Laura Clark
INTRODUCTION
The infraclavicular brachial plexus block provides a block of the arm below the shoulder. Unlike the axillary approach, it can be performed without abduction of the arm, making it useful for patients with limited shoulder mobility. It is amenable to continuous catheter placement by being more accessible and more comfortable for a catheter than the axilla. Georg Hirschel, in 1911, is considered to have carried out the first percutaneous axillary block because he approached the plexus from the axilla. His goal was to place the local anesthetic on top of the first rib via the axilla. He discovered after his own dissections of the plexus the reason for incompleteness of the axillary block, and was the first to describe that the axillary and musculocutaneous nerves separated from the plexus much higher than in the axilla. However, the needles in the early 1900s were not long enough to reach this area to block those nerves.
To remedy this problem in 1911, Diedrich Kulenkampff’s supraclavicular description was soon to follow. He felt his technique was safer and more accurate than Hirschel’s, but after initial success, the reports of complications of pneumothorax ensued. In 1914, Bazy described injecting below the clavicle just medial to the coracoid process along a line connecting with the Chassaignac tubercle. The needle trajectory was pointed away from the axilla, close to the clavicle, and was felt to present little chance of pleural damage. Several modifications occurred in the ensuing 8 years. Babitszky said that “to discuss the anatomical relationship and the technique more fully would be superfluous, as it is customary to familiarize oneself with the anatomy of the field in question on the cadaver any time one tends to use an unfamiliar technique.” Gaston Labat, in 1922, essentially redescribed Bazy’s technique in his textbook, Regional Anesthesia, as did Achille Dogliotti in 1939. However, the technique seemed to fade into obscurity. For instance, infraclavicular block was not included in Daniel Moore’s Regional Block in 1981 or Michael Cousins and Phillip Bridenbaugh’s Neural block in Clinical Anesthesia and Pain Management.
Prithvi Raj is credited with reintroducing the approach in 1973 with modification from the earlier descriptions. He described the initial entry point at the midpoint of the clavicle and directed the needle laterally toward the axilla using a nerve stimulator. His data suggested a virtual absence of risk of pneumothorax with the technique. and a more complete block of musculocutaneous and the ulnar nerves. However, these results were not reproducible in other practitioner’s clinical practice. Kurt Whiffler, in 1981, described what is commonly referred to today as the coracoid block. The injection site was very close to that detailed by Sims, but Whiffler felt that the shoulder should be depressed with the head turned to the opposite side and the arm abducted 45 degrees from the chest wall to make the plexus closer to the coracoid process. To estimate the depth of the plexus one identifies two points. One is the point past the midpoint of the clavicle where the subclavian pulse disappears. The second point is found by determining the highest pulse of the artery in the axilla and placing the thumb of the same hand on the anterior surface of the chest wall that corresponds to that point. Those points are connected, and the needle is then inserted inferior and medial to the coracoid process on that line to the depth that the plexus has been estimated. Whiffler did not use a nerve stimulator because he felt “this simpler approach does not require a nerve stimulator.” Incremental injections were used to a total volume of 40 mL, withdrawing the needle 1 cm one to two times.
In 1983, Alon Winnie’s book, Plexus Anesthesia, describes several infraclavicular approaches including the techniques of Raj (1973), Sims (1977), and Whiffler (1981), although it does not devote a section to infraclavicular block. He states that “none of the infraclavicular techniques appears to offer significant advantages over the more established perivascular techniques …,” and documents once again that the sheath can be entered at any level. The Infraclavicular block gained popularity in the 1990s along with the upsurge of regional anesthesia. Oivind Klaastad, in 1999, performed a magnetic resonance imaging (MRI) study and determined that if followed exactly as described, the needle was not in close proximity to the cords. In a significant number of cases the cords were caudad and posterior to the target. Furthermore, the needle trajectory’s shortest distance to the pleura was only 10 mm, and in one case hit the pleura. Klaastad concluded that a more lateral approach would make it more precise and reduce the risk of complications. This was actually what Raj had found clinically and was suggesting in lectures, but had not published. He had changed the point of needle insertion to be on a line between the pulsation of the subclavian and brachial artery and 2.5 cm from this line, crossing with the inferior border of the clavicle. This is what is commonly referred to as the modified Raj approach Four approaches will be described in this chapter: (1) vertical infraclavicular block as described by Kilka and colleagues, (2) the coracoid approach described by Whiffler11 and modified by Wilson and coworkers, (3) the modified Raj approach, and (4) the lateral and sagittal approach described by Klaastad and associates often used for ultrasound.
INDICATIONS AND CONTRAINDICATIONS
NYSORA Tips
- Distribution of anesthesia consists of the hand, wrist, forearm, elbow, and most of the upper arm.
- Indications are similar to those for axillary block; hand, forearm, elbow, and arteriovenous fistula surgery.
- This approach affords greater applicability due to greater coverage and obviates the need for special arm positioning (abduction).
Indications for infraclavicular block are the same as for axillary block but complete anesthesia of the arm is obtained from the lower shoulder to the hand, making it applicable for any surgery up to but not including the shoulder. A tourniquet is well tolerated without supplementation of the intercostobrachial nerve. Bilateral blocks can be carried out without fear of blocking the phrenic nerve. The coracoid process and clavicle landmarks are easily palpable even in obese patients. The technique is also conducive to continuous catheter placement and long-term infusion. Other than the obligatory contraindications of infection at or near the site or existing coagulopathy, there are no block specific contraindications to infraclavicular block. Coagulopathy is a relative contraindication and based on the risk-vs-benefit ratio.
FUNCTIONAL ANATOMY
NYSORA Tips
- Block occurs at the level of the cords of the brachial plexus below the clavicle.
- Three cords surround the axillary artery.
- The anatomy of the brachial plexus is complex in this area and variability exists.
- The lateral cord is the most superficial, the posterior cord is encountered next, the medial cord is the deepest and is below the axillary artery.
- The lateral cord and the medial cord each contain half of the median nerve.
- The posterior cord contains all of the radial nerve.
- The musculocutaneous nerve is often outside but very close to the lateral cord.
The pertinent anatomy is illustrated in Figure 1. Divisions exist as the brachial plexus crosses the first rib into the infraclavicular area. They originate from the trunks and divide into anterior and posterior divisions, thus, the origin of the name division. The anterior divisions usually supply flexor muscles (which are most often positioned anterior) and posterior divisions usually supply extensor muscles (which are generally posterior). The brachial plexus makes most of its major changes in the infraclavicular area in just a few centimeters as it twists and turns from a parallel course in the neck to circumferentially surround the axillary artery in the infraclavicular area and progresses into the axilla as terminal nerves. Mixing of the nerves occurs, and its organization can be quite complex. Figure 2 shows the course of the brachial plexus from the interscalene to the infraclavicular area. The anatomic terms for the cords are based with the body in anatomic position and relative to its center; this is not how the brachial plexus is encountered clinically. Many textbooks feature two-dimensional rather than three-dimensional diagrams of the plexus in this area, which contributes to the confusion. However, a solid understanding of the three-dimensional organization of the plexus is perhaps the most important factor in its successful block.
