Tips for a Paravertebral Block: Transverse Oblique Technique
Paravertebral blocks have been a cornerstone in regional anesthesia for many types of surgeries, especially in thoracic and breast surgeries, providing efficient pain management. Over time, advances in medical technology have introduced ultrasound-guided techniques and novel alternatives to traditional methods. In this post, we explore the effectiveness, safety, and recent developments in paravertebral blocks, focusing on both landmark-based and ultrasound-guided methods and emerging paraspinal blocks.
What Are Paravertebral Blocks?
Paravertebral blocks involve local anesthetic injection near the vertebral column, specifically in the thoracic paravertebral space. The block targets the nerves exiting the spinal cord to provide analgesia or anesthesia in the corresponding area of the chest or abdomen. The key benefits include:
- Effective analgesia: Commonly used in thoracic and abdominal surgeries.
- Postoperative pain relief: Reduces the need for opioids, lowering the risk of opioid-related side effects.
- Potential use as the sole anesthetic: In specific surgeries like breast surgery, PVB can be used as the primary anesthetic.
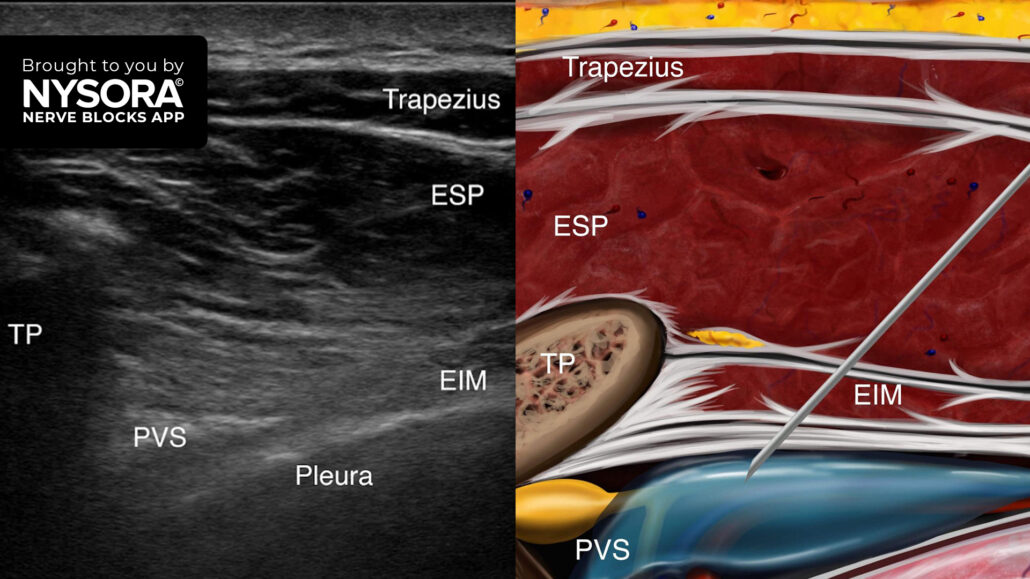
The anatomy of the thoracic paravertebral space
Understanding the anatomy of the thoracic paravertebral space (TPVS) is crucial for performing safe and effective blocks. The space is bordered by the pleura (the lining of the lungs), the vertebral column, and the ribs. It contains vital structures like the intercostal nerves and the sympathetic chain, making it a high-precision technique to avoid complications like pneumothorax (collapsed lung) or vascular injury.
Landmark-based technique
The traditional method relies on anatomical landmarks to guide needle placement. The patient is placed in a sitting or lateral position, and a needle is inserted approximately 2.5-3 cm lateral to the spinous process at the appropriate vertebral level. While effective, this technique has a higher failure rate (up to 5.6%) and a small risk of serious complications, including nerve injury and pneumothorax.
Ultrasound-guided technique
Ultrasound-guided PVB has transformed the procedure by allowing real-time visualization of the anatomical structures. This reduces the failure rate (down to 0-2.3%) and complications. Ultrasound guidance helps:
- Visualize the needle’s path: Improves precision in needle placement.
- Ensure proper anesthetic spread: Reduces the risk of unintended injection sites.
