Jerry D. Vloka and Luc Van Keer
INTRODUCTION
Blocks of the lateral femoral cutaneous, posterior femoral cutaneous, saphenous, sural, and superficial peroneal nerves are useful anesthetic techniques for a variety of superficial surgical procedures and carry a low risk of complications.
Indications and Contraindications
The lateral femoral cutaneous nerve block has been used to provide anesthesia for pediatric patients undergoing muscle biopsy and to provide analgesia after femoral neck surgery in older patients. The posterior femoral cutaneous nerve block is used for any surgical procedure performed on the posterior aspect of the thigh. The saphenous, sural, and superficial peroneal nerve blocks can be used as part of an ankle block to provide complete anesthesia to the foot and ankle, or they can be used separately to provide anesthesia to specific portions of the foot and ankle. The contraindications to performing cutaneous nerve blocks of the lower extremity are few, but include local infection at the sites of needle insertion, and allergy to local anesthetic.
Functional Anatomy
The cutaneous nerves of the extremities are blocked by injection of local anesthetic in the subcutaneous layers above the muscle fascia. The subcutaneous tissue contains a variable amount of fat, superficial nerves, and vessels. Deep to this area lies a tough membranous layer, deep fascia of the lower extremity enclosing muscles of the leg. This deep fascia is penetrated by numerous superficial nerves and vessels.
The cutaneous innervation of the lower extremity is accomplished by nerves that are part of the lumbar and sciatic plexuses (Figures 1 and 2). A more detailed review of the relevant anatomy is provided with a description of the individual block procedures in Functional Regional Anesthesia Anatomy.
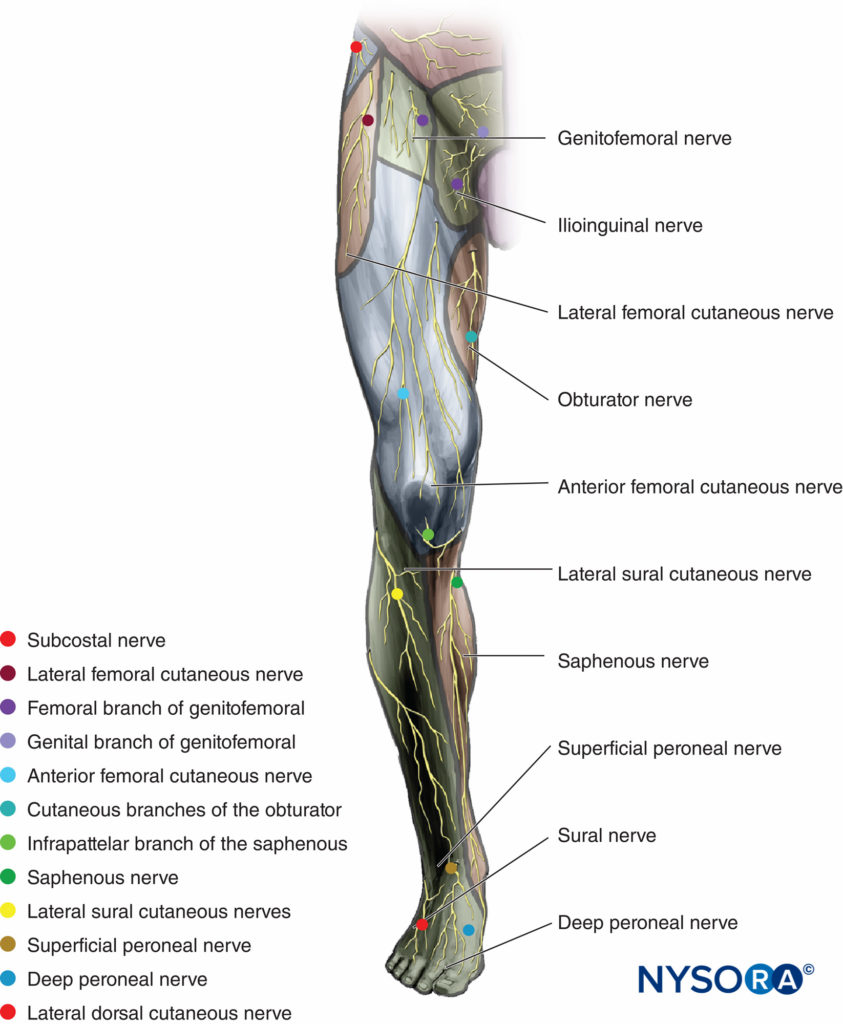
FIGURE 1. Cutaneous innervation of the lower extremity, anterior view.