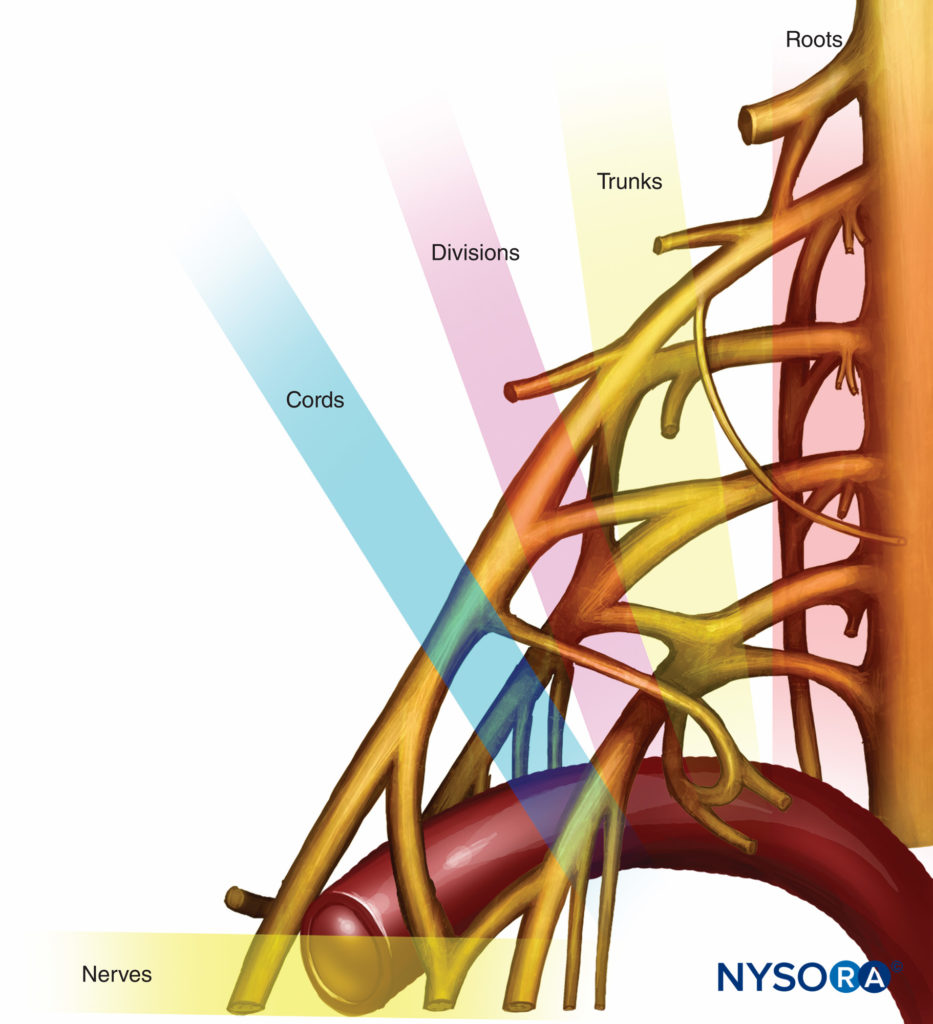
FIGURE 1. Organization of the brachial plexus.
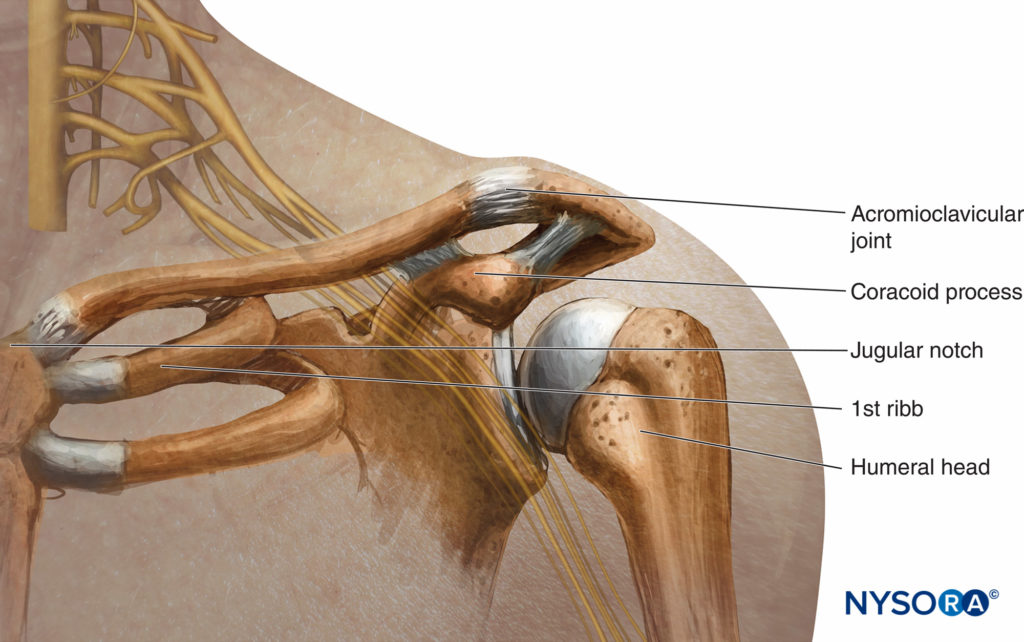
FIGURE 2. Relationship of the brachial plexus, clavicle, and coracoid process.
Divisions, Branches, Cords, and Terminal Nerves
The anterior divisions of the upper (C5 and C6) and middle trunk (C7) unite to form the lateral cord, which lies lateral to the axillary artery and most superficial to the anterior chest. The anterior divisions of the lower trunk (C8 and T1) form the medial cord. It lies medial to the axillary artery and is the deepest from the chest wall. The posterior cord is formed from all of the posterior divisions (C5 through T1) and lies posterior to the artery just under the lateral cord. The cords end in terminal branches that are mixed nerves, which contain both sensory and motor components. They are the musculocutaneous, ulnar, median, axillary, and radial branches. Other branches also exit the plexus prior to the formation of the terminal nerves. They are not mixed and are unique in that they are either sensory or motor nerves. These nerves are often not addressed but are important because the motor branches can be stimulated during the performance of a block and knowing where they originate will help determine where to locate the tip of the needle. Tables 1 and 2 list the branches of the brachial plexus and their innervation.
TABLE 1. Branches of brachial plexus.
| Motor Innervation | Motion Observed | Sensory Innervation | |
|---|---|---|---|
| Lateral | |||
| Lateral pectoral nerve | Pectoralis major | Contraction of pectoralis | |
| Dorsal scapular nerve | Rhomboid major and minor; levator scapulae | Adducts and rotates shoulder, raises scapula | |
| Posterior | |||
| Upper subscapular | Subscapularis (superomedial part) | Medial rotation or arm | |
| Thoracodorsal | Latissimus dorsi | Abduction of arm | |
| Lower subscapular | Subscapularis (lateral part), teres major | Internal rotation, adduction of shoulder | |
| Axillary | Deltoid, teres minor | Elevation of upper arm | Skin of upper lateral arm |
| Medial | |||
| Medial pectoral | Pectoralis minor and major | Contraction of pectoralis | |
| Medial cutaneous nerve of arm | Skin of medial side or arm |
||
| Medial cutaneous nerve of forearm | Skin of medial side or forearm |
TABLE 2. Terminal nerves of brachial plexus.
| Motor Innervation | Motion Observed | Sensory Innervation | |
|---|---|---|---|
| Lateral | |||
| Musculocutaneous | Coracobrachialis, biceps brachii, brachialis | Flexion of elbow | Skin of lateral side of forearm |
| Median | Flexor digitorum superficialis— all, pronator teres, flexor carpi radialis palmaris longus | Flexion of first fingers, opposition of thumb | Skin of radial half of palm and palmer side of radial three and a half digits |
| Posterior | |||
| Radial | Brachioradialis, abductor pollicis longus, extensor muscles of the wrist and fingers | Abduction of thumb, extension of wrist and fingers | Skin of posterior arm, forearm and hand |
| Medial | |||
| Ulnar | Abductor pollicis interossei intrinsic muscles of the hand | Contraction of the 4th and 5th fingers and thumb abduction | Skin of medial side of wrist and hand and ulner one and a half digits |
| Median | Flexor digitorum superficialis— all, pronator leres, flexor carpi radialis palmaris longus | Flexion of first 31/2 fingers, opposition of thumb | Skin of radial half of palm and palmer side of radial three and a half digits |
Note: All branches from the medial cord carry C8 and T1 fibers, and that of the higher spinal segments in the brachial plexus (C5 through C6) tend to innervate muscles more proximal on the upper extremity, whereas the lower segments (C8, T1) tend to innervate more distal muscles, such as those in the hand (T1). Anatomic variation and the comingling of fibers from both lateral and medial cords makes it impossible to tell with certainty which cord is being stimulated with distal median nerve response.
