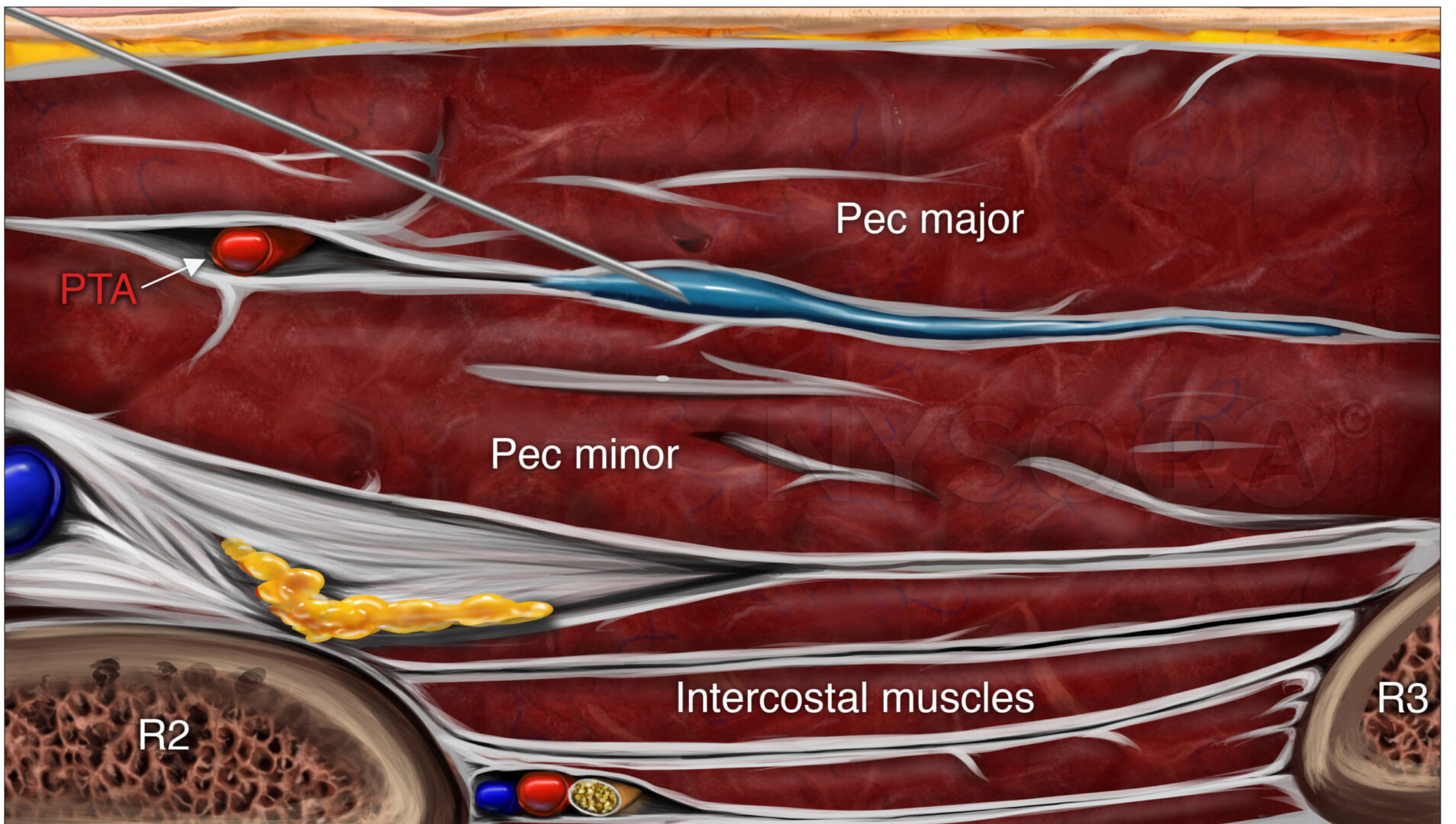
After it exits the intervertebral foramen, the lumbar nerve root does not enter the psoas muscle directly opposite the intervertebral foramen from which it emerges (see Figure 14), but takes a steep caudal course (see Figure 14), entering the psoas muscle at the vertebral level below to join the lumbar plexus. The lumbar plexus is seen as a separate hyperechoic structure within a hypoechoic space, the psoas compartment, in the posterior aspect of the psoas muscle (see Figure 14). In a transverse sonogram produced by the shamrock method (see Figure 15), the psoas, erector spinae, and quadratus lumborum muscles are also clearly visualized (see Figures 16, 17, 18 and 19). The anatomical arrangement of the three muscles around the transverse process—that is, the psoas muscle lying anteriorly, the erector spinae muscle lying posteriorly, and the quadratus lumborum muscle lying at the apex (see Figure 16)—produces a sonographic pattern that has been likened to the shape of a “shamrock,” with the muscles representing its three leaves. The lumbar nerve root may also be visualized close to the angle between the vertebral body and the transverse process (see Figure 16) and the lumbar plexus within the posterior aspect of the psoas muscle, typically about 2 cm anterior to the transverse process (see Figures 17 and 18). From this position, if the transducer is gently tilted caudally, the acoustic shadow of the L4 transverse process disappears, and the US beam is now insonated through the intertransverse space and at the level of the articular process of the L4 vertebra, similar to that seen with a PMTOS-AP (see Figure 17). As a result, apart from the psoas, erector spinae, and quadratus lumborum muscles, the intervertebral foramen and lumbar plexus may also be visualized (see Figure 17).
