Arthur Atchabahian, Catherine Vandepitte, and Ana M. Lopez
FACTS
- Indications: arm, elbow, forearm, and hand surgery (Figure 1)
- Transducer position: approximately parasagittal, just medial to the coracoid process, inferior to the clavicle
- Goal: local anesthetic spread around axillary artery
- Local anesthetic volume: 20–30 mL
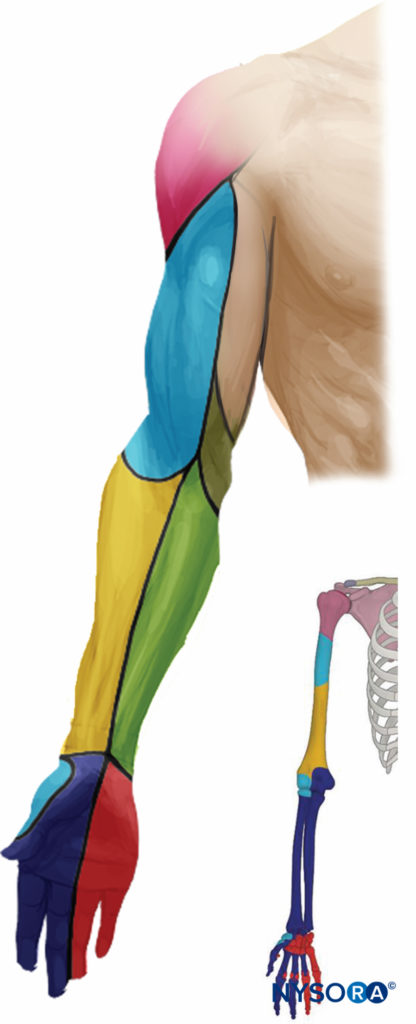
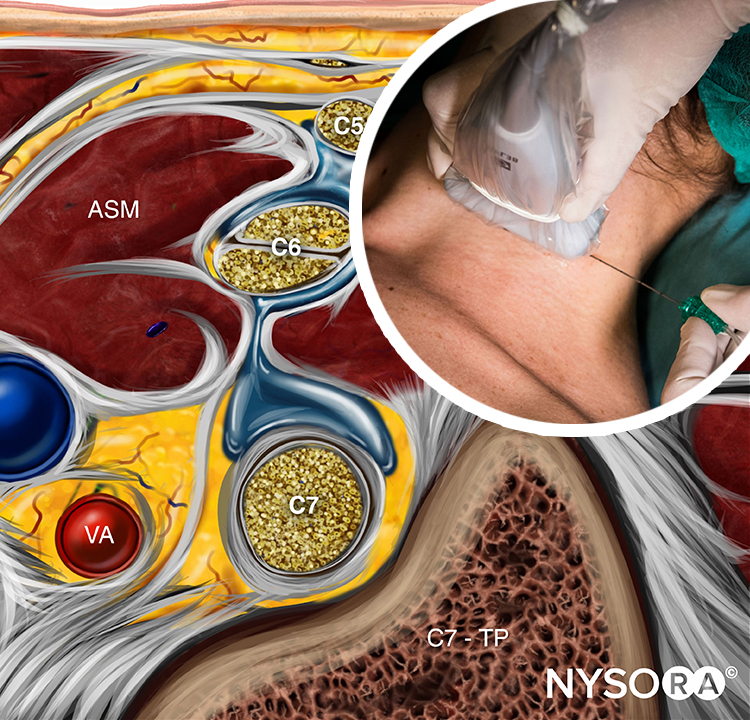
FIGURE 1. Distribution of sensory block of the infraclavicular brachial plexus nerve block.
GENERAL CONSIDERATIONS
The ultrasound (US)-guided infraclavicular brachial plexus nerve block is in some ways both simple and challenging. It is simple in that identification of the arterial pulse on the sonographic image is an easy primary goal in establishing the landmark. However, the plexus at this level is situated deeper, and the angle of approach is more acute, making simultaneous visualization of the needle and the relevant anatomy more challenging. Fortunately, although it is not always possible to reliably identify the three cords of the plexus, an adequate nerve block can be achieved by simply depositing the local anesthetic in a U shape around the artery. The infraclavicular brachial plexus nerve block is well suited for the catheter technique because the musculature of the chest wall helps stabilize the catheter and prevents its dislodgement compared with the more superficial location used with the interscalene and supraclavicular approaches to brachial plexus block.
ULTRASOUND ANATOMY
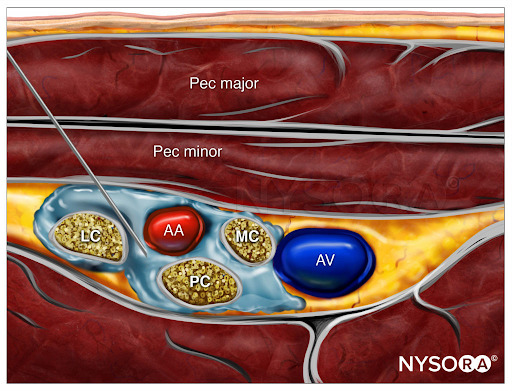
The axillary artery can be identified deep to the pectoralis major and minor muscles. An effort needs to be made to obtain clear views of both pectoralis muscles and their respective fasciae. This is important because the area of interest lies underneath the fascia of the pectoralis minor muscle. Surrounding the artery are the three cords of the brachial plexus: the lateral, posterior, and medial cords. These are named for their usual position relative to the axillary artery, although there is a great deal of anatomical variation. With the left side of the screen corresponding to the cephalad aspect, the cords can often be seen as round hyperechoic structures at the positions of approximately 9 o’clock (lateral cord), 7 o’clock (posterior cord), and 5 o’clock (medial cord) (Figures 2 and 3). The axillary vein is seen as a compressible hypoechoic structure that lies medially to the axillary artery. Multiple other, smaller vessels (eg, the cephalic vein) are often present as well. The transducer is moved in the cephalad-caudad and medial-lateral direction until the artery is identified in cross-section. Depending on the depth selected and the level at which the scanning is performed, the chest wall and the pleura may be seen in the medial and more caudal aspect of the image. The axillary artery and/or brachial plexus are typically identified at a depth of 3–5 cm in average-size patients.