CLINICAL ANATOMY
A simplified schematic diagram of the plexus is shown in Figure 1. This diagram depicts the plexus as it actually exists and a more clinical representation of how it is encountered when performing infraclavicular block. As shown, the posterior cord is not actually the most posterior cord but instead lies between the lateral and medial cords. The most helpful anatomic picture is in the sagittal plane, as shown in Figure 3. This figure illustrates the brachial plexus at the level of infraclavicular block to show this relationship. The relationship shown in Figure 3 is helpful for guiding needle placement while performing this block. The sagittal view shown here illustrates the cords in a close-up view surrounding the artery.
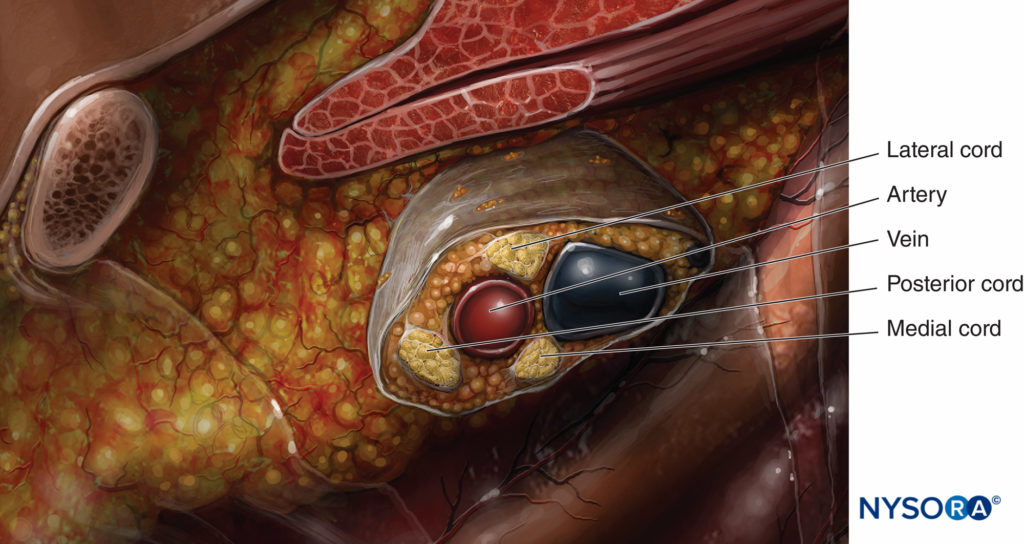
FIGURE 3. Close-up view of the relationship of the cords of the brachial plexus at the level of infraclavicular block to the subclavian/axillary artery.
Once this relationship is learned, the ability to change the needle directions for correct positioning is based on anatomy, and the need for subsequent passes to achieve successful placement lessens. The cord that is most often encountered first when performing the infraclavicular block is the lateral cord because it is the most superficial. Just beyond the lateral cord is the posterior cord, which is in close proximity but just a bit deeper than the lateral cord. The medial cord is actually caudal or below the axillary artery, as can be seen in the sagittal view in Figure 3. The schematic diagram of the cord shown in Figure 4 demonstrates the 90-degree angle of needle insertion for the lateral and posterior cord. This figure also illustrates the proximity of the artery and the risk of puncturing the artery when attempting to encounter the medial cord. The anatomy of the plexus varies widely among individuals. The MRI study of Sauter revealed that the cords are found within 2 cm from the center of the artery, approximately within two-thirds of a circle Figure 5.
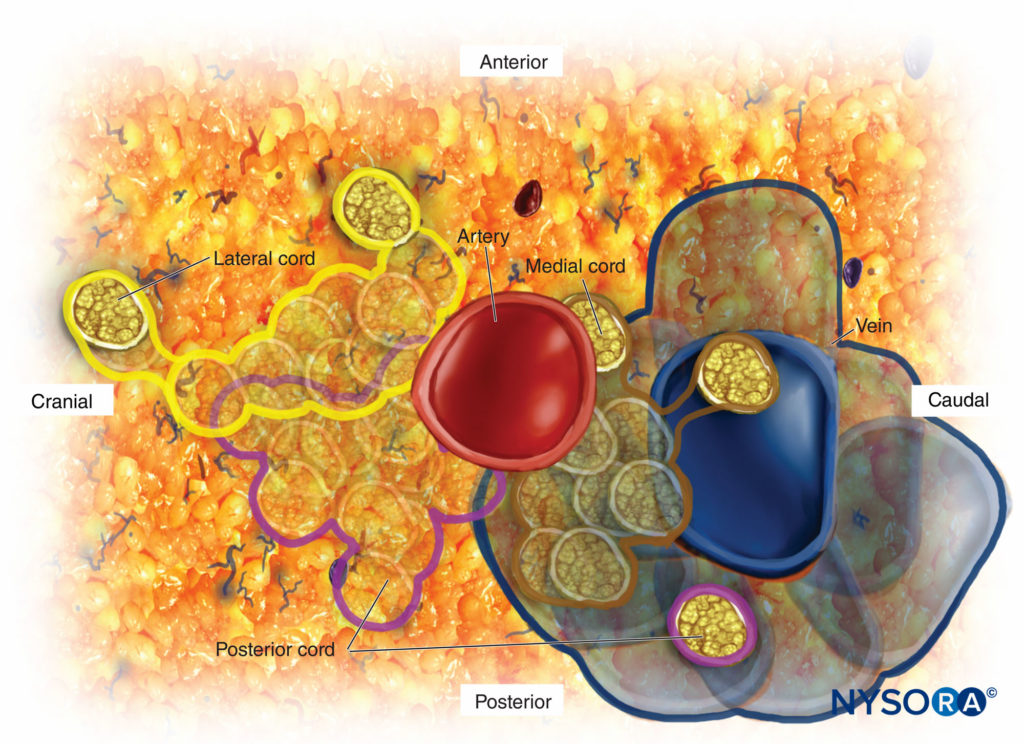
FIGURE 4. Schematic of the relationship of the cords of the brachial plexus to the subclavian/axillary artery.
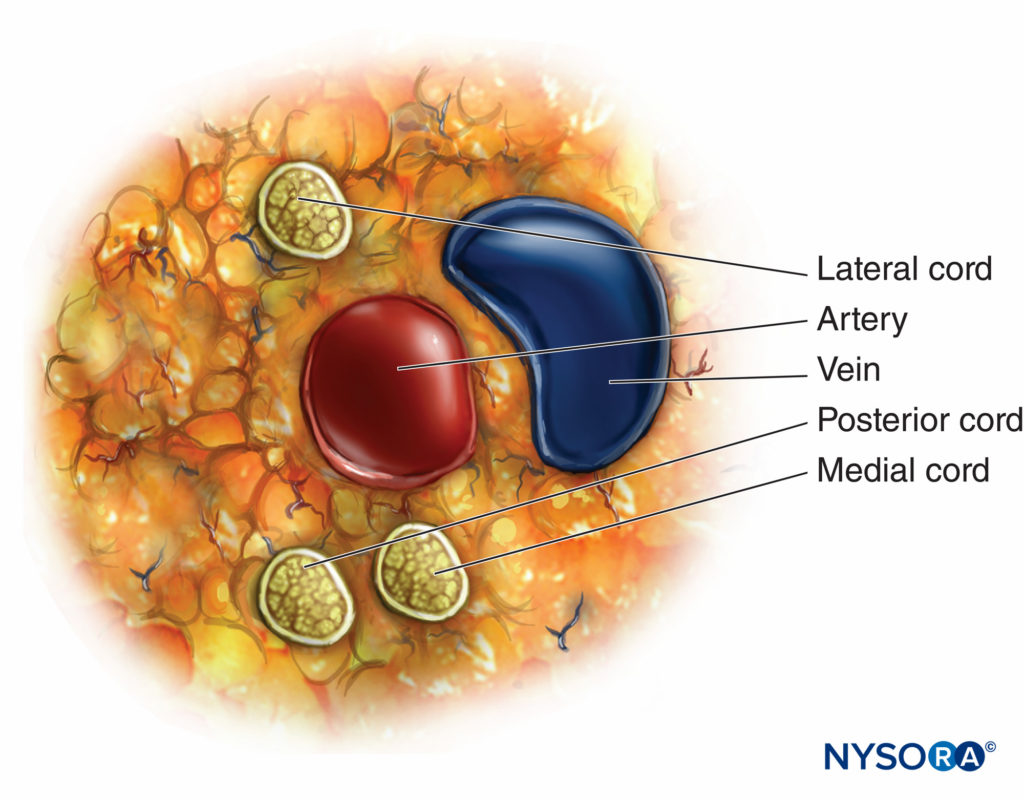
FIGURE 5. Anatomic variations of the infraclavicular brachial plexus among individuals.