ULTRASOUND-GUIDED LUMBAR PLEXUS BLOCK
Although it is possible to define the anatomy relevant for LPB with both sagittal and transverse scans, it is not known which approach is best for USG LPB. Therefore, it is not possible to make recommendations of an optimal technique to use for USG LPB. The author believes that the paucity of data on USG LPB reflects only the greater degree of skill required to perform the US scan, interpret the sonograms, and perform the intervention, which is at a depth. Therefore, USG LPB should be considered an advanced-skill-level block and performed only after one has acquired the appropriate level of training and skill.
Furthermore, since it is not always possible to accurately delineate the lumbar plexus nerves within the psoas muscle in the US scans, it is prudent to use peripheral nerve stimulation in conjunction with US (dual guidance) for nerve localization during a USG LPB.
Ultrasound-Guided Lumbar Plexus Block Techniques
The following section briefly describes the various techniques used for USG LPB.
1. USG LPB Using the Trident View
As described above, a paramedian sagittal scan is performed with the patient in the lateral decubitus position, with the side to be blocked uppermost (see Figure 9 and 10). Once an optimal view of the lumbar US trident is obtained (Figure 22), an insulated nerve block needle, connected to a nerve stimulator, is inserted in plane from the caudal end of the US transducer (see Figure 22).
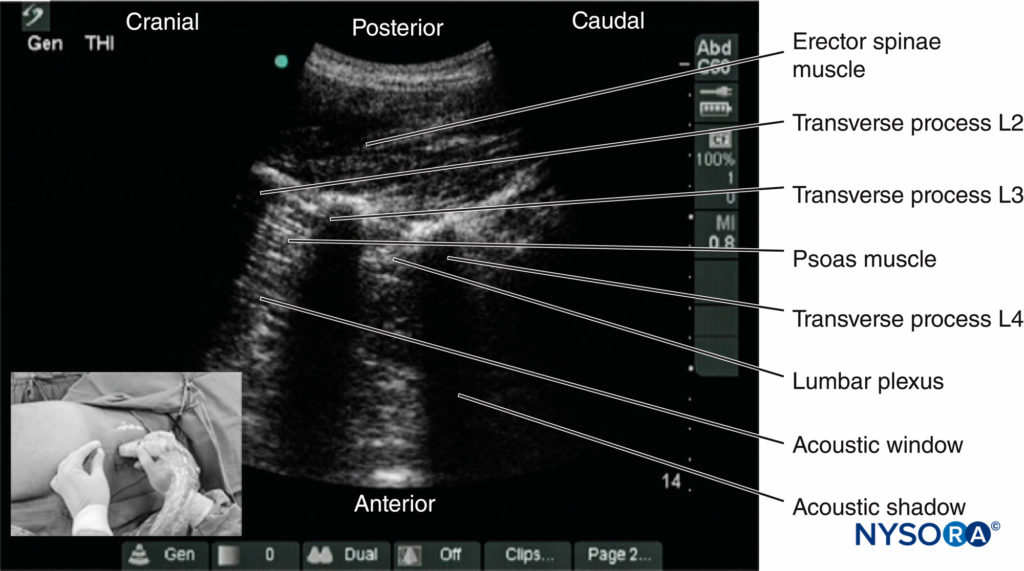
FIGURE 22. Sagittal sonogram of the lumbar paravertebral region showing the “trident” view. The psoas muscle is seen in the acoustic window between the transverse processes and is recognized by its typical striated appearance. Part of the lumbar plexus is also seen as a hyperechoic shadow in the posterior aspect of the psoas muscle between the transverse processes of the L3 and L4 vertebrae. The inset photograph shows the orientation of the US transducer and the direction in which the block needle is introduced (in plane) during a USG LPB via the trident view.
The aim is to guide the block needle through the acoustic window of the lumbar US trident; that is, through the space between the transverse process of L3 and L4 into the posterior aspect of the psoas major muscle until either needle–nerve contact is visualized or an ipsilateral quadriceps muscle contraction is elicited. After negative aspiration, an appropriate dose of local anesthetic (20–25 mL of 0.5% ropivacaine or levobupivacaine) is injected in aliquots over 2–3 minutes and the patient is closely monitored.
Spread of local anesthetic within the posterior aspect of the psoas muscle can be visualized in real time, and the nerves of the lumbar plexus are better visualized after the local anesthetic injection (see Figure 22).