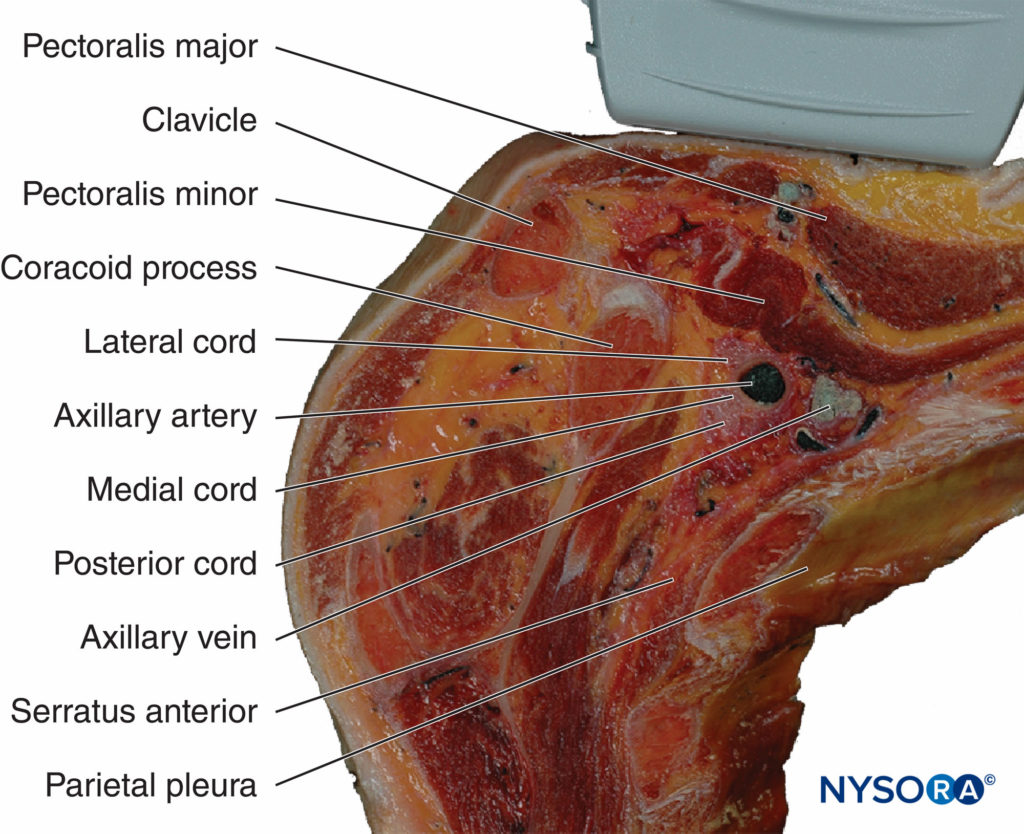
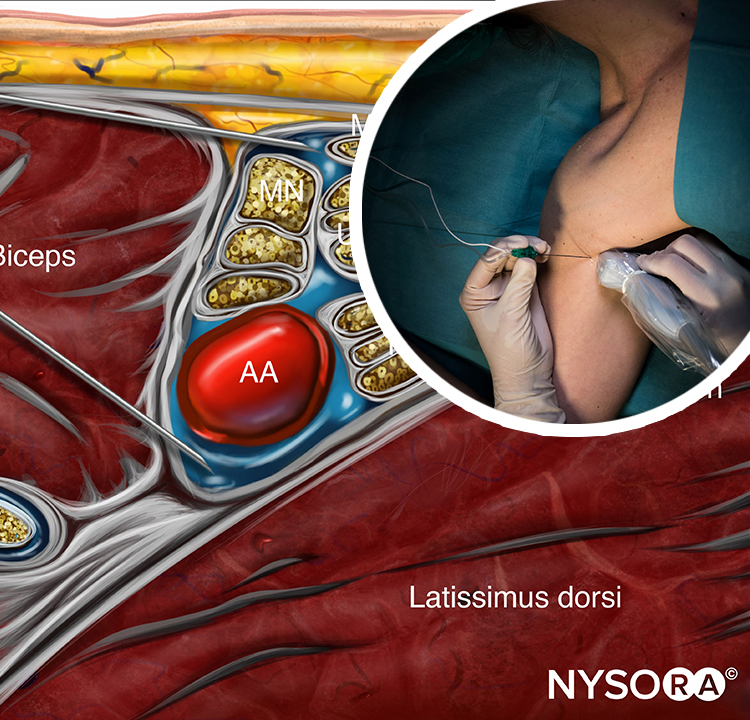
FIGURE 2. Anatomy of the infraclavicular brachial plexus (BP) and the position of the transducer. Paramedian sagittal plane at the level of the coracoid process. The BP is seen surrounding the axillary artery (AA) underneath the coracoid process and pectoralis minor muscle (PMiM). Note that the injection of local anesthetic should take place below the fascia of the PMiM to spread around the AA.
