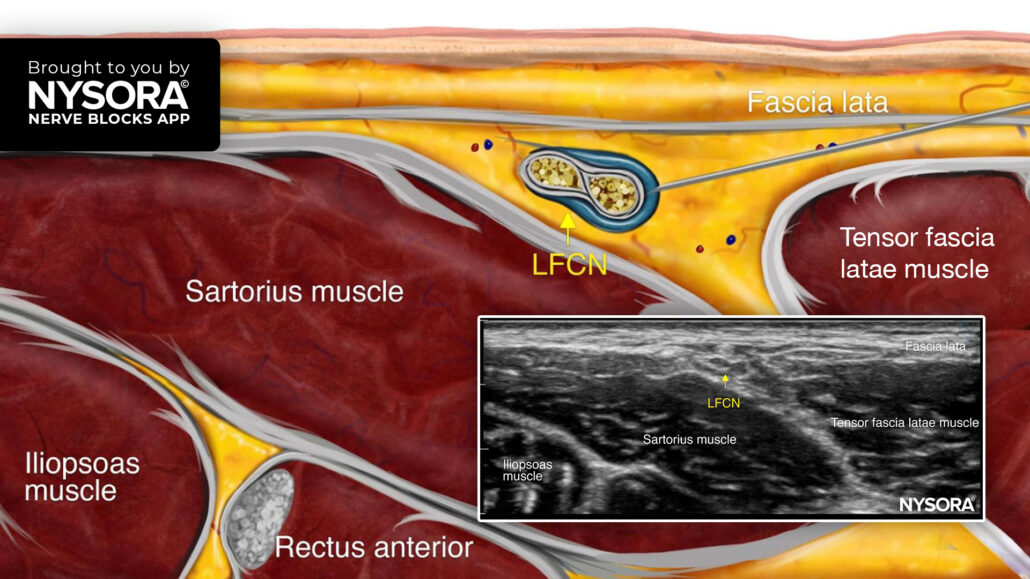
Tips for a Lateral Femoral Cutaneous Nerve Block
The lateral femoral cutaneous nerve (LFCN) block is indicated for analgesia for surgery on the anterolateral thigh (e.g., skin grafting), muscle biopsy, and meralgia paresthetica. The complex branching of the LFCN makes accurate landmark-based blocks difficult, but ultrasound guidance ensures precise needle placement, enhancing pain relief and outcomes.
The management of post-surgical pain has always been a significant challenge for healthcare providers, especially in hip surgeries where pain can be severe. The study of Nielsen et al. 2018 introduces a novel ultrasound-guided technique to block the lateral femoral cutaneous (LFC) nerve, which provides improved pain relief after hip surgery. This technique offers a targeted, efficient approach to anesthetizing the sensory nerves that innervate the lateral thigh, minimizing complications and maximizing pain coverage.
What is the lateral femoral cutaneous nerve?
The LFC nerve originates from the lumbar spine and runs down to the thigh, providing sensation to the lateral aspect of the thigh. Blocking this nerve can greatly reduce post-surgical pain in the affected area, particularly in hip surgeries.
However, achieving effective pain relief via nerve blocks in this region has been historically challenging. Prior techniques have been inconsistent, particularly in anesthetizing the proximal nerve branches critical for many hip surgeries. These challenges arise from the LFC nerve’s anatomical variability and technical difficulties in targeting it accurately with traditional methods.
Challenges in traditional LFC nerve blocks
In conventional techniques, achieving complete anesthesia of the LFC nerve is difficult due to several factors:
- Anatomical variability: The LFC nerve exhibits significant anatomical variation, making it difficult to predict which branches will be effectively anesthetized.
- Proximal nerve branches: Many surgical incisions, particularly in hip surgeries, require blocking the proximal branches of the LFC nerve. Failure to anesthetize these branches can lead to inadequate pain relief.
- Technical difficulties: Traditional techniques often target the LFC nerve deep to the inguinal ligament or anterior to the sartorius muscle, which can complicate the procedure and reduce its success rate.