The Lateral Cord
The lateral cord supplies the lateral half of the median nerve and the musculocutaneous and the pectoral nerve branches (see Tables 1 and 2). This lateral portion of the median nerve is the motor innervation to the flexor muscles in the forearm, flexor carpi radialis, pronator teres (pronation of the forearm), and the thenar muscle of the thumb. It provides sensory innervation for the thumb to the lateral half of the fourth finger including the dorsal tips. The most distal motor response would be flexion of the fingers or flexion and opposition of the thumb. The thumb has motor innervation from the ulnar nerve as well, which may be confusing if trying to interpret isolated thumb twitch. The ulnar nerve supplies the adductor pollicis, flexor pollicis brevis, and the first dorsal interosseous muscle. These muscles radially adduct the thumb. The flexor pollicis brevis assists in opposition of the thumb. The median nerve’s innervation of the flexor pollicis longus, abductor pollicis brevis, and the opponens pollicis are the major flexors for opposition of the thumb.
The musculocutaneous nerve has only muscular branches above the elbow and is purely sensory below the elbow as it becomes the lateral antebrachial cutaneous nerve. The motor response is flexion of the elbow by contraction of the biceps and sensation to the middle to median part of the forearm. The anatomic relationship of the musculocutaneous nerve to the cords and the coracoid process is pertinent to infraclavicular block. It could be considered a branch because it exits early, but it is more like a terminal nerve because it has sensory and motor innervations. Variations in brachial plexus anatomy are common. Because the musculocutaneous nerve most often exits the lateral cord quite early, the stimulation of this nerve is felt to be an unreliable indicator of stimulation of the lateral cord. It often overlies the lateral cord, which will be stimulated with deeper advancement of the needle as it passes the point of musculocutaneous nerve stimulation. Figure 6 depicts the lateral cord with its stimulated hand motor response.
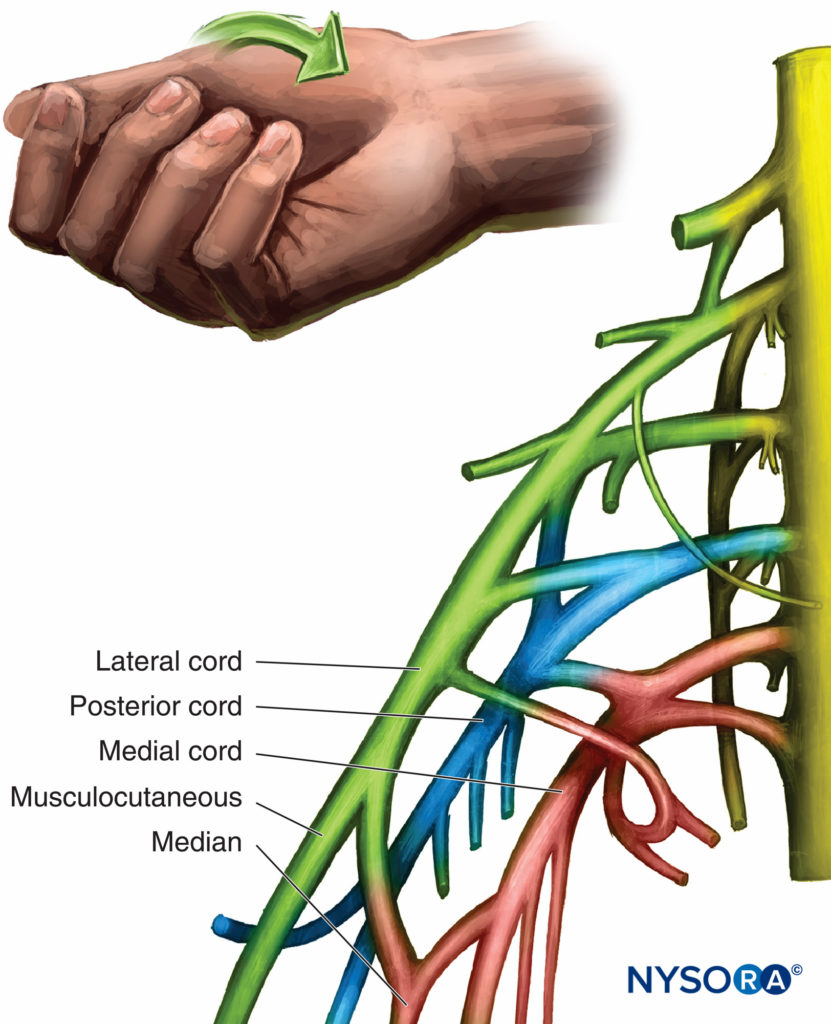
FIGURE 6. Organization and motor response of the lateral cord.
The Posterior Cord
The posterior cord is just deep or inferior to the lateral cord. The axillary, the thoracodorsal, and upper and lower subscapular nerves are the branches from the posterior cord. They are involved in upper arm movement and shoulder movement and rotation as well as adduction of the shoulder and abduction of the arm. The branch most often encountered is the axillary nerve because it often has separated from the cord prior to the coracoid process. The axillary nerve to the deltoid elevates the upper arm. In addition to its branches, the posterior cord is responsible for the complete radial nerve. The distal responses from stimulation are abduction of the thumb and extension of the wrist and fingers (Figure 7). The brachioradialis muscle is innervated by the radial nerve and is classified as an extensor. Its stimulation should be characterized because it may be confused as a median nerve response because it actually flexes the elbow joint. Elbow flexion with radial deviation of the wrist represents stimulation of the brachioradialis muscle and a posterior cord response. The needle should be readjusted to obtain a more distal response of the radial nerve.
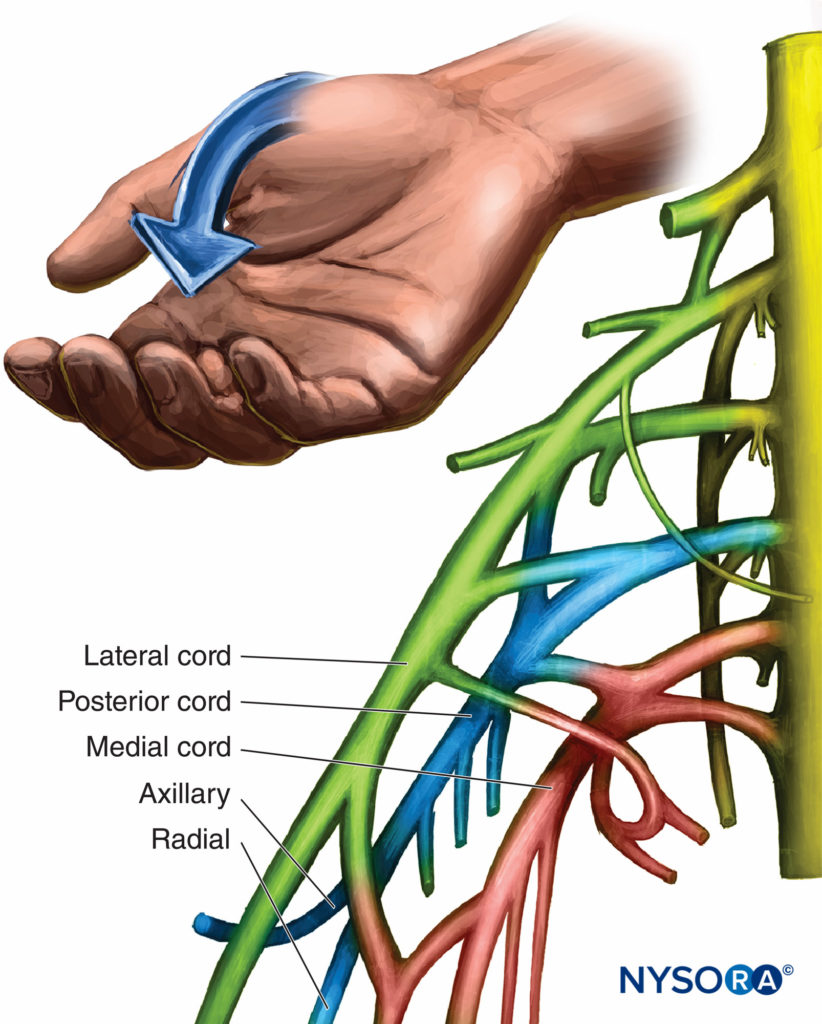
FIGURE 7. Organization and motor response of the posterior cord.
