Jennifer E. Dominguez and Thomas M. Halaszynski
INTRODUCTION AND DEFINITION OF ELDERLY
Healthcare providers have become increasingly focused on providing effective management of acute perioperative pain in all patients, but especially older adults, as the size of this patient population has steadily increased in recent years. Advances in anesthetic and surgical techniques, an improved understanding of the pathophysiology of pain, the development of new opioid and nonopioid analgesic drugs, the incorporation of regional techniques that reduce or eliminate reliance on traditional opioid analgesics, and novel methods of drug delivery have all led to greater numbers of older patients undergoing major surgery. An increased prevalence of chronic medical conditions among older individuals may also lead to higher degrees of acute and chronic pain (including acute-on-chronic pain). For instance, acute exacerbations of arthritis, osteoporotic fractures of the spine, cancer pain, and pain from acute medical conditions (eg, ischemic heart disease, herpes zoster, peripheral vascular disease) must be properly addressed in order to maximize multimodal perioperative pain management. In addition, older individuals are adopting more active lifestyles that can predispose them to trauma and orthopedic injuries that require surgery.
The term elderly encompasses both chronologic and physiologic factors. Chronologic age is the actual number of years an individual has lived, whereas physiologic age refers to functional capacity or reserve within organ systems defined in pathophysiologic parameters. The chronologic component can be divided into two separate groups: the “young old” (65 to 80 years of age) and the “older old” (greater than 80 years of age). Physiologic reserve describes the functional capacity of organ systems to compensate for acute stress and traumatic derangements. When present, comorbid disease states such as diabetes mellitus, arthritis, renal insufficiency, ischemic heart disease, and chronic obstructive pulmonary disease (COPD) can all decrease a patient’s physiologic reserve making it difficult for him or her to recover from traumatic or surgical injury.
There are a host of additional factors that may compromise the ability to provide optimal and effective acute pain management to older patients. A consequence of the comorbid diseases that afflict this patient population with increased frequency is the medications used in treatments for such diseased conditions, along with a subsequent increased risk of drug-to-drug and disease-to-drug interactions. An improved understanding of age-related changes in physiology, pharmacodynamics, and pharmacokinetics must be incorporated into any acute pain medicine care plan for older individuals. Altered responses to pain among the elderly population along with difficulties in pain assessment for certain individuals with cognitive dysfunction are potential problems that must also be considered.
Several theories have been advocated to describe the multidimensional aspects and consequences of aging that underscore the complexities and difficulties encountered in developing optimal regional anesthetic and analgesic choices for elderly patients. Therefore, the focus of this chapter is to outline the physiologic and pharmacologic implications of aging on surgical anesthesia and acute pain management, as well as the potential risks and benefits of neuraxial block along with peripheral nerve/nerve plexus block in geriatric patients.
PHYSIOLOGIC CHANGES ASSOCIATED WITH AGING AND CONSIDERATIONS FOR REGIONAL ANESTHESIA/ANALGESIA
Aging is characterized by progressive reductions in the homeo-static reserves of nearly every organ system. Declining organ function, often referred to as homeostenosis, may be gradual or progressive and becomes evident by the third decade of life. The compromised function of each organ system generally occurs independent of changes to other organ systems and may be influenced by a host of factors, including diet, environment, habits, and genetic predisposition. Optimal anesthetic management using regional techniques in elderly patients depends upon a knowledge and understanding of normal age-related changes in anatomy, physiology, and response to pharmacologic agents. It is also important to distinguish normal physiologic alterations of the central nervous system (CNS), cardiovascular, pulmonary, and hepatorenal systems from disease-related pathophysiologic changes.
NYSORA Tips
- The pain thresholds to a variety of noxious stimuli are altered in older individuals.
- Older patients have a reduction in pain tolerance.
- Patient-controlled analgesia (PCA) and epidural analgesia are more effective in elderly patients than most other conventional (PO and IM) opioid analgesic regimens.