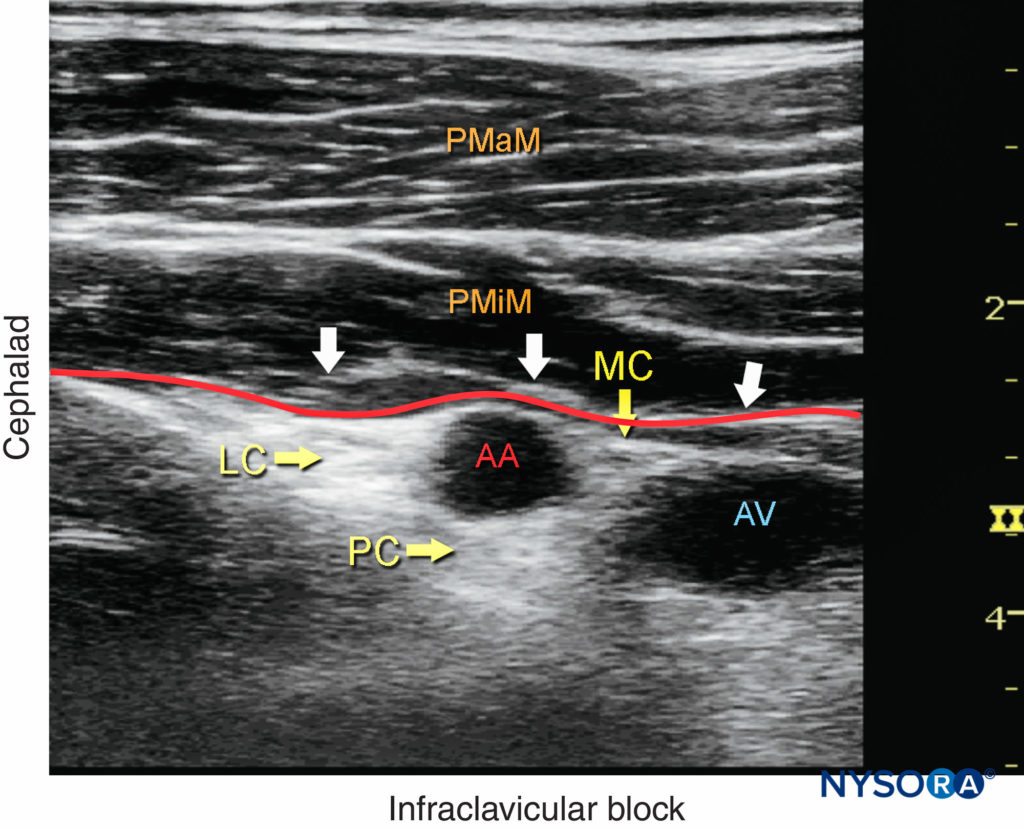
FIGURE 3. Ultrasound image of the brachial plexus (BP) distal to the clavicle. Note that the BP, axillary artery (AA) and axillary vein (AV) are located below the fascia (red line) of the pectoralis minor muscle (PMiM). LC, lateral cord; MC, medial cord; PC, posterior cord; PMaM, pectoralis major muscle.
From the Compendium of Regional Anesthesia: Cognitive priming for an infraclavicular brachial plexus block.
For a more comprehensive review of the brachial plexus, see Functional Regional Anesthesia Anatomy.
DISTRIBUTION OF ANESTHESIA
The infraclavicular approach to brachial plexus block results in anesthesia of the upper limb below the shoulder. If required, the skin of the medial aspect of the upper arm (intercostobrachial nerve, T2) can be blocked by an additional subcutaneous injection on the medial aspect of the arm just distal to the axilla. A simpler approach is for surgeons to infiltrate the skin with the local anesthetic directly over the incision line as needed.
EQUIPMENT
The equipment recommended for an infraclavicular brachial plexus nerve block includes the following:
- Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel
- Standard nerve block tray
- 20–30 mL of local anesthetic drawn up in syringes
- 8- to 10-cm, 21- to 22-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Opening injection pressure monitoring system
- Sterile gloves
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
Any position that allows for the comfortable placement of the ultrasound transducer and needle advancement is appropriate. The nerve block is typically performed with the patient in the supine position with the head turned away from the side to be blocked (Figure 4). The arm is abducted to 90 degrees and the elbow flexed. This maneuver raises the clavicle, reduces the depth from the skin to the plexus, and substantially facilitates visualization of the pectoralis muscles as well as the cords of the brachial plexus and the needle. The coracoid process is an important landmark and can be easily identified by palpating the bony prominence just medial to the shoulder while the arm is elevated and lowered. As the arm is lowered, the coracoid process meets the fingers of the palpating hand. Scanning usually begins just medial to the coracoid process and inferior to the clavicle. Keeping the probe in a parasagittal plane, scanning medially and laterally allows the chest wall and pleura to be located (Figure 5). The nerve block should be performed with the probe lateral to the pleura in order to minimize the risk of pneumothorax.