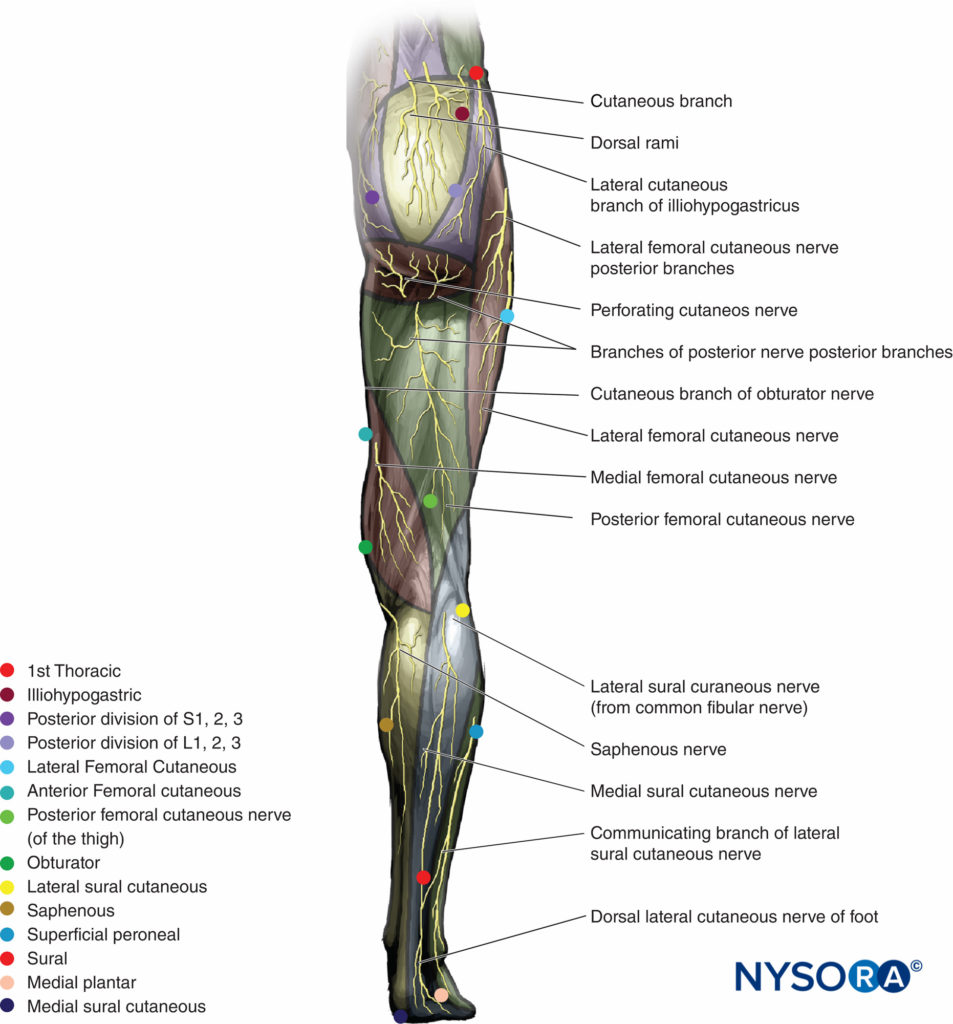
FIGURE 2. Cutaneous innervation of the lower extremity, posterior view.
Choice of Local Anesthetic
Any local anesthetic can be used for cutaneous blocks of the lower extremity; the choice is based primarily on the desired duration of block. Because these blocks do not result in motor block, longeracting local anesthetics are most commonly chosen (e.g., 0.2%–0.5% ropivacaine or 0.25%-0.5% bupivacaine). When performing blocks in the ankle area, it is always prudent to avoid using epinephrine owing to the risk of decreasing blood flow to the toes. Onset time for the block depends on the local anesthetic used (Table 1).