A novel ultrasound-guided approach
This novel approach focuses on a more reliable, ultrasound-guided method of blocking the LFC nerve by targeting it in a structure called the fat-filled flat tunnel (FFFT), located between two major muscles in the thigh: the sartorius and tensor fasciae latae. This tunnel provides an accessible and predictable location for administering the anesthetic, improving the success rate of the nerve block.
Key features of the technique:
- Ultrasound guidance: Ultrasound allows for precise visualization of the LFC nerve within the FFFT. This improves accuracy in targeting the nerve, reducing the risk of blocking adjacent nerves, such as the femoral nerve, which could cause motor complications.
- Dynamic needle tip tracking: Real-time tracking of the needle tip during the injection ensures the anesthetic spreads effectively along the nerve’s course. This dynamic approach ensures the entire nerve, including proximal branches, is adequately anesthetized.
- Fat-filled flat tunnel (FFFT): The FFFT serves as a natural anatomical space for the nerve block, ensuring the injectate spreads around the LFC nerve and covers the necessary sensory regions.
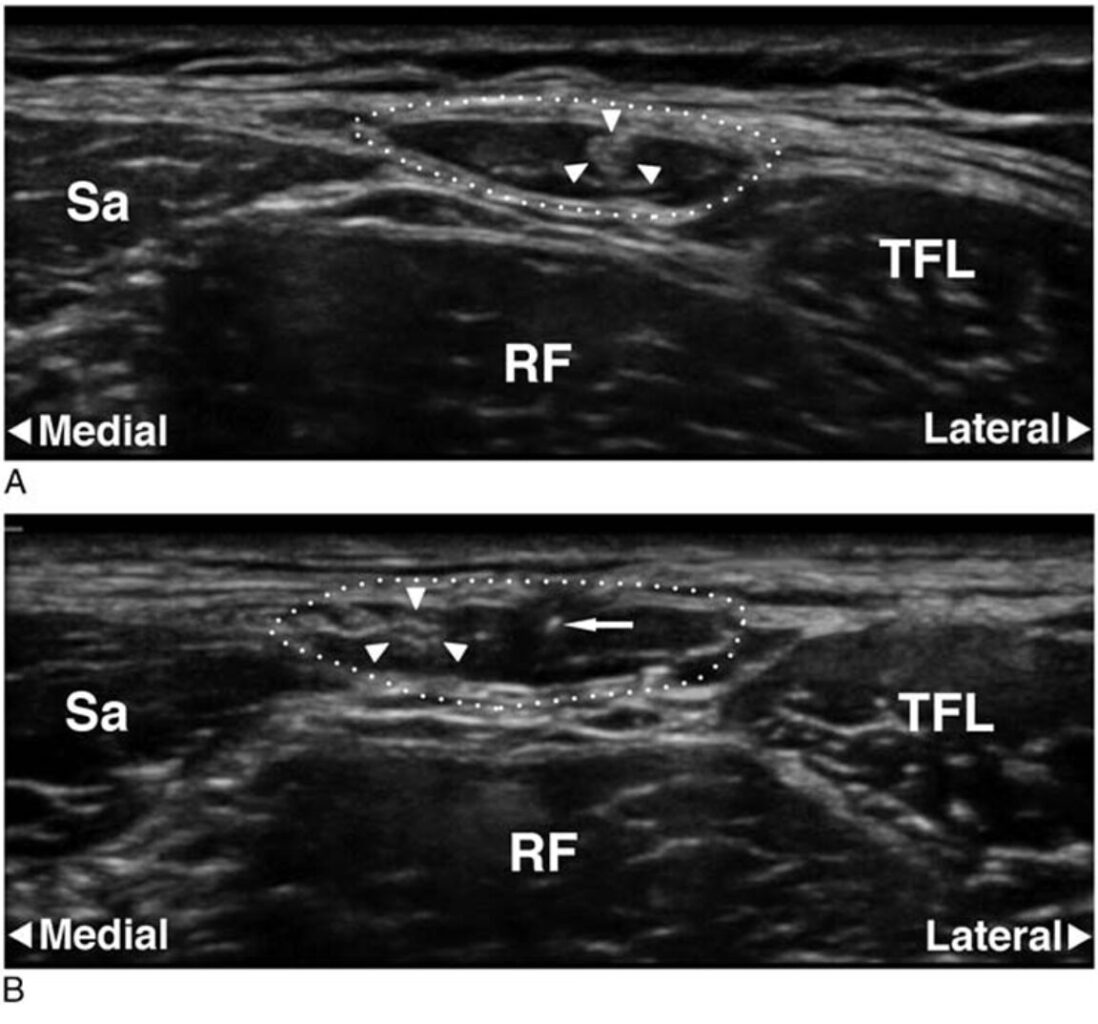
Ultrasound images of the fat-filled flat tunnel (FFFT). In A, a transverse scan taken 10 cm below the anterior superior iliac spine (ASIS) shows the outlined circumference of the FFFT, with the lateral femoral cutaneous (LFC) nerve (marked by arrowheads) visible as a hyperechoic structure within the dark (anechoic) fat inside the FFFT. In B, another transverse scan 5 cm below the ASIS captures the needle tip (marked by an arrow) in cross-section, with the LFC nerve (arrowheads) entering the FFFT just after passing over the front of the sartorius muscle (Sa). Additional muscle landmarks include the rectus femoris (RF) and tensor fasciae latae (TFL) muscles. Source of the image: Nielsen et al. Regional Anesthesia & Pain Medicine. 2018 Aug;43(6):650-651.
Methods
The study to evaluate this technique consisted of two parts: a cadaveric study and a clinical trial involving healthy volunteers.
Cadaveric study
- The researchers first tested the technique on cadavers to assess how effectively the anesthetic spread to the nerve branches.
- They used real-time ultrasound to inject 5-10 mL of anesthetic into the FFFT and tracked the distribution.
Clinical trial