The Medial Cord
The medial cord branches into the ulnar nerve and the medial half of the median nerve. Branches include the medial pectoral, medial brachial cutaneous, and the medial antebrachial cutaneous nerves. These branches innervate the skin of the anterior and medial surfaces of the forearm to the wrist. The ulnar nerve innervates half of the fourth and the fifth fingers, the adductor pollicis, and all interossei, which results in contraction of the fourth and fifth fingers and thumb adduction. Median nerve stimulation results in flexion and sensation of the first three and one half fingers, opposition of the thumb, and sensation of the palm (Figure 8). Unlike the axillary block, responses to stimulation of the median nerve during infraclavicular block could conceivably arise from either the lateral or medial cord.
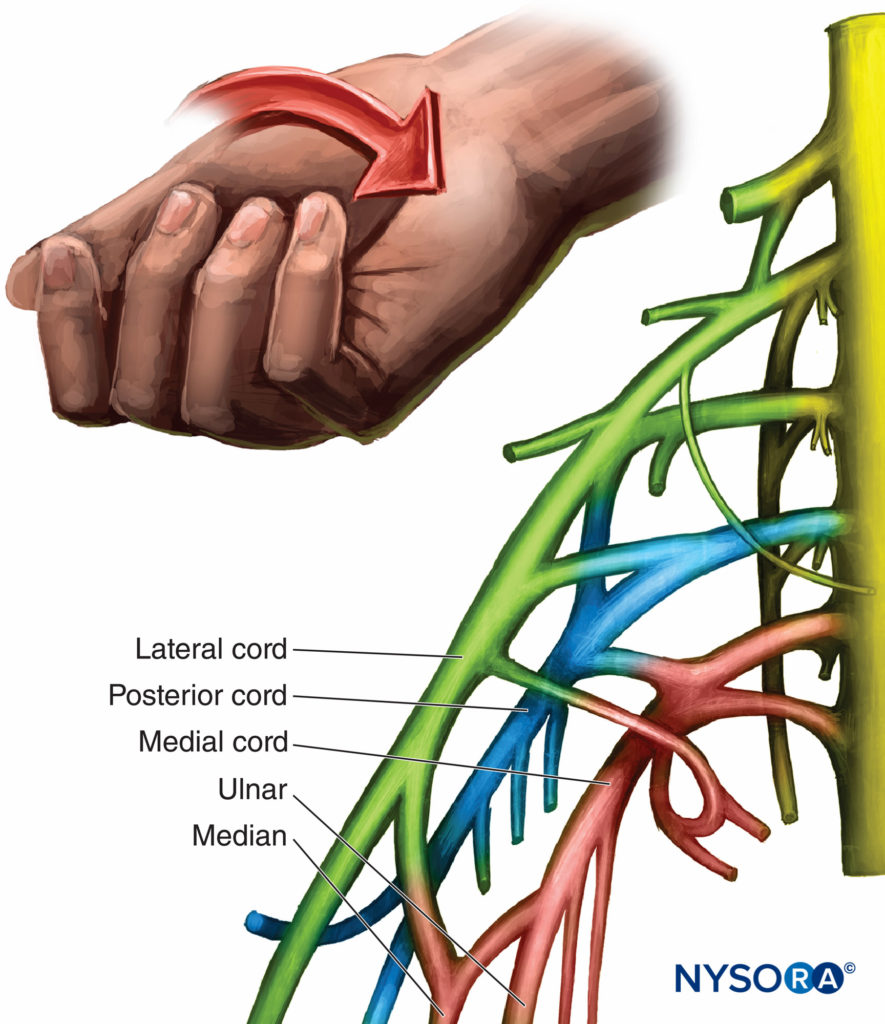
FIGURE 8. Organization and motor response of the medial cord.
Classic studies of fiber topography of the median nerve by Sunderland identified pronator teres fibers and flexor carpi radialis in the lateral root, along with nerves to the flexor digitorum profundus, flexor pollicis longus, and intrinsic thenar muscles in the medial root. Nerve injury studies also suggest that median fibers to the finger flexors are most likely found in the medial cord and medial root of the median nerve. With the most commonly occurring plexus anatomy, finger flexion most likely identifies medial cord (or root) stimulation, but wrist flexion may result from either median or lateral cord (or root) stimulation. Tables 1 and 2 summarize the cords, branches, terminal nerves, and their motor stimulus response. Because of anatomic variability and the mixing of the median nerve between the medial and lateral cords, the same responses are listed for both nerves. Except in rare variants, the ulnar nerve is carried within the medial cord. Learn more about the brachial plexus distribution in Functional Regional Anesthesia Anatomy.
LANDMARKS AND TECHNIQUE
General Guidelines
The bony landmarks used in most approaches are the clavicle, the jugular fossa or notch, the acromioclavicular joint, and the coracoid process, depicted in Figure 9.
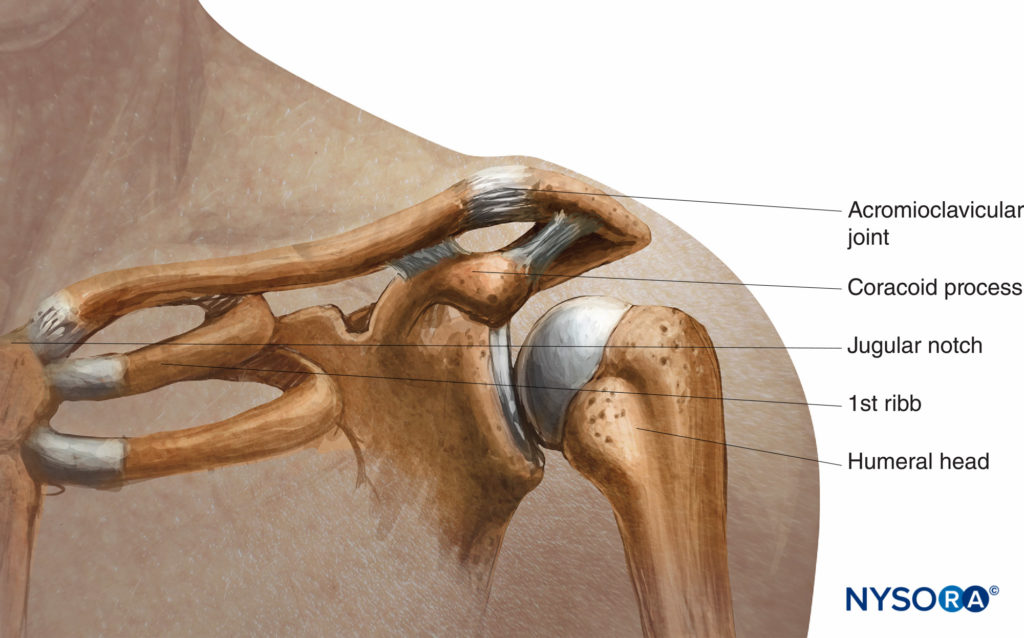
FIGURE 9. Relationship of the jugular (sternal) notch, clavicle and coracoid process.