TABLE 1. Choice of anesthetic for cutaneous nerve block of the lower extremity.
| Onset (min) | Anesthesia (h) | Analgesia (h) | |
|---|---|---|---|
| 1.5% Mepivacaine | 15–20 | 2–3 | 3–5 |
| 2% Lidocaine | 10–20 | 2–5 | 3–8 |
| 0.5% Ropivacaine | 15–30 | 4–8 | 5–12 |
| 0.75% Ropivacaine | 10–15 | 5–10 | 6–24 |
| 0.5% (L) Bupivacaine | 15–30 | 5–15 | 6–30 |
LATERAL FEMORAL CUTANEOUS NERVE BLOCK
General Considerations
This block can be used to provide complete anesthesia in patients undergoing skin graft on the lateral aspect of the thigh, or it can be combined with femoral block or sciatic block. Its use has also been reported as a diagnostic tool for meralgia paresthetica, neuralgia of the lateral femoral cutaneous nerve of the thigh.
Distribution of Anesthesia
The lateral femoral cutaneous nerve provides sensation to the anterolateral aspect of the thigh (see Figure 1). In some patients however, the nerve can provide surprisingly large innervation territory of the anterior thigh as well.
Patient Positioning
The patient is in a supine position and the anterior superior iliac spine is palpated and marked.
Anatomic Landmarks
The main landmark for lateral femoral cutaneous nerve block is the anterior superior iliac spine. The lateral femoral cutaneous nerve emerges from the lateral border of the psoas major muscle and crosses the iliacus muscle obliquely toward the anterior superior iliac spine, where it supplies the parietal peritoneum of the iliac fossa. The nerve then passes into the thigh behind or through the inguinal ligament, variably medial to the anterior iliac spine (typically about 1 cm) or through the tendinous origin of the sartorius muscle, dividing into anterior and posterior branches.
The anterior branch becomes superficial about 10 cm distal to the anterior superior iliac spine supplying innervation to the skin of the anterior and lateral thigh as far as the knee. It connects terminally with the cutaneous branches of the anterior division of the femoral nerve and the infrapatellar branch of the saphenous nerve, forming the patellar plexus. The posterior branch pierces the fascia lata higher than the anterior, dividing to supply the skin on the lateral surface from the greater trochanter to about the middle of the thigh and occasionally also supplying the gluteal skin.
Technique
A 22-25 gauge needle is inserted 2 cm medial and 2 cm distal to the anterior superior iliac spine (Figure 3). The needle is advanced until a loss of resistance or a “pop” is felt as the needle passes through the fascia lata. Because this fascia “give” is not consistent and its perception may vary among practioners, local anesthetic is injected in a fanwise fashion both above and below the fascia lata from medial to lateral. A volume of 10 mL of local anesthetic is injected for this block. Although the lateral femoral cutaneous nerve is a sensory nerve, relatively higher concentrations of lo,g-acting local anesthetic are useful to increase the succes rate (0,5% ropivacaine or bupivacaine) because this is essential a “blind” technique. Alternatively, nerve stimulator (2 mA, 1 msec) can be used to elect paresthesia sensation in the typical distribution of the nerve to assure its location.

FIGURE 3. Lateral femoral cutaneous nerve block. The landmark for this block is the anterior superior iliac spine.
When used to provide anesthesia for a skin graft harvest site on the lateral thigh, the peripheral innervation of the lateral femoral cutaneous nerve in specific patients is outlined before beginning harvesting. Because no larger vascular structures or other organs are nearby, block of the lateral femoral cutaneous nerve carries a minimal risk of complications.
POSTERIOR CUTANEOUS NERVE OF THE THIGH BLOCK
General Considerations
This block has been used in burn patients with donor skin for grafting taken from the posterior thigh or as part of a popliteal/posterior femoral cutaneous nerve block in short saphenous vein stripping.