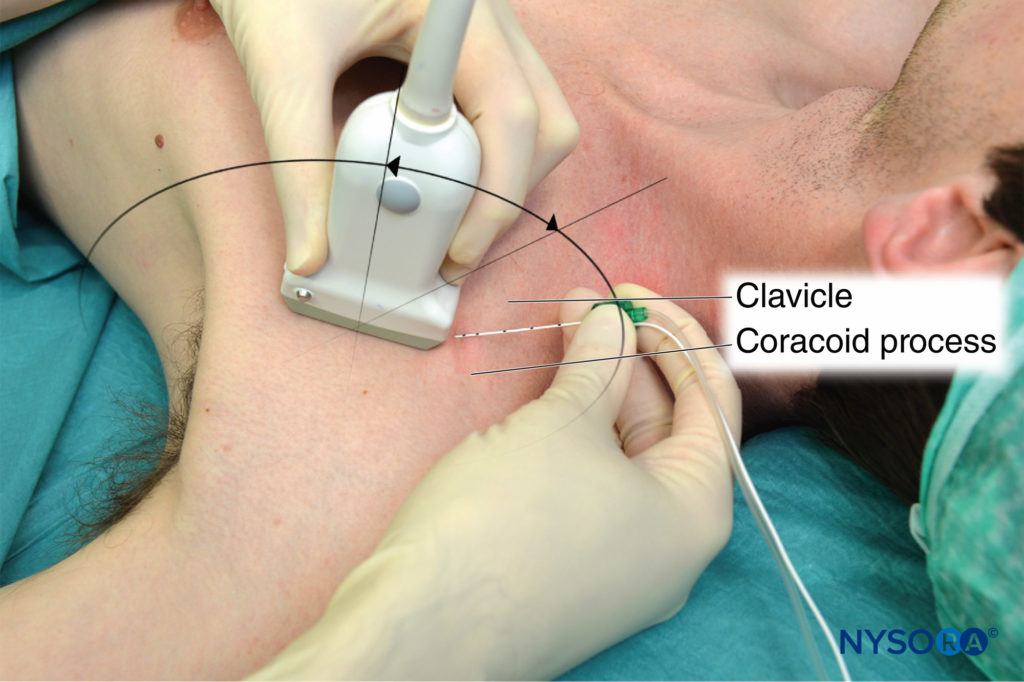
FIGURE 4. Patient position for infraclavicular brachial plexus nerve block needle insertion. The transducer is positioned parasagittally just medial to the coracoid process and inferior to the clavicle.
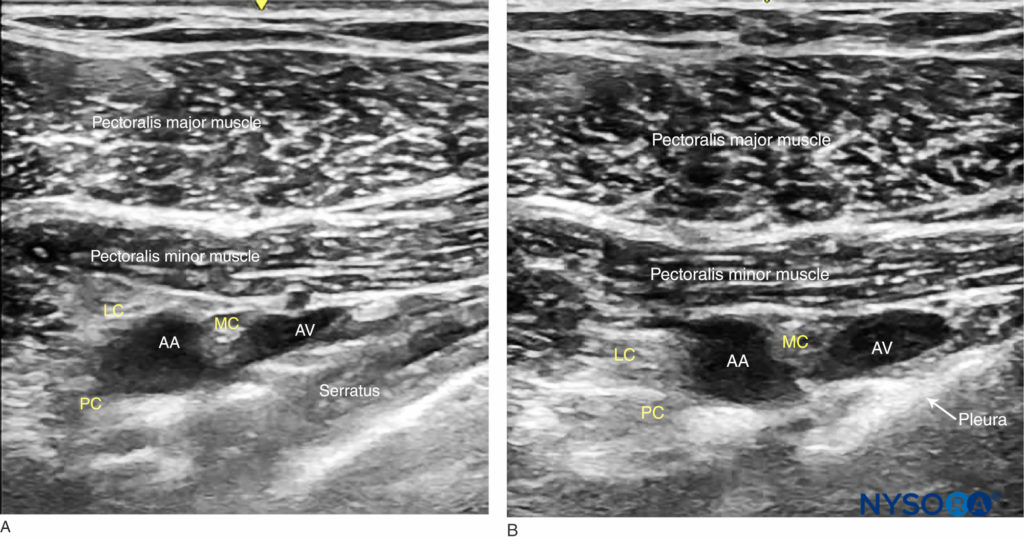
FIGURE 5. Ultrasound-guided infraclavicular nerve block: a medial-to-lateral probe movement is used to avoid the area where the needle advanced in the parasagittal plane could enter the pleura. (A) Parasagittal lateral view: the serratus anterior is seen between the neurovascular bundle and the pleura. (B) In this probe position, the pleura lies closer to the brachial plexus.
GOAL
The goal of the technique is to inject local anesthetic until the spread around the artery is verified by ultrasound. It is not necessary to identify and target individual cords. Instead, injection of local anesthetic to surround the artery in an U-shaped pattern (cephalad, caudad, and posterior) suffices for the nerve block of all three cords.
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for an infraclavicular brachial plexus block with needle insertion in-plane and local anesthetic spread (blue). AA, axillary artery; AV, axillary vein; LC, lateral cord; MC, medial cord; PC, posterior cord.
TECHNIQUE
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the parasagittal plane to identify the axillary artery (see Figure 3 and 4). This may require adjustment of the depth, depending on the thickness of the patient’s chest wall musculature. The axillary artery is typically seen between 3 and 5 cm. Once the artery has been identified, an attempt is made to identify the hyperechoic cords of the brachial plexus and their corresponding positions relative to the artery, although these may not always be identifiable. Fortunately, visualization of the cords are not necessary for successful block. The needle is inserted in-plane from the cephalad end of the probe, with the insertion point just inferior to the clavicle (see Figure 4). The needle is aimed toward the posterior aspect of the axillary artery and passes through the pectoralis major and minor muscles. If nerve stimulation is used concurrently (0.5–0.8 mA, 0.1 msec), the first motor response is often from the lateral cord (either elbow flexion or finger flexion). As the needle is advanced farther beneath the artery, a posterior cord motor response may appear (finger and wrist extension). After careful aspiration, 1–2 mL of local anesthetic is injected to confirm proper needle placement and spread. The injectate should spread cephalad and caudad to cover the lateral and medial cords, respectively (Figure 6).