MODIFIED RAJ APPROACH
A small amount, approximately 5 mL or less, of local anesthetic is needed for the skin and subcutaneous tissue. Care must be taken to avoid the pleura by never directing the needle in a medial direction. If the plexus is not encountered, the needle should be withdrawn and redirected sequentially by a factor of 10 degrees in either a cephalad or caudad direction. If those maneuvers are not successful, the landmarks should be reassessed before attempting another pass. Initial settings on the nerve stimulator are 1.5 mA, with an acceptable response occurring at less than 0.5 mA. Distal motor responses (below the elbow) are preferable. The infraclavicular block is a large-volume block, and 30 mL of local anesthetic is necessary to block the entire brachial plexus. Some commonly used local anesthetic solutions are listed in Table 3.
TABLE 3. Local anesthetic solutions for infraclavicular block.
| Duration | Anesthetic | |
|---|---|---|
| Short (1.5–3.0 h) | 3% chloroprocaine | |
| 1.5% lidocaine | ||
| Do not inject when the patient complains of pain or 1.0%–1.5% mepivacaine | ||
| Intermediate (4–5 h) | 2% lidocaine + epinephrine | |
| 1.0%–1.5% mepivacaine | ||
| Long-Lasting (10–14 h) | 0.25%–0.50% bupivacaine | (0.0625%–0.1% for infusion) |
| 0.50% ropivacaine | 0.1%–0.2% for infusion) |
The patient is in the recumbent position with the head turned away. The subclavian artery is palpated where it crosses the clavicle, or the midpoint of the clavicle is marked. The brachial artery is palpated and marked at the lateral border of the pectoralis muscle. A line joining these two points is made with needle insertion 2.5–3.0 cm below the midpoint of the clavicle at a 45- to 65-degree angle toward the axillary artery (Figure 10). The operator stands on the opposite side to the site of block placement. The skin is infiltrated with local anesthetic into the skin and pectoralis muscle. The first two fingers of the palpating hand anchor the skin at the point of insertion, and the needle is advanced at a 45- to 65-degree angle toward the point of brachial pulsation or parallel to a line connecting the medial clavicular head with the coracoid process if pulsation cannot be felt (Figure 11). If the plexus is not encountered, the needle should be withdrawn and redirected 10 degrees cephalad or caudad, depending on the originating angle of insertion. At no time should the needle be pointed medially or posteriorly toward the lung.
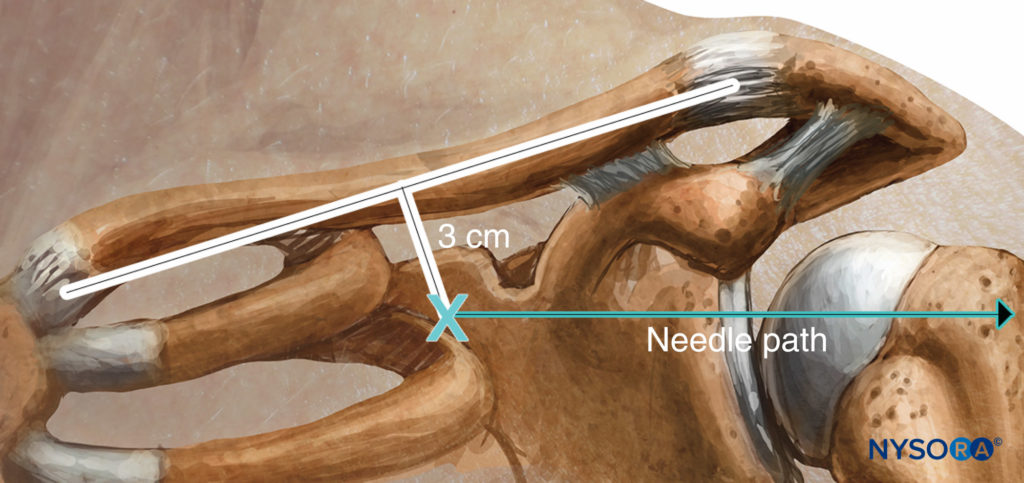
FIGURE 10. Raj approach: Landmarks and needle insertion plane.

FIGURE 11. Raj approach: Needle insertion and orientation.
VERTICAL INFRACLAVICULAR BLOCK
The vertical infraclavicular block was described by Kilka and coworkers in 1995. The landmarks are the midpoint of a line from the middle of the jugular notch and the ventral process of the acromion (Figure 12). The patient is lying in a supine position with the forearm relaxed on the chest with the head turned slightly to the side.
- Needle insertion is at the midpoint of the line from the jugular fossa to the acromioclavicular joint.
- Insertion is just under the clavicle.
- Needle assumes a 90-degree needle angle.
- A 50-mm needle is used
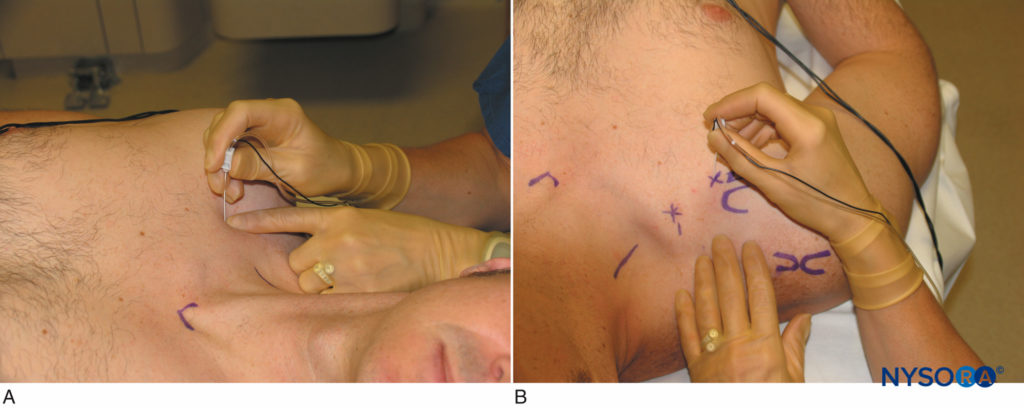
FIGURE 12. A AND B. Vertical approach: Needle insertion and orientation.
A 50-mm needle is inserted close to the clavicle at an angle of 90 degrees (see Figure 12). Local anesthetic is injected after a distal stimulus is obtained at or below 0.5 mA. If on first pass the needle does not encounter the plexus, only the angle is changed while keeping the same plane by 10 degrees caudad or cephalad. The needle is never directed in a medial fashion.
NYSORA Tips
The three most common errors that increase the risk of pneumothorax are:
- Too medial insertion of the needle
- Depth of needle insertion >6 cm
- Medial direction of needle
Adams described an improved success rate by moving the puncture site 1 cm laterally. The rate of unsuccessful block (defined as need for additional analgesic or sedation) was reduced to 8.3%, although this may depend on patient size. Using ultrasonographic assessment, Greher and colleagues demonstrated topographic anatomy in volunteers and compared the classic approach to a puncture site determined by high-resolution ultrasound location of the plexus. A clear trend was found to a more lateral puncture site, especially in women. They found that when the line from jugular fossa to acromion measured 22.0-22.5 cm the puncture site was exactly at the center of this line. However, for every 1 cm decrease in the length of this line the puncture site moved 2 mm laterally from the center and for every 1 cm increase the puncture site moved 2mm medially.