Distribution of Anesthesia
The posterior cutaneous nerve of the thigh innervates the skin over the posterior thigh between the lateral femoral cutaneous and anterior femoral cutaneous nerves (see Figure 2).
Patient Positioning
The patient can be positioned prone, in the lateral decubitus position (shown in Figures 4 and 5), or supine with the leg elevated 90 degrees.

FIGURE 4. Posterior cutaneous nerve of the thigh block, subgluteal approach.
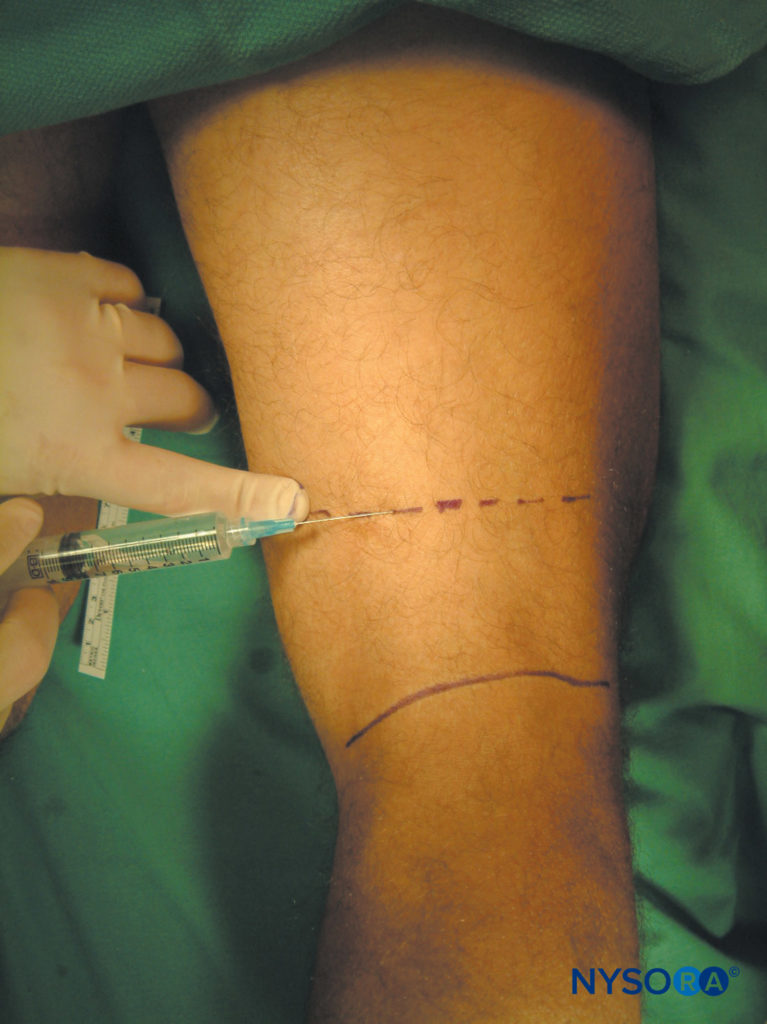
FIGURE 5. Posterior cutaneous nerve of the thigh block, midthigh approach.
Anatomic Landmarks
The posterior femoral cutaneous nerve originates from the dorsal branches of the first and second sacral rami and from the ventral branches of the second and third sacral rami.
It runs through the greater sciatic foramen below the piriformis and descends under the gluteus maximus muscle with the inferior gluteal vessels, posterior or medial to the sciatic nerve. The nerve then descends in the back of the thigh deep to the fascia lata. Its branches are all cutaneous and are distributed to the gluteal region, the perineum, and the flexor aspect of the thigh and leg.
Technique
The gluteal fold is identified and 10 mL of local anesthetic is injected subcutaneously to raise a skin wheal (see Figure 4). In addition, at the midpoint of the gluteal crease, 5 mL of local anesthetic is injected at a deeper level, using a fan technique to reach the nerve that has not emerged through the deep fascia. To block the posterior cutaneous nerve of the thigh above the knee level, as for short saphenous vein stripping (as a complement to popliteal block), 10 mL of local anesthetic is injected subcutaneously along a line 5 cm above and parallel with the popliteal crease (see Figure 5).