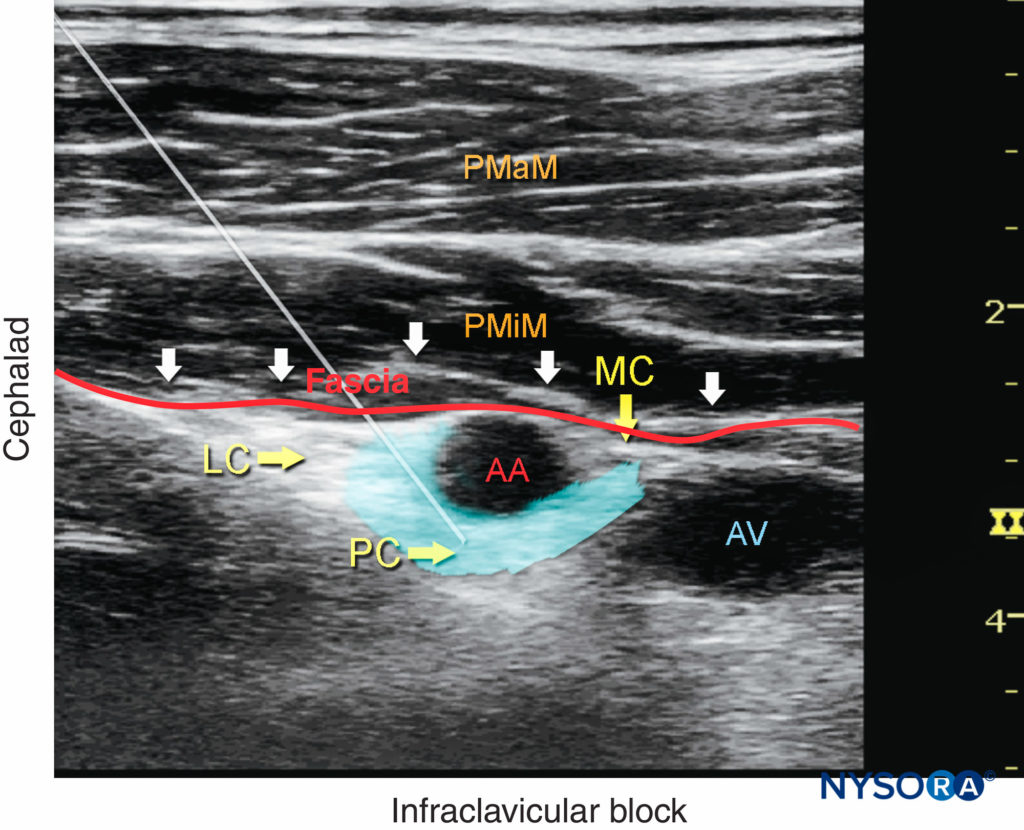
FIGURE 6. Ultrasound image demonstrating an ideal needle path for the infraclavicular brachial plexus nerve block. The blue-shaded area mimics an ideal spread of local anesthetic around the axillary artery (AA) and reaches all three cords of the brachial plexus (the lateral cord [LC], posterior cord [PC], and medial cord [MC]) below the fascia (red line) of the pectoralis minor muscle (PMiM), pectoralis major muscle (PMaM), and axillary vein (AV).
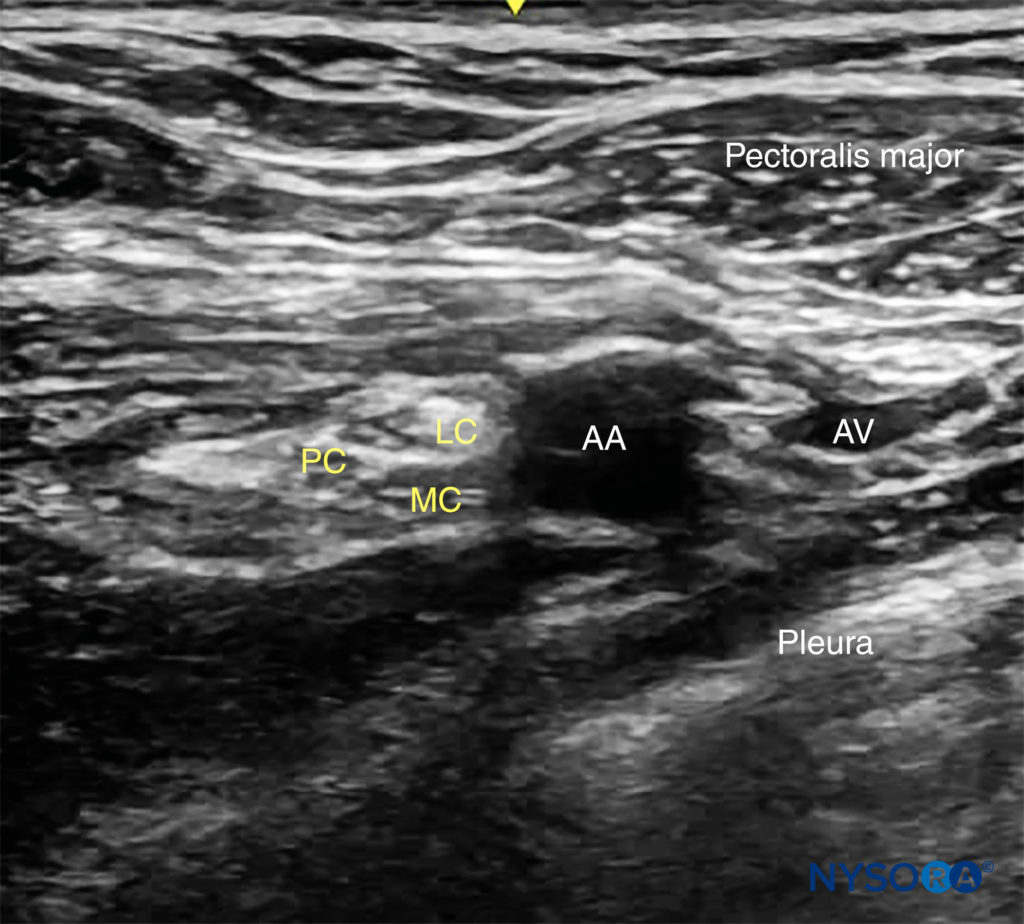
FIGURE 7. Ultrasound view of the brachial plexus at the costoclavicular space. The lateral (LC), medial (MC) and posterior (PC) cords are clustered together lateral to the axillary artery lying more superficial. At this level, the pectoralis minor is not seen deep to the pectoralis major.