- Physiologic changes associated with aging vary markedly among individuals. The administration of pain medica-tions warrants a decrease in dose (maintenance and/or bolus) of drug required for analgesia to avoid the risk of increased plasma drug accumulation and accumulation of active metabolites.
Nervous System Function
Aging results in anatomical and biochemical changes of the brain, spinal cord, and peripheral nervous system (PNS) that result in qualitative and quantitative alterations in function (Table 1). In addition, advanced age can be associated with decreased brain volume, a manifestation of the loss of neurons, as well as a reduction in cerebral white matter nerve fibers. Specifically, the number of cholinergic and dopaminergic neurons declines, and morphologic changes in neuronal fibers occur that result in fewer synaptic contacts and neuroreceptors.
TABLE 1. Physiologic central nervous system changes associated with aging and eects on pharmacokinetic variables.
| Physiologic Process | Magnitude of Change | Variable Kinetic/Dynamic Consequences | General Dosing Strategy |
|---|---|---|---|
| Cerebral blood flow, metabolism, and volume | ↓ 20% ↓ 20% | ↓ distribution to the CNS ↓ apparent volume in the CNS | Little net effect on drug dose |
| Active blood–brain barrier transport (efflux) | Drug-specific ↓ | ↑ apparent volume in the CNS | ↓ bolus dose during drug titration ↓ maintenance dose |
| Pain threshold sensitivity | Little change | ↑ apparent sensitivity of the CNS | Need for titration is unchanged |
| Concentration response (opioids) | ↑ 50% for some opioids | ↑ response to opioids | ↓ bolus dose during titration ↓ maintenance dose |
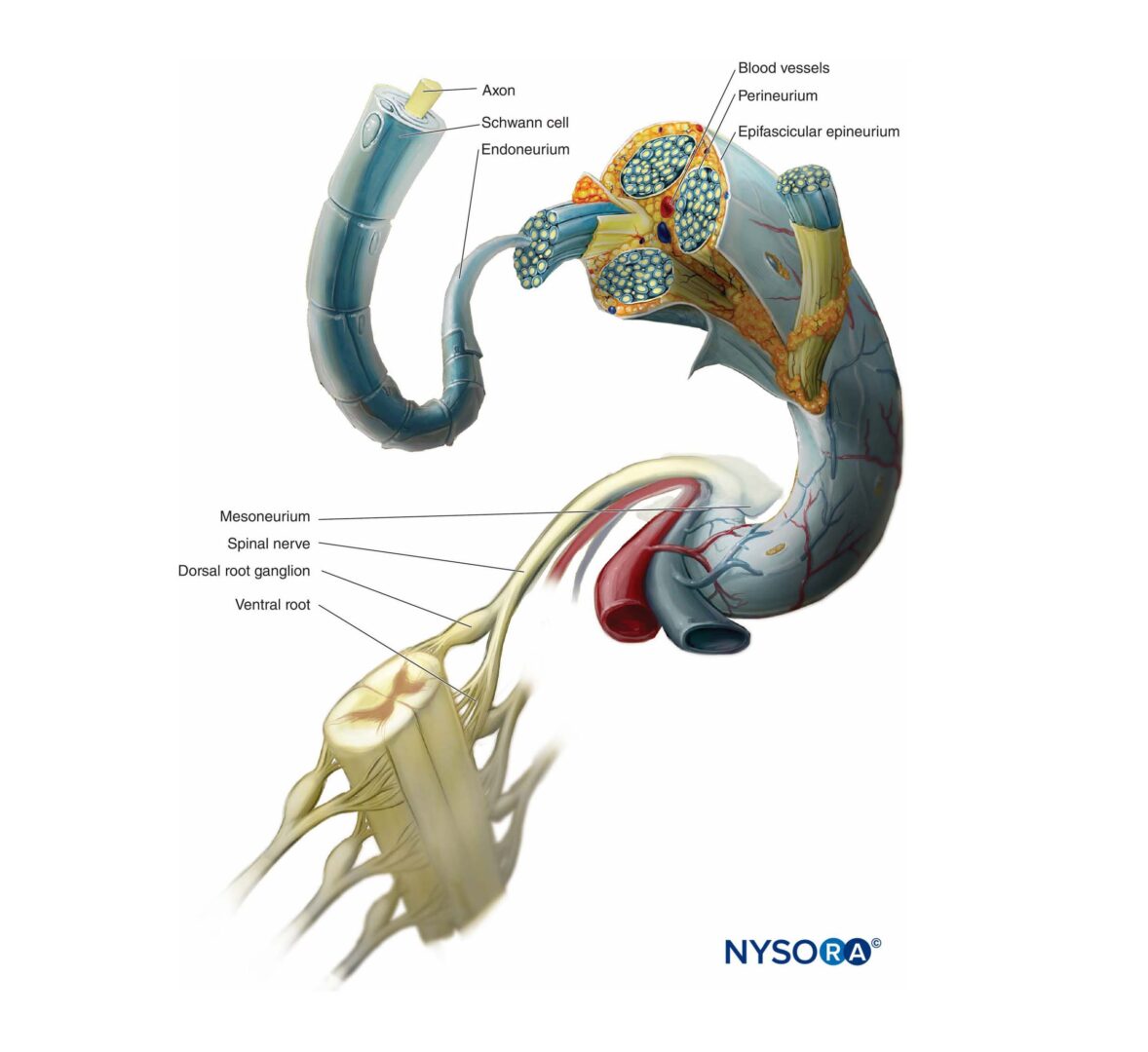
Levels of acetylcholine, dopamine, and other neurotransmitters also decline, and there may be an extraneuronal accumulation of amyloid, which underlies neurocognitive dysfunction. Alterations in brain phospholipid chemistry associated with changes in second messengers, such as diacylglycerol, are also evident in the elderly. Overall, both cerebral electrical and metabolic activity are decreased in elderly compared to younger individuals and may be a result of the multitude of anatomic, structural, and biochemical changes that accompany aging. It is possible that degenerative changes in the myelin sheaths of nerve fibers in the CNS and PNS can also lead to changes in nerve conduction velocity and disrupt the normal timing of neuronal circuits. Additional anatomical changes occur that affect nervous system function, including decreased spinal cord volume and degeneration of the bony spinal canal.