2. USG LPB Using a Paramedian Transverse Scan
Originally described by Kirchmair and colleagues in cadavers, this technique involves performing a transverse scan of the lumbar paravertebral region to delineate the psoas major muscle (as described above) at the L3–L4 or L4–L5 level. It may be difficult to locate the psoas muscle at the L4–L5 level as the iliac crest interferes with transducer placement, particularly curved array transducers with a large footprint (60 mm). As described above, the author prefers to perform a PMTOS-AP with the patient positioned in the lateral position (Figure 23) since it provides better visualization of the anatomy relevant for LPB. Once an optimal PMTOS-AP view is obtained (see Figure 14), an insulated block needle, connected to a nerve stimulator, is inserted medially to the US transducer and in the plane of the US beam (in-plane technique) (Figure 23–24a).
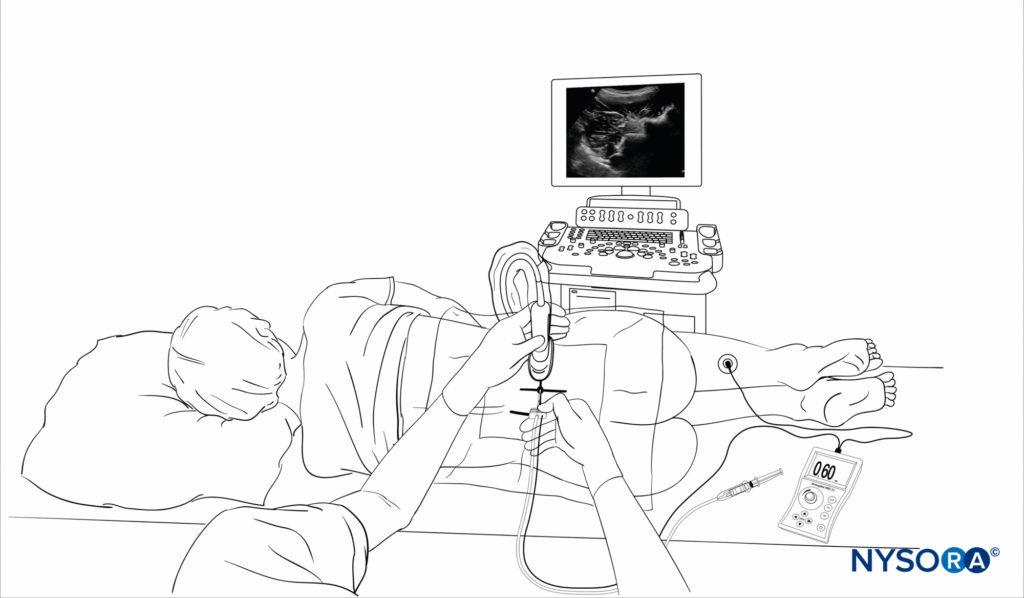
FIGURE 23. Position of the patient, anesthesiologist, US system, and US transducer orientation during a paramedian transverse oblique scan through the lumbar intertransverse space and at the level of the articular process.
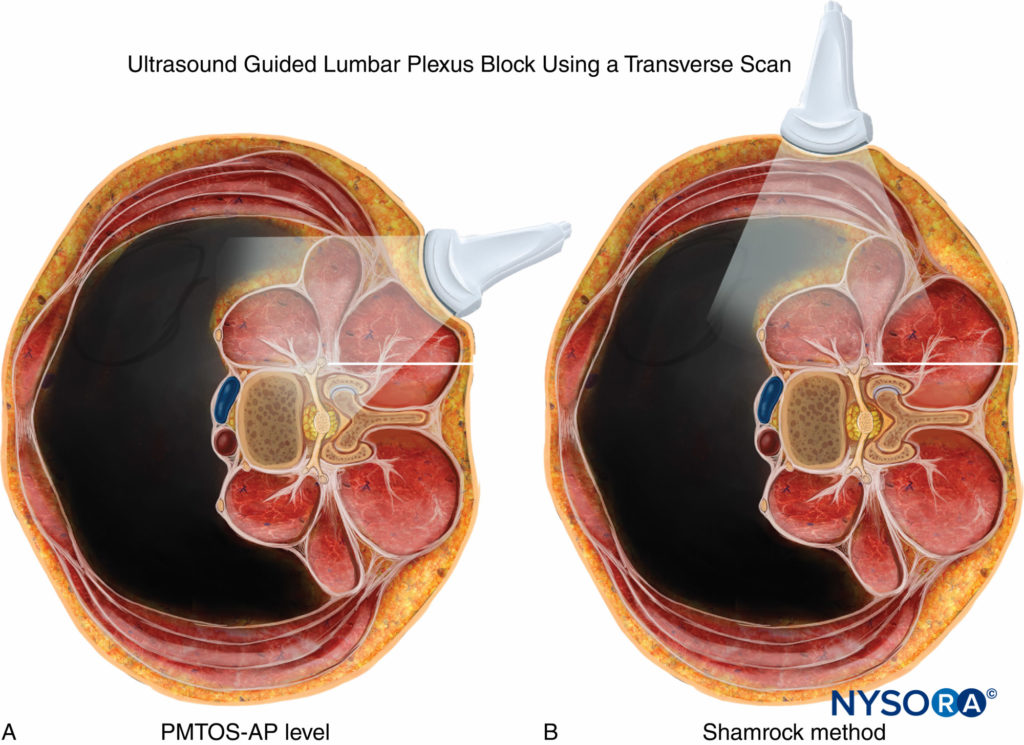
FIGURE 24. Position of the US transducer and the plane of the US beam, which has been superimposed on a transverse anatomical section (L4 vertebral level), rendered from the Visible Human Project® male dataset, illustrating the relevant lumbar paravertebral anatomy and how the US beam is insonated during (A) the paramedian transverse oblique scan at the level of the articular process (PMTOS-AP) and (B) the shamrock method. Note the relationship (in plane) of the nerve block needle to the US beam in both methods.