SAPHENOUS NERVE BLOCK
General Considerations
The saphenous nerve block is most commonly used in combination with a sciatic nerve block or popliteal block to complement anesthesia of the lower leg for various vascular, orthopedic, and podiatric procedures. The saphenous nerve is a terminal cutaneous branch of the femoral nerve. Its course is in the subcutaneous tissue of the skin on the medial aspect of the ankle and foot. All cutaneous nerves of the foot should be thought of as a neuronal network rather than well defined innervation territories of specific nerves.
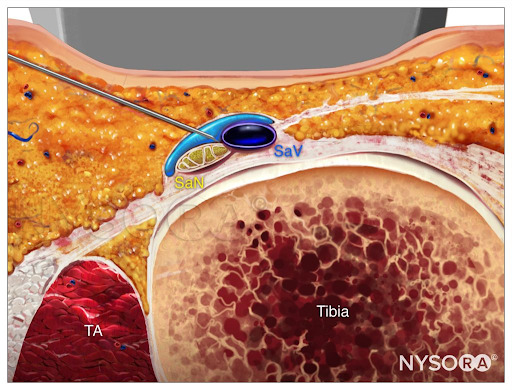
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for a saphenous nerve block with needle insertion in-plane and local anesthetic spread (blue). TA, tibialis anterior muscle; SaN, saphenous nerve; SaV, saphenous vein.
Distribution of Anesthesia
The saphenous nerve innervates the skin over the medial, anteromedial, and posteromedial aspects of the lower leg from above the knee (part of the patellar plexus) to as low as the first metatarsophalangeal joint in some instances (Figures 1 and 7).
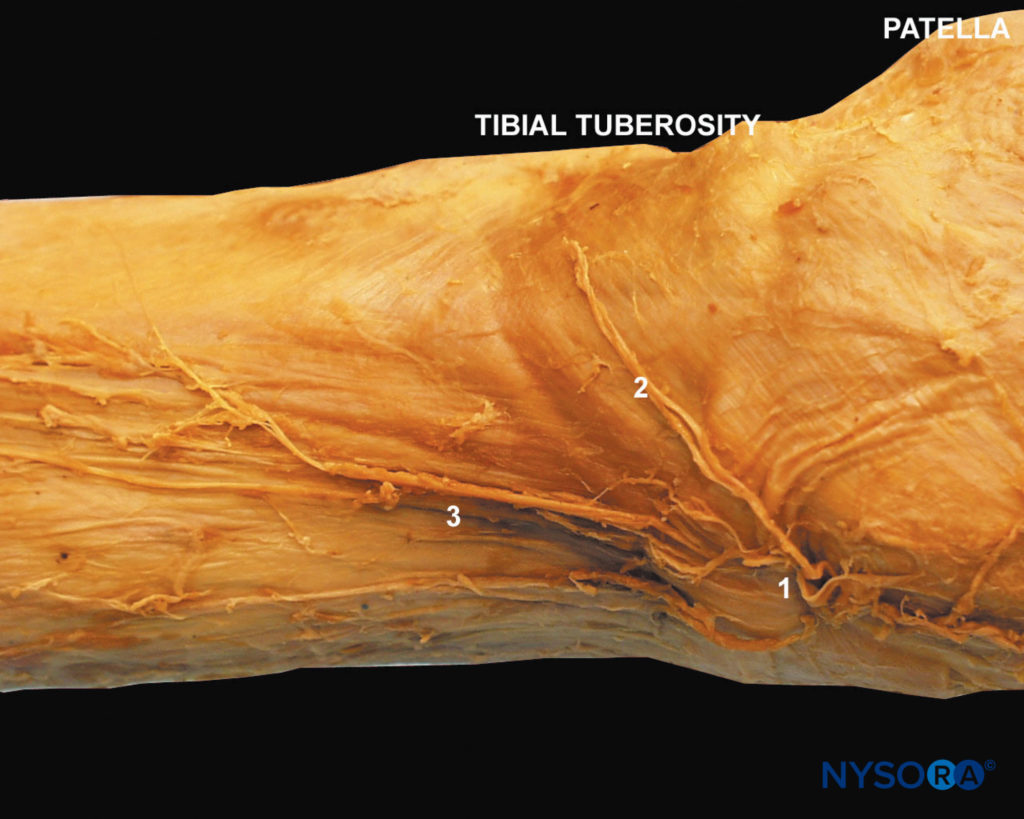
FIGURE 7. Saphenous nerve anatomy. Saphenous nerve pierces through the sartorius muscle (1), subpatellar branch (2), saphenous nerve in its descent on the medial aspect of the thigh (3).