Changes in the somatic nervous system of the PNS associated with aging include (1) peripheral nerve deterioration; (2) dysfunction of genes responsible for myelin sheath protein components; (3) decreased myelinated nerve fiber conduction velocity; (4) motor and sensory discriminatory changes in the feet; and (5) changes in sensation (eg, pain, touch). The autonomic nervous system (ANS) of the PNS also experiences age-related changes that dictate most of the involuntary physiological functions of the body through the parasympathetic and sympathetic divisions. Aging of the ANS is characterized by (1) limited adaptability to stress; (2) decreased basal activity of the parasympathetic nervous system and overall net activation of the sympathetic nervous system; (3) decreased baroreflex sensitivity; and (4) slowing and weakening of homeostatic func-tions. The increase in sympathetic tone in older patients should also be considered when choosing an anesthetic with sympathomimetic properties, as such anesthetics may be poorly tolerated by some individuals with cardiovascular disease.
NYSORA Tips
- Aging is associated with a shift in balance within the autonomic nervous system toward a predominance of sympathetic tone.
Aging affects peripheral nerves, resulting in deterioration and decreases in the number of myelinated nerve fibers. Large myelinated fibers are particularly affected by aging, resulting in atrophy along with degenerative changes to the myelin. Levels of expression for key genes that encode major protein components of the myelin sheath, such as proteolipid protein and myelin basic protein, may influence this process. Maintenance of myelin sheath integrity involves continued expression of genes specifically associated with myelin protein production. Restoration of myelin sheaths to demyelinated axons occurs spontaneously in the adult nervous system, but aging has a detrimental effect on this process. Spontaneous remyelination efforts and the rate of reappearance of proteolipids and myelin basic proteins are slowed. In the CNS, oligodendrocyte progenitor recruitment and differentiation are also impaired by age-related decline in remyelination.