The point of needle insertion corresponds to a point 4 cm lateral to the midline and at the same location where one would insert the block needle during a landmark-based LPB (see Figure 23). The block needle is slowly advanced under real-time US guidance to the posterior aspect of the psoas muscle, and correct needle tip position is confirmed by observing needle–nerve contact (Figure 25) and/or an ipsilateral quadriceps muscle contraction (mostly the latter). There are also reports of the block needle being inserted from the lateral border of the US transducer and being advanced anteromedially in plane toward the psoas muscle from a lateral to medial direction.
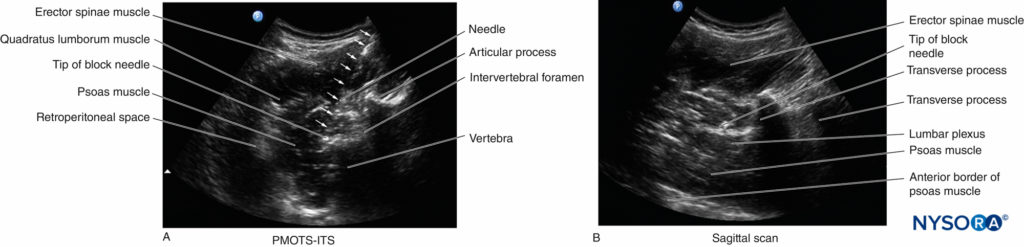
FIGURE 25. Sonograms of the lumbar paravertebral region showing the needle–lumbar plexus relationship when an ipsilateral quadriceps muscle contraction is elicited during a USG LPB. (A) Paramedian transverse oblique scan at the level of the articular process (PMTS-AP). (B) Sagittal sonogram in the same patient, validating the accuracy of the observation. Also note the direction of the in-plane needle insertion.
As described above, the lumbar plexus is not sonographically visualized in all patients but, when visualized, is seen as a hyperechoic structure in the posterior part of the psoas muscle (see Figure 25). Since the block needle is inserted in the plane of the US beam, it can be visualized and tracked in real time (see Figure 25). After negative aspiration, an appropriate dose of local anesthetic (20–25 mL of 0.5% ropivacaine or levobupivacaine) is injected in aliquots over 2–3 minutes and the patient is closely monitored (Figure 26). Occasionally, needle–nerve contact can be visualized on the US image during needle insertion or after the local anesthetic injection (see Figure 25). Also, the lumbar plexus is better visualized after the local anesthetic injection, as the hypoechoic local anesthetic surrounds the lumbar plexus nerves (Figures 26 and 27).
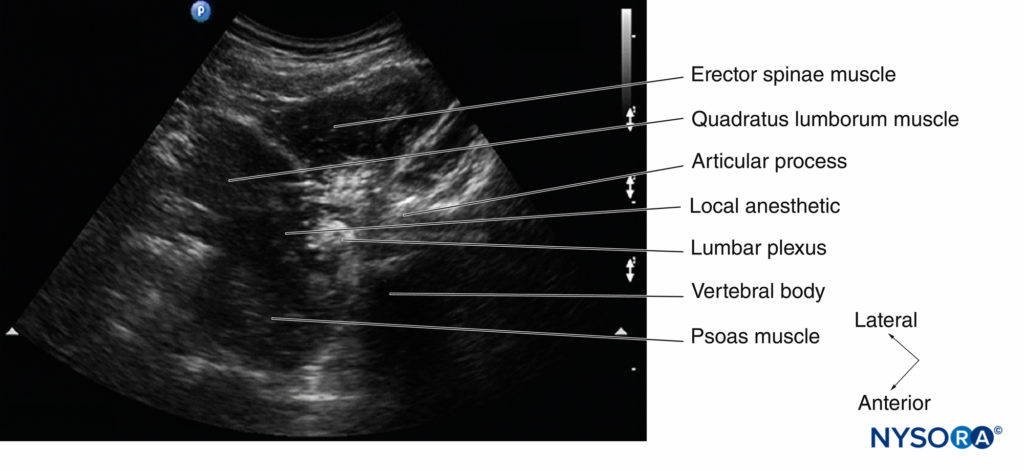
FIGURE 26. Transverse sonogram of the lumbar paravertebral region during a USG LPB and after local anesthetic (LA) injection. Note the spread of the LA relative to the lumbar plexus and the distention of the psoas compartment (short white arrows) by the LA.