Patient Positioning
The patient is placed supine with the leg to be blocked supported by a footrest.
Anatomic Landmarks
The main landmark for this block is the tibial tuberosity, an easily recognizable and palpable bony prominence on the anterior aspect of the tibia, a few centimeters distal from the patella (Figure 6). The saphenous nerve is the largest cutaneous branch of the femoral nerve. It descends lateral to the femoral artery into the adductor canal, where it crosses anteriorly to become medial to the artery. It proceeds vertically along the medial side of the knee behind the sartorius, pierces the fascia lata between the tendons of the sartorius and gracilis, and then becomes subcutaneous. From here, it descends on the medial side of the leg with the long saphenous vein. Note that the saphenous nerve divides into numerous small branches as it enters the subcutaneous space, and, as such, it is often difficult to achieve block of the entire extensive saphenous nerve network.

FIGURE 6. Tibial tuberosity. Palpation of the landmark for the saphenous nerve block.
Techniques
The below-knee field block is performed with the patient in the supine position. Five to 10 mL of local anesthetic is injected as a ring deeply subcutaneously, starting at the medial surface of the tibial condyle and ending at the dorsomedial aspect of the upper calf (Figure 8).
A perivenous technique has also been described, which is based on the close relation of the saphenous vein and nerve, to achieve a higher success rate. First, the saphenous vein is identified using a tourniquet around the leg in dependent position. The technique involves injection of 5 mL of local anesthetic in a fanlike fashion around the vein on the medial side of the leg just distal from the patella. This technique, however, carries a small risk of creating a hematoma if the saphenous vein is punctured.

FIGURE 8. Saphenous nerve block. Shown is a subcutaneous injection of 10 mL of local anesthetic in a circumferential fashion on the medial aspect of the leg at the level of the tibial tuberosity.
In the transsartorial approach, with the patient in the supine position, a skin wheal is raised over the sartorius muscle belly. The sartorius muscle can be palpated just above the knee with the leg extended and actively elevated. The needle is inserted at 1 finger-width above the patella slightly posterior to the coronal plane and slightly caudad through the muscle belly of the sartorius until a loss of resistance identifies the subsartorial adipose tissue. The depth of insertion is typically between 1.5 and 3.0 cm. After negative aspiration for blood, 10 mL of local anesthetic is injected.
For surgery on the foot, the saphenous nerve is best blocked just above the medial malleolus, similar to the technique in ankle block (Figure 9). Using a 1.5-in. needle, 6–8 mL of local anesthetic is injected subcutaneously immediately above the medial malleolus in a ring-like fashion. The most commonly reported complication of this block is a hematoma of the saphenous vein at the injection site.

FIGURE 9. Saphenous nerve block, distal approach above the medial malleolus.
The saphenous nerve can also be blocked by using a nerve stimulator technique and performing a low-volume femoral nerve block (see Femoral Nerve block). Injection of 10 mL of local anesthetic after obtaining either a medial muscle response, signified by contraction of the vastus medialis muscle, or an anterior muscle response, signified by contraction of the rectus femoris muscle and elevation of the patella, results in a high rate of block success.
Neurostimulation of the medial compartment of the femoral nerve requires even less volume of local anesthetic, compared with that of a standard femoral block.
NYSORA Tips
- The most effective method of blocking the saphenous nerve is a low-volume femoral nerve block.
- Injection of 10 mL of local anesthetic upon obtaining twitches of the patella or vastus medialis muscle results in a high success rate.