TIPS
• An artifact posterior to the artery is often misinterpreted as the posterior cord. Figure 6.
• A “heel-up” maneuver (rocking the probe toward the patient’s head in a parasagittal plane, depressing the tissues caudad to the probe) makes it easier to change the needle’s angle as needed (see Figure 4).
• To decrease the risk of complications, adhere to the following guidelines:
• Aspirate intermittently every 5 mL to decrease the risk of intravascular injection.
• Do not inject if the injection resistance is high (> 15 psi).
CONTINUOUS ULTRASOUND-GUIDED INFRACLAVICULAR NERVE BLOCK
The goal of the continuous infraclavicular nerve block is similar to the non–ultrasound-based techniques: to place the catheter within the vicinity of the cords of the brachial plexus beneath the pectoral muscles. The procedure consists of three phases: (1) needle placement; (2) catheter advancement; and (3) securing the catheter. For the first two phases of the procedure, ultrasound can be used to ensure accuracy in most patients. The needle is typically inserted in-plane from the cephalad to caudad direction, similar to the single-injection technique (Figure 8). As with the single-injection technique, the needle tip should be placed posterior to the axillary artery prior to injection and catheter advancement. Proper needle placement can also be confirmed by obtaining a motor response of the posterior cord (finger or wrist extension), at which point 1–2 mL of local anesthetic is injected. The rest of the technique, advancing and securing the catheter is the same as previously described (continuous nerve block section, Ultrasound-Guided Interscalene Brachial Plexus Nerve Block). A typical starting infusion regimen is 5 mL/h, followed by 8-mL patient-controlled boluses every hour. The larger bolus volume is necessary for the adequate spread of the injectate around the artery so that all cords of the brachial plexus are reached.

FIGURE 8. The patient position, imaging, and needle placement for continuous infraclavicular brachial plexus nerve block are similar to those for a single-injection technique. Once proper needle tip placement is determined by the injection of a small volume of local anesthetic, the catheter is inserted 2–4 cm beyond the needle tip.
Follow the link to Continuous Peripheral Nerve Blocks for additional information.
REFERENCES
- Ruiz A, Sala X, Bargallo X, Hurtado P, Arguis MJ, Carrera A: The influence of arm abduction on the anatomic relations of infraclavicular brachial plexus: an ultrasound study. Anesth Analg 2009;108:364–366.
- Auyong DB, Gonzales J, Benonis JG: The Houdini clavicle: arm abduction and needle insertion site adjustment improves needle visibility for the infraclavicular nerve block. Reg Anesth Pain Med 2010;35:403–404.
- Fredrickson MJ, Wolstencroft P, Kejriwal R, Yoon A, Boland MR, Chinchanwala S: Single versus triple injection ultrasound-guided infraclavicular block: confirmation of the effectiveness of the single injection technique. Anesth Analg 2010;111:1325–1327.
- Tran DQ, Bertini P, Zaouter C, Muñoz L, Finlayson RJ: A prospective, randomized comparison between single- and double-injection ultrasoundguided infraclavicular brachial plexus block. Reg Anesth Pain Med 2010;35:16–21.
- Desgagnés MC, Lévesque S, Dion N, et al: A comparison of a single or triple injection technique for ultrasound-guided infraclavicular block: a prospective randomized controlled study. Anesth Analg 2009;109:668–672
- Dolan J: Fascial planes inhibiting the spread of local anesthetic during ultrasound-guided infraclavicular brachial plexus block are not limited to the posterior aspect of the axillary artery. Reg Anesth Pain Med 2009; 34:612–613
- Morimoto M, Popovic J, Kim JT, Kiamzon H, Rosenberg AD: Case series: septa can influence local anesthetic spread during infraclavicular brachial plexus blocks. Can J Anaesth 2007;54:1006–1010.
- Aguirre J, Baulig B, Borgeat A: Does ultrasound-guided infraclavicular block meet users’ expectations? Can J Anaesth 2010;57:176–177.
- Akyildiz E, Gurkan Y, Caglayan C, Solak M, Toker K: Single vs. double stimulation during a lateral sagittal infraclavicular block. Acta Anaesthesiol Scand 2009;53:1262–1267.
- Arcand G, Williams SR, Chouinard P, et al: Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg 2005;101:886–890.
- Benkhadra M, Faust A, Fournier R, Aho LS, Girard C, Feigl G: Possible explanation for failures during infraclavicular block: an anatomical observation on Thiel’s embalmed cadavers. Br J Anaesth 2012;109: 128–129.
- Berry JM: Selective local anesthetic placement using ultrasound guidance and neurostimulation for infraclavicular brachial plexus block. Anesth Analg 2010;110:1480–1485.
- Bigeleisen P, Wilson M: A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth 2006;96:502–507.
- Bigeleisen PE: Ultrasound-guided infraclavicular block in an anticoagulated and anesthetized patient. Anesth Analg 2007;104:1285–1287.
- Bloc S, Garnier T, Komly B, et al: Spread of injectate associated with radial or median nerve-type motor response during infraclavicular brachial-plexus block: an ultrasound evaluation. Reg Anesth Pain Med 2007;32:130–135.
- Bowens C Jr, Gupta RK, O’Byrne WT, et al: Selective local anesthetic placement using ultrasound guidance and neurostimulation for infraclavicular brachial plexus block. Anesth Analg 2010;110:1480–1485.
- Brull R, Lupu M, Perlas A, Chan VW, McCartney CJ: Compared with dual nerve stimulation, ultrasound guidance shortens the time for infraclavicular block performance. Can J Anaesth 2009;56:812–818.