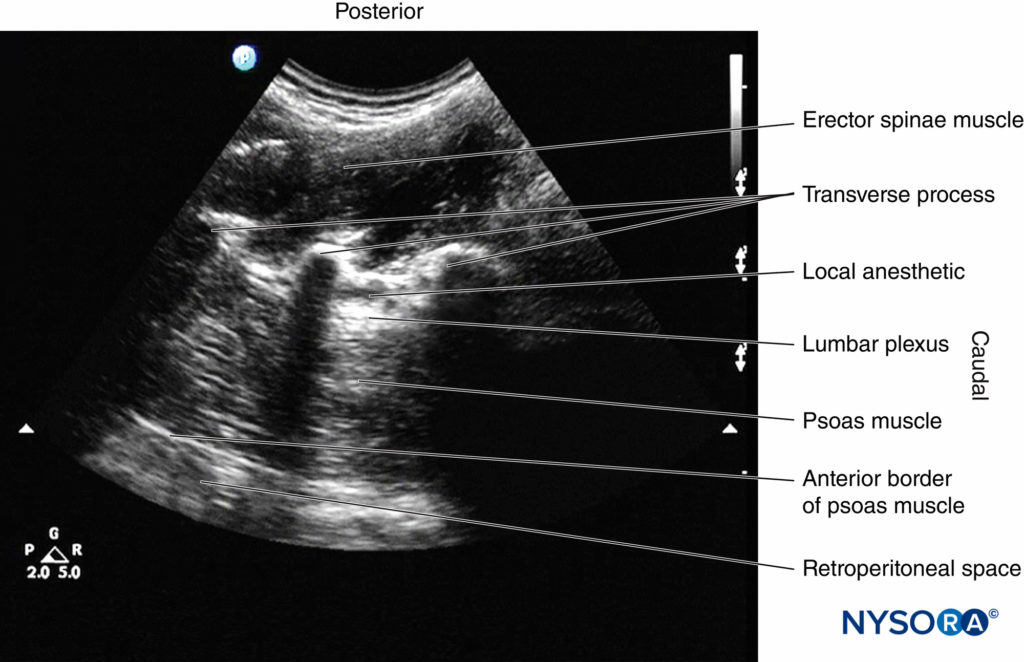
FIGURE 27. Sagittal sonogram of the lumbar paravertebral region during a USG LPB using the paramedian transverse oblique scan at the level of the articular process (PMTOS-AP) and after local anesthetic injection. Note the hyperechoic lumbar plexus nerve in the posterior aspect of the psoas muscle and the distribution of LA relative to the nerve (in front, behind, and in a craniocaudal direction) within the psoas compartment.
3. The Shamrock Method
Sauter and colleagues recently described an alternative approach for USG LPB, which they refer to as the “shamrock method (Figure 24b).” As described above, a transverse scan is performed at the flank and immediately above the iliac crest, with the patient in the lateral position and with the side to be blocked uppermost (see Figures 15a,b and 24b). Once the sonographic pattern of the “shamrock” is obtained at the level of the L4 transverse process (see Figure 16), the US transducer is tilted slightly caudally until the acoustic shadow of the transverse process is no longer visualized (see Figure 17).
This view represents the transverse view of the anatomy relevant for LPB through the L4–5 intertransverse space. A line is then drawn on the patient’s back extending from the center of the medial end of the IS transducer to the midline (back). A nerve block needle is inserted 4 cm from the midline along this line (Figure 28) and gradually advanced anteriorly under real-time US guidance (in-plane needle insertion; Figure 29a) until the needle tip is close to the L3 nerve root. Nerve stimulation should be used in conjunction with US to confirm correct needle placement, after which 20–30 mL of ropivacaine or levobupivacaine 0.5% is injected slowly while visualizing the perineural spread of the drug in the posterior aspect of the psoas muscle (Figure 29b).
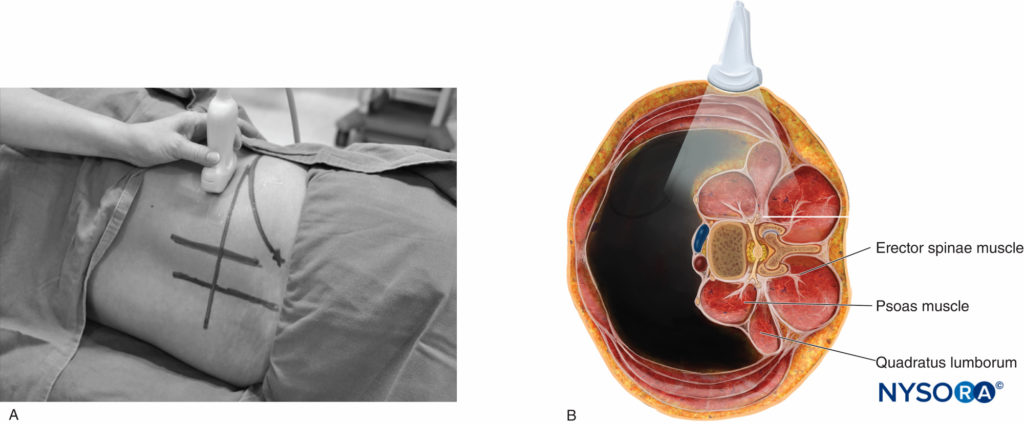
FIGURE 28. The shamrock method of US LPB. (A) Position of the patient (lateral decubitus), anesthesiologist, and US transducer and site and direction of needle insertion. (B) Simulated path of the block needle relative to the plane of the US beam (in plane) and paravertebral anatomy.