In a comparison of the different approaches to saphenous nerve block, the transsartorial approach resulted in 100% sensory block of the medial aspect of the leg, whereas the perifemoral and the below-knee field block were successful only in 70%. The medial femoral condyle block resulted in 40% of the patients having sensory block of the medial aspect of the leg with only 25% having complete anesthesia at the medial malleolus. This supported the findings of a previous study in which 94% of patients had complete anesthesia of the medial malleolus after a transsartorial saphenous nerve block. However, saphenous nerve often does not reach the level of the medial malleolus. The introduction of ultrasound-guided techniques and several studies supporting its use as an alternative to femoral block for total knee arthroplasty have greatly increased the interest in the transsartorial (or “adductor canal”) approach to the saphenous nerve.
SURAL NERVE BLOCK
General Considerations
The sural nerve block is used for superficial surgery on the lateral aspect of the ankle and foot and in conjunction with ankle block for foot and toe surgery.
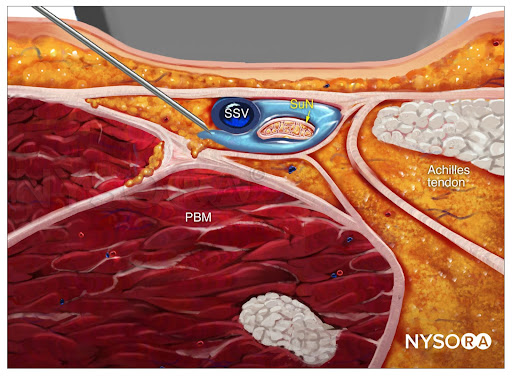
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for a sural nerve block with needle insertion in-plane and local anesthetic spread (blue). PBM, peroneus brevis muscle; SuN, sural nerve; SSV, small saphenous vein.
Distribution of Anesthesia
The sural nerve innervates the posterior and lateral skin of the distal third of the leg along the lateral side of the foot and little toe (see Figure 1).
Patient Positioning
For the block procedure, the patient can be positioned prone or supine with the ankle supported by a footrest.
Anatomic Landmarks
The sural nerve, a branch of the tibial nerve, pierces the deep fascia proximally in the leg and is joined by a branch of the common peroneal nerve. It descends near the lesser saphe-nous vein and between the lateral malleolus and the calcaneus.
Technique
Using a 1.5-in., 25-gauge needle, a skin wheal is raised lateral to the Achilles tendon and just above the lateral malleolus (Figure 10). The needle is then inserted through the wheal and advanced toward the fibula while injecting 6–8 mL of local anesthetic.

FIGURE 10. Sural nerve block.
SUPERFICIAL PERONEAL BLOCK
General Considerations
A superficial peroneal block is used alone or in combination with other blocks for foot surgery or ascending venography.
Distribution of Anesthesia
The superficial peroneal branches supply innervation to the dorsal skin of all the toes except that of the lateral side of the fifth and adjoining sides of the first and second toes (see Figures 1 and 2).
Anatomic Landmarks
The superficial peroneal nerve begins at the common peroneal bifurcation. It pierces the deep fascia in the distal third of the leg. It descends the leg adjacent to the extensor digitorum longus muscle, where it divides into terminal branches above the ankle.
Patient Positioning
For the block procedure, the patient can be positioned supine with the ankle supported by a footrest.
Technique
The superficial peroneal nerve is blocked immediately above and medial to the lateral malleolus. 5–10 mL of local anesthetic is injected to form a subcutaneous wheal from the extensor hallucis longus tendon to the anterior surface of the lateral malleolus (Figure 11).

FIGURE 11.Superficial peroneal block.
COMPLICATIONS
Few complications result from performing cutaneous nerve blocks of the lower extremity. Possible complications and suggestions for how to avoid them are outlined in Table 2.
TABLE 2. Possible complications from cutaneous nerve blocks of the lower extremity.
| Systemic toxicity of local anesthetic | • Risk is small and may be of concern only when higher volumes are used in conjunction with other high-volume major conduction blocks |
| Hematoma | • Avoid multiple needle insertions and insertion of the needle through superficial veins |
| Nerve injury | • Usually manifested as transient paresthesias or dysesthesias • Avoid injecting when high pressures on injection are felt or when the patient reports pain in the distribution of the nerve |
SUMMARY
There are many uses for cutaneous nerve blocks of the lower extremity in everyday clinical practice. These blocks are easy to perform and are nearly devoid of complications.