- Shorten onset time: Provides faster pain relief.
Recent advances: novel paraspinal blocks
Recently, novel paraspinal blocks have emerged as potential alternatives to the traditional PVB. These techniques are also ultrasound-guided but aim to achieve similar pain relief without entering the paravertebral space directly.
Erector spinae plane (ESP) block
The ESP block is one of the most promising new techniques. In this method, the needle is inserted into the fascial plane between the erector spinae muscle and the transverse processes of the vertebrae. This technique offers:
- Simplicity and safety: The needle is placed further from the pleura, reducing the risk of pneumothorax.
- Wide coverage: A single injection can provide a multilevel dermatomal block.
Retrolaminar block
This block involves guiding the needle to the lamina (part of the vertebra) instead of entering the paravertebral space directly. Similar to the ESP block, it avoids the TPVS, making it potentially safer.
Mid-point transverse process to pleura (MTP) block
In the MTP block, the needle is directed to the mid-point between the transverse process and the pleura. This block may offer similar benefits to PVB without entering the paravertebral space directly.
Indications for PVB
Paravertebral blocks are versatile and can be used for a wide range of surgeries, including:
- Thoracic and breast surgery: Effective for both analgesia and anesthesia.
- Chronic pain management: For neuropathic pain and post-surgical pain syndromes.
- Other procedures: Include renal surgeries, inguinal herniorrhaphy, and laparoscopic cholecystectomy.
Efficacy of PVB in breast and thoracic durgery
Two systematic reviews have demonstrated that PVB is highly effective in reducing postoperative pain after breast surgery. It lowers opioid requirements, postoperative nausea, and the incidence of chronic post-surgical pain (CPSP). The use of PVB for thoracic surgery has also been shown to reduce complications like hypotension and urinary retention when compared to thoracic epidural analgesia.
Complications and risk factors
While PVB is generally considered safe, complications can occur, particularly when using landmark-based techniques:
- Block failure: The failure rate is higher in landmark techniques, between 1.98% and 5.6%. This can result in inadequate pain relief or the need for additional interventions.
- Pneumothorax: A feared complication, especially in landmark-based PVBs, where the needle may inadvertently puncture the pleura.
- Vascular puncture: This can occur during multi-level injections, with a reported incidence of up to 9% in bilateral PVBs.
- Hypotension: Seen in less than 1% of cases, hypotension occurs due to the block’s proximity to the sympathetic chain, which can lead to temporary autonomic dysfunction.
Lower complication rates with ultrasound
Using ultrasound guidance significantly reduces the risk of these complications by allowing the anesthetist to visualize the structures in real time. In a retrospective study involving 1500 ultrasound-guided blocks, no cases of pneumothorax were reported, underscoring the importance of image guidance in minimizing complications.
Conclusion
Paravertebral blocks, whether landmark-based or ultrasound-guided, are effective techniques for providing analgesia and anesthesia, particularly in thoracic and breast surgeries. With the advent of ultrasound guidance and novel paraspinal blocks, the safety profile of these blocks has significantly improved, making them a reliable option for pain management.
A paravertebral block is recommended for pain management following breast surgery, thoracotomy, rib fractures, and procedures involving the thoracic and upper abdominal regions. This technique involves injecting local anesthetic alongside the thoracic vertebra, near where the spinal nerves emerge from the intervertebral foramen.
Here are our 3 go-to tips to perform a paravertebral block with the transducer placed in a transverse oblique orientation
- Place the transducer just lateral to the spinous process at the targeted level in a transverse oblique orientation parallel to the course of the ribs. Visualize the transverse processes and ribs as hyperechoic structures with acoustic shadowing below them.
- Move the transducer slightly caudad into the intercostal space to identify the tip of the transverse process and the hyperechoic line of the pleura. The hyperechoic internal intercostal membrane can be visualized limiting the thoracic paravertebral space and the adjoining intercostal space as a wedge-shaped hypoechoic layer.
- Insert the needle in-plane, from lateral to medial, toward the paravertebral space. The goal is to inject the local anesthetic below the internal intercostal ligament, resulting in a downward displacement of the pleura, indicating the proper spread of the local anesthetic.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!