- Brull R, McCartney CJ, Chan VW: A novel approach to infraclavicular brachial plexus block: the ultrasound experience. Anesth Analg 2004;99:950.
- Chin KJ, Alakkad H, Adhikary SD, Singh M: Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Cochrane Database Syst Rev 2013;8:CD005487.
- Chin KJ, Singh M, Velayutham V, Chee V: Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Anesth Analg 2010;111:1072.
- Chin KJ, Singh M, Velayutham V, Chee V: Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Cochrane Database Syst Rev 2010;2:CD005487.
- Dhir S, Ganapathy S: Comparative evaluation of ultrasound-guided continuous infraclavicular brachial plexus block with stimulating catheter and traditional technique: a prospective-randomized trial. Acta Anaesthesiol Scand 2008;52:1158–1166.
- Dhir S, Ganapathy S: Use of ultrasound guidance and contrast enhancement: a study of continuous infraclavicular brachial plexus approach. Acta Anaesthesiol Scand 2008;52:338–342.
- Dhir S, Singh S, Parkin J, Hannouche F, Richards RS: Multiple finger joint replacement and continuous physiotherapy using ultrasound guided, bilateral infraclavicular catheters for continuous bilateral upper extremity analgesia. Can J Anaesth 2008;55:880–881.
- Dingemans E, Williams SR, Arcand G, et al: Neurostimulation in ultrasoundguided infraclavicular block: a prospective randomized trial. Anesth Analg 2007;104:1275–1280.
- Dolan J: Fascial planes inhibiting the spread of local anesthetic during ultrasound-guided infraclavicular brachial plexus block are not limited to the posterior aspect of the axillary artery. Reg Anesth Pain Med 2009;34:612–613.
- Dolan J: Ultrasound-guided infraclavicular nerve block and the cephalic vein. Reg Anesth Pain Med 2009;34:528–529.
- Eren G, Altun E, Pektas Y, et al: To what extent can local anesthetics be reduced for infraclavicular block with ultrasound guidance? Anaesthesist 2014;63:760–765.
- Fredrickson MJ, Patel A, Young S, Chinchanwala S: Speed of onset of “corner pocket supraclavicular” and infraclavicular ultrasound guided brachial plexus block: a randomised observer-blinded comparison. Anaesthesia 2009;64:738–744.
- Gleeton D, Levesque S, Trépanier CA, Gariépy JL, Brassard J, Dion N: Symptomatic axillary hematoma after ultrasound-guided infraclavicular block in a patient with undiagnosed upper extremity mycotic aneurysms. Anesth Analg 2010;111:1069–1071.
- Gurkan Y, Acar S, Solak M, Toker K: Comparison of nerve stimulation vs. ultrasound-guided lateral sagittal infraclavicular block. Acta Anaesthesiol Scand 2008;52:851–855.
- Gurkan Y, Ozdamar D, Hosten T, Solak M, Toker K: Ultrasound guided lateral sagittal infraclavicular block for pectoral flap release. Agri 2009;21:39–42.
- Gurkan Y, Tekin M, Acar S, Solak M, Toker K: Is nerve stimulation needed during an ultrasound-guided lateral sagittal infraclavicular block? Acta Anaesthesiol Scand 2010;54:403–407.
Jiang XB, Zhu SZ, Jiang Y, Chen QH, Xu XZ: Optimal dose of local anesthetic mixture in ultrasound-guided infraclavicular brachial plexus block via coracoid approach: analysis of 160 cases [in Chinese]. Zhonghua Yi Xue Za Zhi 2009;89:449–452. - Kalagara HK, Uppal V, McKinlay S, Macfarlane AJ, Anderson K: Effect of body mass index on angle of needle insertion during ultrasound-guided lateral sagittal infraclavicular brachial plexus block. J Clin Anesth 2015; ž27:375–379.
- Karmakar MK, Sala-Blanch X, Songthamwat B, Tsui BC: Benefits of the costoclavicular space for ultrasound-guided infraclavicular brachial plexus block: description of a costoclavicular approach. Reg Anesth Pain Med 2015;40:287–288.
- Koscielniak-Nielsen ZJ, Frederiksen BS, Rasmussen H, Hesselbjerg L: A comparison of ultrasound-guided supraclavicular and infraclavicular blocks for upper extremity surgery. Acta Anaesthesiol Scand 2009;53:620–626.
- Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L: Pneumothorax after an ultrasound-guided lateral sagittal infraclavicular block. Acta Anaesthesiol Scand 2008;52:1176–1177.
- Lecours M, Lévesque S, Dion N, Nadeau MJ, Dionne A, Turgeon AF: Complications of single-injection ultrasound-guided infraclavicular block: a cohort study. Can J Anaesth 2013;60:244–252.
- Levesque S, Dion N, Desgagne MC: Endpoint for successful, ultrasoundguided infraclavicular brachial plexus block. Can J Anaesth 2008;55:308.
- Marhofer P, Harrop-Griffiths W, Willschke H, Kirchmair L: Fifteen years of ultrasound guidance in regional anaesthesia: part 2—recent developments in block techniques. Br J Anaesth 2010;104:673–683.
- Mariano ER, Loland VJ, Bellars RH, et al: Ultrasound guidance versus electrical stimulation for infraclavicular brachial plexus perineural catheter insertion. J Ultrasound Med 2009;28:1211–1218.
- Martinez Navas A, De La Tabla Gonzalez RO: Ultrasound-guided technique allowed early detection of intravascular injection during an infraclavicular brachial plexus block. Acta Anaesthesiol Scand 2009;53:968–970.
- Moayeri N, Renes S, van Geffen GJ, Groen GJ: Vertical infraclavicular brachial plexus block: needle redirection after elicitation of elbow flexion. Reg Anesth Pain Med 2009;34:236–241.