REFERENCES
- Hopkins P, Ellis F, Halsall P: Evaluation of local anaesthetic block of the lateral femoral cutaneous nerve. Anaesthesia 1991;46:95–96.
- Coad N: Postoperative analgesia following femoral-neck surgery: A comparison between 3 in 1 femoral nerve block and lateral cutaneous nerve block. Eur J Anaesthesiol 1991;8:287–290.
- Maccani R, Wedel D, Melton A, Gronert G: Femoral and lateral femoral cutaneous nerve block for muscle biopsies in children. Paediatr Anaesth 1995;5:223–227.
- Jones S, White A: Analgesia following femoral neck surgery. Lateral cutaneous nerve block as an alternative to narcotics in the elderly. Anaesthesia 1985;40:682–685.
- Hood G, Edbrooke D, Gerrish S: Postoperative analgesia after triple nerve block for fractured neck of femur. Anaesthesia 1991;46:
- Hughes P, Brown T: An approach to posterior femoral cutaneous nerve block. Anaesth Intensive Care 1986;14:350–351.
- Elmas C, Elmas Y, Gautschi P, Uehlinger P: Combined sciatic 3-in-1 block. Application in lower limb orthopedic surgery. Anaesthetist 1992;41:639–643.
- McNicol L: Lower limb blocks for children. Lateral cutaneous and femoral nerve blocks for postoperative pain relief in paediatric practice. Anaesthesia 1986;41:27–31.
- Wardrop P, Nishikawa H: Lateral cutaneous nerve of the thigh block as primary anaesthesia for harvesting skin grafts. Br J Plast Surg 1995;48:597–600.
- Brown T, Dickens D: A new approach to lateral cutaneous nerve of thigh block. Anaesth Intensive Care 1986;14:126–127.
- Vloka J, Hadzic A, Mulcare R, et al: Combined popliteal and posterior cutaneous nerve of the thigh blocks for short saphenous vein stripping in outpatients: an alternative to spinal anesthesia. J Clin Anesth 1997;9:618–622.
- De Mey J, Deruyck L, Cammu G, et al: A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med 2001;26:504–506.
- Comfort V, Lang S, Yip R: Saphenous nerve anaesthesia: a nerve stimulator technique. Can J Anaesth 1996;43:852–857.
- Mansour N: Subsartorial saphenous nerve block with the aid of nerve stimulator. Reg Anesth Pain Med 1993;18:266–268.
- Chassery C, Gilbert M, Minville V, et al: Neurostimulation does not increase the success rate of saphenous nerve blocks. Can J Anaesth 2005;52:269–275.
- Benzon H, Sharma S, Calimaran A: Comparison of the different approaches to saphenous nerve block. Anesthesiology 2005;102:633–638.
- van der Wal M, Lang S, Yip R: Transsartorial approach for saphenous nerve block. Can J Anaesth 1993;40:542–546.
- López AM1, Sala-Blanch X, Magaldi M, Poggio D, Asuncion J, Franco CD: Ultrasound-guided ankle block for forefoot surgery: the contribution of the saphenous nerve. Reg Anesth Pain Med. 2012 37(5):554-7.
- Jœger P, Zaric D, Fomsgaard JS, et al: Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med. 2013;38:526–532.
- Shah NA, Jain NP: Is Continuous Adductor Canal Block Better Than Continuous Femoral Nerve Block After Total Knee Arthroplasty? Effect on Ambulation Ability, Early Functional Recovery and Pain Control: A Randomized Controlled Trial. J Arthroplasty. 2014 Jun 19 [Epub ahead of print].
- Mussurakis S: Combined superficial peroneal and saphenous nerve block for ascending venography. Eur J Radiol 1992;14:56–59. 22. Lieberman R, Kaplan P: Superficial peroneal nerve block for leg venography. Radiology 1987;165:578–579.