- Following the success of cadavers, the technique was tested on 20 healthy volunteers in a randomized, controlled clinical trial.
- The key outcome measured was how effectively the anesthetic covered the proximal LFC nerve branches.
Results
- 95% Success rate: The technique successfully anesthetized the lateral thigh in 95% of cases, as confirmed by sensory testing.
- 68% Coverage of proximal branches: The technique effectively blocked the proximal branches of the LFC nerve in 68% of cases. This is crucial for covering surgical incisions in the upper thigh.
- No femoral nerve block: One of the major advantages of this technique is the reduced risk of inadvertently blocking the femoral nerve, which is critical for preserving motor function in the leg.
Benefits of the new technique
This novel LFC nerve block technique offers several advantages over traditional methods:
- Using ultrasound guidance, clinicians can visualize the LFC nerve and ensure the anesthetic is delivered exactly where needed. This reduces variability in outcomes and enhances the block’s reliability.
- The technique provides more consistent anesthesia of the lateral thigh, particularly in areas close to the hip joint where traditional blocks may fail. This translates into better pain control for patients undergoing hip arthroplasty or fracture repair procedures.
- Traditional LFC nerve blocks, especially those done deep into the inguinal ligament, carry the risk of blocking the femoral nerve. This can result in motor complications, such as weakness in the leg muscles. The FFFT technique avoids this issue, providing better outcomes for patients.
Conclusion
The novel ultrasound-guided lateral femoral cutaneous nerve block technique presents a promising advancement in regional anesthesia. Targeting the fat-filled flat tunnel (FFFT) between the sartorius and tensor fasciae latae muscles allows for precise anesthesia of the LFC nerve, particularly its proximal branches, which are crucial in many hip surgeries. The technique’s high success rate, along with its minimal risk of motor block, offers significant potential for improving postoperative pain management and reducing opioid reliance.
For more detailed information, refer to the full article in Regional Anesthesia & Pain Medicine.
Coraci D, Giovannini S, Loreti C, Ruggeri F, Padua L. The Lateral Femoral Cutaneous Nerve: Ultrasound Support in Nerve Assessing. Reg Anesth Pain Med. 2018 Aug;43(6):650-651.
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!