CORACOID TECHNIQUE (BLOCK)
The coracoid block as described by Whiffler11 in 1981 used a needle entry site that is most often inferior and medial to the coracoid process. In 1998, Wilson reviewed MRIs and located a point 2 cm medial to the coracoid process and 2 cm caudad. At this skin entry site, direct posterior insertion of the needle makes contact with the cords at a mean range of 4.24 cm ± 1.49 (2.25–7.75 cm) in men and 4.01 ± 1.29 cm (2.25–6.5 cm) in women. As shown in Figure 13, the lateral tip of the coracoid process (not the medial edge) is palpated. Kapral,19 in 1999, described a lateral approach with the patient in the same position. The point of needle insertion is lateral to the lateral point of the coracoid process. After identifying the coracoid process by touching the bone, the 7-cm needle is withdrawn 2–3 mm and redirected underneath the coracoid process 2–3 cm until the brachial plexus is reached. The usual distance was 5.5–6.5 cm. Rodriguez described his series of coracoid blocks as closer to the coracoid process by making his puncture site 1 cm inferior and 1 cm medial to the coracoid process. He reported a similar success rate.
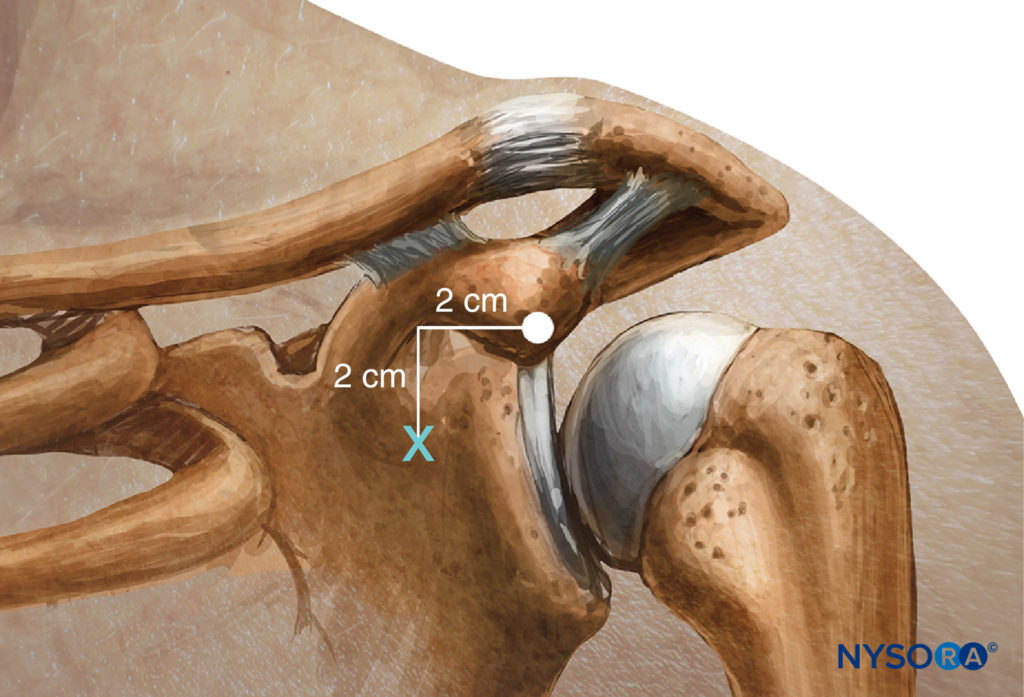
FIGURE 13. Coracoid approach: Landmarks.
THE LATERAL AND SAGITTAL TECHNIQUE LANDMARKS
In 2004, Klaastad and coworkers described this technique and tested it in an MRI model. The point of needle insertion is the intersection between the clavicle and the coracoid process (see Figure 2). The needle is advanced 15 degrees posteriorly, always strictly in the sagittal plane next to the coracoid process while abutting the anteroinferior edge of the clavicle. All needle directions in this method adhere strictly to the sagittal plane through this coracoid prominence. The posterior cord and medial cord were more often reached than the lateral cord. Insertion depth should be no greater than 6.5 cm. Although the cords are usually reached before the axillary artery and vein, puncture of these vessels as well as the cephalic vein is always a possibility.
Klaastad and coworkers reported occasionally needing to insert the needle more than 6.5 cm (their estimated maximal safe depth) to obtain satisfactory nerve contact and has not had a case of pneumothorax. The needle can encounter a vessel. Although initially used with a nerve stimulator, this technique has become the preferred method for use with ultrasound localization of the brachial plexus cords. The cords are superior and posterior to the axillary artery, most commonly at a depth of 4–6 cm. Although it is always possible to puncture the artery, the trajectory of this approach appears to avoid puncture of the axillary vessels because the cords are encountered cephalad to the artery and 2–3 cm cephalad to the pleural cavity. The use of ultrasound may improve block success and decrease morbidity compared with nerve stimulator alone.
SINGLE INJECTION VS MULTIPLE INJECTION AND CONTINUOUS TECHNIQUE
Single stimulation has been reported to have success rates from 82% to 100%. Gaertner and colleagues compared single stimulation to stimulation of all three cords. Multistimulation took slightly longer (9.0 vs 7.5 min); however, 2 of the 40 patients in the multistimulation group were excluded because three cords could not be localized within 15 minutes. A distal response in the hand or wrist was considered adequate with 10 mL of local anesthetic injected at each site. In the singlestimulation group, 30 mL of local anesthetic was injected after identifying a single response from any cord, (Figure 14). Although their overall success rate was low for both techniques (40.0% for single stimulation and 72.5% for multiple stimulation), Gaertner and colleagues reported that multiple stimulation was significantly more successful than single. The amount of local anesthetic, 30 mL, could have contributed to the overall decreased success rate. However, these researchers attributed the bulk of the difference in overall success to the varying definition of success in the literature.
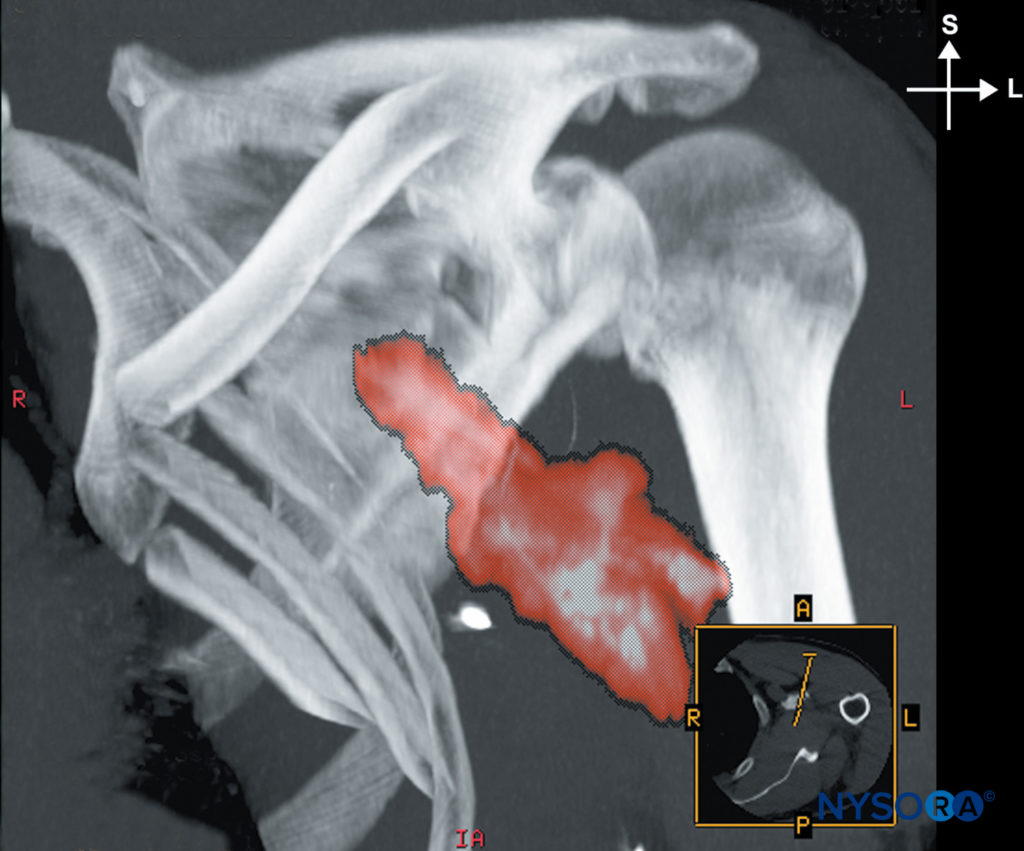
FIGURE 14. Distribution of the local anesthetic after injection through an indwelling catheter.