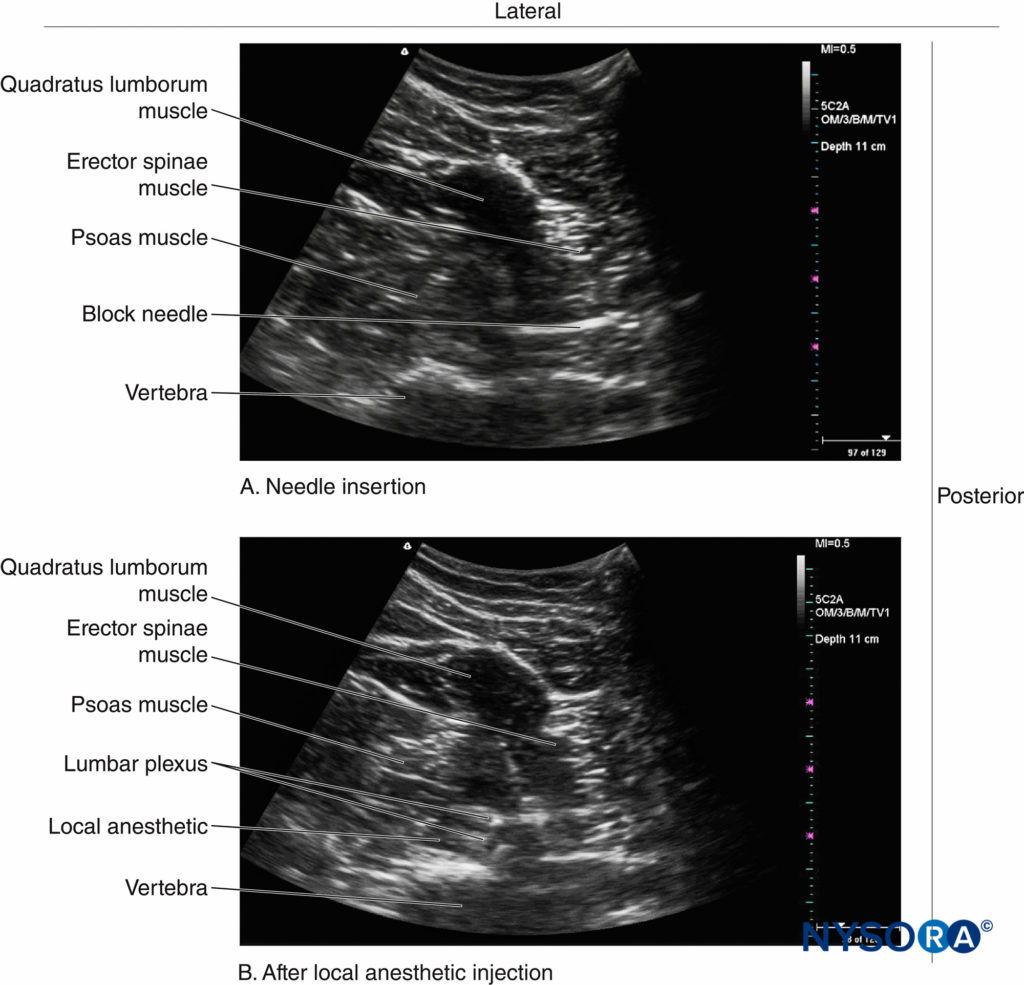
FIGURE 29. Transverse sonograms showing (A) the direction of needle insertion relative to the lumbar paravertebral anatomy and (B) the local anesthetic (LA) spread during a USG LPB using the shamrock method.
The technical challenge with this approach is that although the block needle is inserted in plane, visualizing the needle initially can be very challenging, since the sites for the US scan and needle insertion are separated by a considerable distance (see Figure 28). Nevertheless, with experience, needle visualization can be easily accomplished.
THE PEARLS AND PITFALLS OF ULTRASOUND-GUIDED LUMBAR PLEXUS BLOCK
The lumbar paravertebral region is highly vascular and contains the ascending lumbar veins and lumbar arteries, which can be visualized using color and power Doppler US (see Figures 7 and 19). There is also a rich network of blood vessels (arteries and veins) within the substance of the psoas major muscle including the psoas compartment. The dorsal branch of the lumbar artery is also closely related to the transverse processes and the posterior aspect of the psoas muscle (see Figure 7b), where the lumbar plexus is located.