- Morimoto M, Popovic J, Kim JT, Kiamzon H, Rosenberg AD: Case series: septa can influence local anesthetic spread during infraclavicular brachial plexus blocks. Can J Anaesth 2007;54:1006–1010.
- Nadig M, Ekatodramis G, Borgeat A: Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth 2003;90:107–108.
- Ootaki C, Hayashi H, Amano M: Ultrasound-guided infraclavicular brachial plexus block: an alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med 2000;25:600–604.
- Perlas A, Chan VW, Simons M: Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiology 2003;99:429–435.
- Ponde V, Shah D, Johari A: Confirmation of local anesthetic distribution by radio-opaque contrast spread after ultrasound guided infraclavicular catheters placed along the posterior cord in children: a prospective analysis. Paediatr Anaesth 2015;25:253–257.
- Ponde VC, Diwan S: Does ultrasound guidance improve the success rate of infraclavicular brachial plexus block when compared with nerve stimulation in children with radial club hands? Anesth Analg 2009;108: 1967–1970.
- Porter JM, McCartney CJ, Chan VW: Needle placement and injection posterior to the axillary artery may predict successful infraclavicular brachial plexus block: a report of three cases. Can J Anaesth 2005;52: 69–73.
- Punj J, Joshi A, Darlong V, Pandey R: Ultrasound characteristics of spread during infraclavicular plexus block. Reg Anesth Pain Med 2009;34:73.
- Renes S, Clark L, Gielen M, Spoormans H, Giele J, Wadhwa A: A simplified approach to vertical infraclavicular brachial plexus block using handheld Doppler. Anesth Analg 2008;106:1012–1014.
- Sahin L, Gul R, Mizrak A, et al: Ultrasound-guided infraclavicular brachial plexus block enhances postoperative blood flow in arteriovenous fistulas. J Vasc Surg 2011;54:749–753.
- Sala-Blanch, Reina MA, Pangthipampai P, Karmakar MK. Anatomic Basis for Brachial Plexus Block at the Costoclavicular Space A Cadaver Anatomic Study. Reg Anesth Pain Med 2016;41:387–391.
- Sandhu NS, Capan LM: Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth 2002;89:254–259.
- Sandhu NS, Maharlouei B, Patel B, Erkulwater E, Medabalmi P: Simultaneous bilateral infraclavicular brachial plexus blocks with low-dose lidocaine using ultrasound guidance. Anesthesiology 2006;104:199–201.
- Sandhu NS, Sidhu DS, Capan LM: The cost comparison of infraclavicular brachial plexus block by nerve stimulator and ultrasound guidance. Anesth Analg 2004;98:267–268.
- Sauter AR, Dodgson MS, Stubhaug A, Halstensen AM, Klaastad O: Electrical nerve stimulation or ultrasound guidance for lateral sagittal infraclavicular blocks: a randomized, controlled, observer-blinded, comparative study. Anesth Analg 2008;106:1910–1915.
- Sauter AR, Smith HJ, Stubhaug A, Dodgson MS, Klaastad O: Use of magnetic resonance imaging to define the anatomical location closest to all three cords of the infraclavicular brachial plexus. Anesth Analg 2006;103: 1574–1576.
- Slater ME, Williams SR, Harris P, et al: Preliminary evaluation of infraclavicular catheters inserted using ultrasound guidance: through-the-catheter anesthesia is not inferior to through-the-needle blocks. Reg Anesth Pain Med 2007;32:296–302.
- Taboada M, Rodriguez J, Amor M, et al: Is ultrasound guidance superior to conventional nerve stimulation for coracoid infraclavicular brachial plexus block? Reg Anesth Pain Med 2009;34:357–360.
- Tedore TR, YaDeau JT, Maalouf DB, et al: Comparison of the transarterial axillary block and the ultrasound-guided infraclavicular block for upper extremity surgery: a prospective randomized trial. Reg Anesth Pain Med 2009;34:361–365.
- Trabelsi W, Amor MB, Lebbi MA, Romdhani C, Dhahri S, Ferjani M: Ultrasound does not shorten the duration of procedure but provides a faster sensory and motor block onset in comparison to nerve stimulator in infraclavicular brachial plexus block. Korean J Anesthesiol 2013;64:327–333.
- Tran DQ, Bertini P, Zaouter C, Muñoz L, Finlayson RJ: A prospective, randomized comparison between single- and double-injection ultrasoundguided infraclavicular brachial plexus block. Reg Anesth Pain Med 2010;35:16–21.
- Tran DQ, Charghi R, Finlayson RJ: The “double bubble” sign for successful infraclavicular brachial plexus block. Anesth Analg 2006;103:1048–1049.
- Tran DQ, Clemente A, Tran DQ, Finlayson RJ: A comparison between ultrasound-guided infraclavicular block using the “double bubble” sign and neurostimulation-guided axillary block. Anesth Analg 2008;107:1075–1078.
- Tran DQ, Dugani S, Dyachenko A, Correa JA, Finlayson RJ: Minimum effective volume of lidocaine for ultrasound-guided infraclavicular block. Reg Anesth Pain Med 2011;36:190–194.
- Tran DQ, Russo G, Muñoz L, Zaouter C, Finlayson RJ: A prospective, randomized comparison between ultrasound-guided supraclavicular, infraclavicular, and axillary brachial plexus blocks. Reg Anesth Pain Med 2009;34:366–371.
- Yazer MS, Finlayson RJ, Tran DQ: A randomized comparison between infraclavicular block and targeted intracluster injection supraclavicular block. Reg Anesth Pain Med 2015;40:11–15.
Additional reading: Infraclavicular Brachial Plexus Block – Landmarks and Nerve Stimulator Technique