Hand surgery constitutes a large part of the surgeries in these studies. Most hand surgery can be performed with two or three of the nerves to the hand blocked if they are in the correct distribution of the surgery. Gaertner and colleagues felt more stringent criteria should be used. A complete motor and sensory block of all nerves was necessary for their criteria of success as compared with success defined as completing the procedure without supplementation or the need for general anesthesia. An example of this criterion is demonstrated by Rodriguez and collaborators21 in a random controlled trial comparing injection of 42 mL of mepivacaine using a single-, dual-, or triple-injection technique. A significantly less complete motor block was found with single injection versus the dual or triple injection. No significant difference was found in the dual- or triple-injection groups. In another study, comparing single and dual stimulation, 22% of the single stimulation group had a musculocutaneous or axillary response.
The investigators state that the recommendations for not accepting these responses is based on a published anecdotal report on a noncoracoid approach. Dual injection was suggested as the best balance between efficacy and comfort for patients and resulted in shorter block performance times and decreased vascular puncture rates compared with that for triple-stimulation injection. Deluze and coworkers found a similar effective rate when comparing single stimulation to triple stimulation by using 40 mL of 0.75% ropivacaine.
Continuous Technique
The infraclavicular block is well suited for continuous nerve block. Patient comfort and catheter securing are easier accomplished with an infraclavicular catheter rather than a dressing in the axillary area. If the distribution of the pain is in the axillary nerve or musculocutaneous areas, the chance of constant sensory block of those areas and pain relief are greater.
All approaches have been utilized successfully with a continuous technique, and there is no overwhelming evidence that favors a particular approach.
NYSORA Tips
- The coracoid process can easily be found even in obese patients. The middle finger is placed just below the clavicle and the hand is moved laterally toward the shoulder. The first bony prominence that is felt by the index finger is the coracoid process. The patient’s head should be turned to the opposite side.
SUMMARY
The infraclavicular block provides a useful alternative to axillary block for surgery of the arm. The block is reliable for surgery and amenable to ultrasound technique and can be used for continuous as well as single-shot techniques.
For a more comprehensive review of the infraclavicular block, see Ultrasound-guided infraclavicular brachial plexus block.
REFERENCES
- Hirschel G: Die Anasthesierung des Plexus brachialis bei Operationen der oberen Extremitat. MMW Munch Med Wochenschr 1911;58:1555–1556.
- Kulenkampff D: Anasthesie des Plexus brachialis. Zentralbl Chir 1911;8:1337–1350.
- Bazy L, Pouchet V, Sourdat V, et al: J Anesth Reg 1917;222–225.
- From Zentralbl Chir 45, 1918. In Winnie AP: Plexus Anesthesia. Philadelphia, PA: Saunders, 1983, pp 215–217.
- Labat’s Regional Anesthesia: Its Technique and Clinical Application, Philadelphia, PA: Saunders, 1923, p 223.
- Dogliotti AM: Anesthesia: Narcosis, Local, Regional, Spinal. SB Debour: Chicago, 1939.
- Moore DC: Regional Block, 4th ed. Springfield, IL: Thomas, 1981.
- Cousins MJ, Bridenbaugh PO: Neural block in Clinical Anesthesia and Pain Management. Philadelphia, PA: Lippincott, 1980.
- Raj PP, Montgomery SJ, Nettles D, et al. Infraclaficular brachial plexus block—a new approach. Anesth Analg 1973;52:897–904.
- Sims JK: A modification of landmarks for infraclavicular approach to brachial plexus block. Anesth Analg 1977;56:554–557.
- Whiffler K: Coracoid block—a safe and easy technique. Br J Anaesth 1981;53:845.
- Winnie AP: Plexus Anesthesia. Philadelphia, PA: Saunders, 1983.
- Klaastad O, Lileas FG, Rotnes JS, et al. Magnetic resonance imaging demonstrates lack of precision in needle placement by the infraclavicular brachial plexus block described by Raj et al. Anesth Analg 1999;88:593–598.
- Kilka HG, Geiger P, Mehrkens HH: Infraclavicular block. A new method for anesthesia of the upper extremity: an anatomical and clinical study. Anaesthesist 1995;44:339–344.
- Wilson JL, Brown DL, Wongy GY: Infraclavicular brachial plexus block: parasagittal anatomy important to the coracoid technique. Anesth Analg 1998;87:870–873.
- Gelberman RH: Operative Nerve Repair and Reconstruction. Philadelphia, PA: Lippincott, 1991, p 1288.
- Sunderland S: The intraneural topography of the radial, median, and ulnar nerves. Brain 1945;68(pt 4):243–299.
- Weller RS, Gerancher JC: Brachial plexus block: “best” approach and “best” evoked response—where are we? Reg Anesth Pain Med 2004;29:520–523.
- Kapral S, Jandrasits O, Schabernig C, et al. Lateral infraclavicular plexus block vs. axillary block for hand and forearm surgery. Acta Anaesthesiol Scand 1999;43:1047–1052.
- Greher M, Retzl G, Niel P, et al. Ultrasound assessment of topographic anatomy in volunteers suggests a modification of the infraclavicular block. Br J Anaesth 2002;88:621–624.
- Rodriguez J, Barcena M, Taboada-Muiz M, et al. A comparison of single versus multiple injections on the extent of anesthesia with coracoid infraclavicular brachial plexus block. Anesth Analg 2004;99:1225–1230.
- Rodriguez J, Barcena M, Lagunilla J, et al. Increased success rate with infraclavicular brachial plexus block using a dual-injection technique. J Clin Anesthesia 2004;16:251–256.
- Klaastad O, Smith HG, Smedby O, et al. A novel infraclavicular brachial plexus block: the lateral and sagittal technique, developed by magnetic resonance imaging studies. Anesth Analg 2004;98:252–256.
- Gaertner E, Estebe JP, Zamfir A, et al. Infraclavicular plexus block: multiple injection versus single injection. Reg Anesth Pain Med 2002;27:590–594.
- Klaastad O, Smith H-J, Smedby O, et al. Response to letter to editor. Anesth Analg 2004;99:950–951.
- Brull R, McCartney C, Chan V: A novel approach to the infraclavicular brachial plexus block: The ultrasound experience [Letter]. Anesth Analg 2004;99:950.
- Borgeat A, Ekatodramis G, Dumont C: An evaluation of the infraclavicular block via a modified approach of the Raj technique. Anesth Analg 2001:93:436–441.
- Jandard C, Gentili ME, Girard F, et al. Infraclavicular block with lateral approach and nerve stimulation: Extent of anesthesia and adverse effects. Reg Anesth Pain Med 2002;27:37–42.
- Fitzgibbon DR, Deps AD, Erjavec MK: Selective musculocutaneous nerve block and infraclavicular brachial plexus anesthesia. Reg Anesth 1995;20:239–241.
- Rodriguez J, Taboada-Muiz M, Barcena M, et al. Median versus mus- culocutaneous nerve response with single-injection infraclavicuar coracoid block. Reg Anesth Pain Med 2004:29:534–538.
- Deluze A, Gentili ME, et al. A comparison of a single-stimulation lateral infraclavicular plexus block with a triple stimulation axillary block. Reg Anesth Pain Med 2003;28:89–94.
- Mehrkens HH, Geiger PK: Continuous brachial plexus block via the vertical infraclavicular approach. Anaesthesia 1998;53(Suppl 2):
19–20. - Macaire P, Gaertner E, Capdevila X: Continuous post operative regional analgesia at home. Minerva Anestesiol 2001;67:109–116.