Therefore, this blood vessel may be at risk of needlerelated injury during LPB because it is directly in the path of the advancing needle (see Figure 7). Considering the vascularity of the lumbar paravertebral region, it is not surprising that inadvertent intravascular injection of local anesthetic and psoas hematoma have been described after LPB. It is for the same reason that one must exercise caution when considering an LPB in patients with mild to moderate coagulopathy or in patients receiving thromboprophylaxis; based on our current understanding, such conditions may be considered a relative contraindication for LPB. That said, there are reports of the safe use of LPB (both the single-injection and continuous techniques) before the initiation of postoperative thromboprophylaxis and the removal of catheters in patients receiving thromboprophylaxis and/or aspirin with an international normalized ratio (INR) of equal to or greater than 1.5. One must exercise caution in interpreting such results, however, because the site at which an LPB is performed is noncompressible, and there are previous reports of retroperitoneal hematoma complicating LPB. Moreover, there are currently very few evidence-based indications for LPB.
The echo intensity (EI) of skeletal muscles is significantly increased in the elderly, and there is a strong correlation between the EI of muscles and age. Therefore, in US images, the lumbar paravertebral region in the elderly appears whiter and brighter than in younger patients, and there is also a loss of contrast between the muscle and the adjoining structures, making it more difficult to delineate the lumbar plexus. Therefore, USG LPB in the elderly can be very challenging. The same is also true in the obese, as excessive fat can make US imaging of the lumbar paravertebral anatomy and US guidance during LPB difficult. Gadsden and colleagues have also recently demonstrated that injection of local anesthetic under high pressure (> 20 psi) during a lumbar plexus block results in unwanted bilateral sensory motor block and a high incidence of neuraxial block. Therefore, one must ensure that the injection pressure is low (< 15 psi) during USG LPB. Occasionally, one may also find that during USG LPB, the needle tip is in the posterior aspect of the psoas muscle but no motor response is elicited. This may not be an uncommon phenomenon, considering that it is commonly seen during upper extremity blocks. However, one must ensure that the block needle has not been inadvertently inserted in the upper lumbar region because the upper lumbar nerves (L1 and L2) contribute predominantly to sensory nerves, and stimulating these nerves may not elicit a motor response.
SUMMARY
Recent advances in US technology, the image processing capabilities of US machines, and the development of new US scan protocols to image the lumbar paravertebral region have made it possible to image the anatomy relevant for lumbar plexus block. With US, one is able to preview the paravertebral anatomy, determine the safe depth for needle insertion, accurately guide the block needle to the target in real time, and visualize the distribution of the injected local anesthetic. These advantages may translate into improved accuracy, reduced needle-related complications, and improved success. It is also an excellent teaching tool for demonstrating the anatomy of the lumbar paravertebral region. However, the use of US for LPB is still in its infancy, and it is the author’s opinion that USG LPB is an advanced-skill-level block that should be performed only after one has acquired the necessary imaging and interventional skills.
Published data suggest that it is possible to image the anatomy relevant for LPB, and several USG LPB techniques have been described. Future research is warranted to define the role of US for LPB and to establish evidence-based indications for LPB.
Acknowledgements
Thanks to Dr. Jui-An Lin, M.D., Department of Anesthesiology, Taipei Medical University, Taiwan for sharing sonograms of the “Shamrock technique” from his archive (Figure 29). The cadaver anatomic sections are courtesy of the Visible Human Server at Ecole Polytechnique Fédérale de Lausanne, Visible Human Visualization Software (http://visiblehuman.epfl.ch), and Gold Standard Multimedia (www.gsm.org). The figures were reproduced with kind permission from www.aic.cuhk.edu.hk/usgraweb.
Continue reading: Sonography of the Lumbar Paravertebral Space and Considerations for the Ultrasound-Guided Lumbar Plexus Block
REFERENCES
- Parkinson SK, Mueller JB, Little WL, Bailey SL: Extent of block with various approaches to the lumbar plexus. Anesth Analg 1989;68: 243–248
- de Leeuw MA, Zuurmond WW, Perez RS: The psoas compartment block for hip surgery: the past, present, and future. Anesthesiol Res Pract 2011;2011:159541.
- Ilfeld BM, Mariano ER, Madison SJ, et al: Continuous femoral versus posterior lumbar plexus nerve blocks for analgesia after hip arthroplasty: a randomized, controlled study. Anesth Analg 2011;113: 897–903.
- Stevens RD, Van GE, Flory N, Fournier R, Gamulin Z: Lumbar plexus block reduces pain and blood loss associated with total hip arthroplasty. Anesthesiology 2000;93:115–121.
- Ho AM, Karmakar MK: Combined paravertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in a patient with severe aortic stenosis. Can J Anaesth 2002;49:946–950.
- Chayen D, Nathan H, Chayen M: The psoas compartment block. Anesthesiology 1976;45:95–99.
- Kirchmair L, Entner T, Wissel J, Moriggl B, Kapral S, Mitterschiffthaler G: A study of the paravertebral anatomy for ultrasound-guided posterior lumbar plexus block. Anesth Analg 2001;93:477–481.
- Farny J, Drolet P, Girard M: Anatomy of the posterior approach to the lumbar plexus block. Can J Anaesth 1994;41:480–485.
- Karmakar MK, Li JW, Kwok WH, Soh E, Hadzic A: Sonoanatomy relevant for lumbar plexus block in volunteers correlated with crosssectional anatomic and magnetic resonance images. Reg Anesth Pain Med 2013;38:391–397.
- Karmakar MK, Li JW, Kwok WH, Hadzic A: Ultrasound-guided lumbar plexus block using a transverse scan through the lumbar intertransverse space: a prospective case series. Reg Anesth Pain Med 2015;40:75–81.
- Kirchmair L, Lirk P, Colvin J, Mitterschiffthaler G, Moriggl B: Lumbar plexus and psoas major muscle: not always as expected. Reg Anesth Pain Med 2008;33:109–114.
- Capdevila X, Coimbra C, Choquet O: Approaches to the lumbar plexus: success, risks, and outcome. Reg Anesth Pain Med 2005;30: 150–162.
- Kirchmair L, Entner T, Kapral S, Mitterschiffthaler G: Ultrasound guidance for the psoas compartment block: an imaging study. Anesth Analg 2002;94:706–710.
- Aida S, Takahashi H, Shimoji K: Renal subcapsular hematoma after lumbar plexus block. Anesthesiology 1996;84:452–455.
- Aveline C, Bonnet F: Delayed retroperitoneal haematoma after failed lumbar plexus block. Br J Anaesth 2004;93:589–591.
- Weller RS, Gerancher JC, Crews JC, Wade KL: Extensive retroperitoneal hematoma without neurologic deficit in two patients who underwent lumbar plexus block and were later anticoagulated. Anesthesiology 2003; 98:581–585.
- Karmakar MK, Ho AM, Li X, Kwok WH, Tsang K, Kee WD: Ultrasound-guided lumbar plexus block through the acoustic window of the lumbar ultrasound trident. Br J Anaesth 2008;100:533–537.
- Doi K, Sakura S, Hara K: A modified posterior approach to lumbar plexus block using a transverse ultrasound image and an approach from the lateral border of the transducer. Anaesth Intensive Care 2010;38: 213–214.
- Sauter AR, Ullensvang K, Bendtsen TF, Boerglum J: The “Shamrock Method”—a new and promising technique for ultrasound guided lumbar plexus blocks [letter]. Br J Anaesth February 26, 2013. http://bja.oxfordjournals.org/forum/topic/brjana_el%3B9814. Accessed July 6, 2015.
- Bendtsen TF, Pedersen EM, Haroutounian S, et al: The suprasacral parallel shift vs lumbar plexus block with ultrasound guidance in healthy volunteers—a randomised controlled trial. Anesthesia 2014;69: 1227–1240.
- Morimoto M, Kim JT, Popovic J, Jain S, Bekker A: Ultrasound-guided lumbar plexus block for open reduction and internal fixation of hip fracture. Pain Pract 2006;6:124–126.
- Madison SJ, Ilfeld BM, Loland VJ, Mariano ER: Posterior lumbar plexus perineural catheter insertion by ultrasound guidance alone. Acta Anaesthesiol Scand 2011;55:1031–1032.
- Chin KJ, Karmakar MK, Peng P: Ultrasonography of the adult thoracic and lumbar spine for central neuraxial block. Anesthesiology 2011;114:1459–1485.
- Karmakar MK, Li X, Ho AM, Kwok WH, Chui PT: Real-time ultrasound-guided paramedian epidural access: evaluation of a novel in-plane technique. Br J Anaesth 2009;102:845–854.
- Karmakar MK, Li X, Kwok WH, Ho AM, Ngan Kee WD: Sonoanatomy relevant for ultrasound-guided central neuraxial blocks via the paramedian approach in the lumbar region. Br J Radiol 2012;85:e262–e269.
- Klein SM, d’Ercole F, Greengrass RA, Warner DS: Enoxaparin associated with psoas hematoma and lumbar plexopathy after lumbar plexus block. Anesthesiology 1997;87:1576–1579.
- Chelly JE, Schilling D: Thromboprophylaxis and peripheral nerve blocks in patients undergoing joint arthroplasty. J Arthroplasty 2008;23:350–354.
- Chelly JE, Szczodry DM, Neumann KJ: International normalized ratio and prothrombin time values before the removal of a lumbar plexus catheter in patients receiving warfarin after total hip replacement. Br J Anaesth 2008;101:250–254.
- Li X, Karmakar MK, Lee A, Kwok WH, Critchley LA, Gin T:Quantitative evaluation of the echo intensity of the median nerve and flexor muscles of the forearm in the young and the elderly. Br J Radiol 2012;85:e140–e145.
- Gadsden JC, Lindenmuth DM, Hadzic A, Xu D, Somasundarum L, Flisinski KA: Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology 2008;109: 683–688.