Changes in both the PNS and CNS may affect functional outcomes during the recovery phase following surgery and anesthesia and should be considered in the perioperative evaluation. The neurologic dysfunction of aging can produce altered pharmacodynamics, resulting in increased sensitivity to anesthetic medications with signs and symptoms of altered reflexes, deterioration of gait and mobility, altered sleep patterns, impairment of memory and intellect, and decrements of the senses. Perioperative delirium, a common form of acute cognitive impairment in elderly patients, can increase postoperative morbidity, present with difficult pain management scenarios, impair postoperative rehabilitation and prolong hospital stays. Delirium can occur in up to 80% of elderly postoperative patients depending upon the type and extent of surgery, perioperative anesthesia and analgesic needs of the patient, and type of pain therapy administered. It is more common with emergency, trauma, and major surgery. Risk factors associated with the development of delirium are numerous and include increased age, level of patient education, preexisting pain, and use of preoperative medications such as opioids, ketamine, and benzodiazepines. Subsequent to the negative effects of delirium, some patients may go on to experience postoperative cognitive dysfunction (POCD). A systematic review has confirmed that POCD is very com-mon and that older patients are at a higher risk of POCD after major noncardiac surgery than are younger patients.
NYSORA Tips
- Advancing age, level of patient education, and evidence of preexisting cerebral vascular disease are strong predictors of perioperative delirium.
Cardiovascular Function
There are a variety of morphological and functional changes in the cardiovascular system associated with aging, including a reduction in left ventricular compliance, generalized hypertro-phy of the left ventricular wall, fibrotic changes of the heart, and decreased myocardial compliance. These changes can result in increased stroke volume and elevated diastolic and systolic blood pressure (Table 2). Many elderly patients present with cardiac pathology, including moderate to severe coronary artery disease, valvular heart disease, and conduction defects that increase the risk of postsurgical morbidity and death. The effects of aging on cardiac output in the absence of coexisting disease may have minimal influence on the resting individual, but functional changes can become evident with stress and effort-dependent stress. Anesthetics and anesthesia technique may also interact with the patient’s preexisting cardiovascular disease in a manner that may be unfavorable. For example, patients with a fixed cardiac output (as in aortic stenosis) may not tolerate a decrease in systemic vascular resistance associated with neuraxial anesthesia well. Acute/extreme hemodynamic variability in the setting of regional anesthesia, however, can be overcome with careful titration of neuraxial anesthesia with an epidural or spinal catheter and skillful use of vasopressors.
Age-related influences on the cardiovascular system may have important clinical implications for the treatment of elderly surgical patients and for postoperative pain management, especially for those patients receiving regional anesthesia/analgesia. Several recent studies have demonstrated benefits of regional techniques on cardiac morbidity, intensive care unit (ICU) admissions and short-term survival. Although there are sparse data to indicate evidence-based and statistically significant differences in the impact of anesthetic technique on mortality or major complications, regional analgesia can positively influence pain management and lead to better outcomes when the type of surgery being performed is considered. Regional anesthesia/analgesia may have positive implications for perioperative cardiac function. For example, ischemic heart disease and hypertension are more common among elderly than younger patients, and coronary blood flow in such patients could be compromised in response to the sympathetic stimulation of surgery, perioperative stress, pain, and anesthesia. In a study by Park et al, researchers investigated the use of epidural anesthesia/analgesia combined with general anesthesia for abdominal aortic aneurysm repair. They showed that the duration of postoperative tracheal intubation, mechanical ventilation, and total ICU stay were reduced. In addition, the quality of postoperative analgesia improved, whereas the incidence of major complications and death were reduced.
Research has also shown that placement of thoracic epidural analgesia can improve left ventricular function and increase myocardial oxygen availability. In addition, patients with ischemic heart disease treated with a high thoracic epidural injection of bupivacaine showed improved myocardial blood flow in response to sympathetic stimulation. However, neuraxial anesthesia with an epidural in older patients undergoing coronary artery bypass grafting surgery has not been shown to improve perioperative outcomes. Therefore, to permit physicians to development preliminary guidelines and anesthesia protocols that could positively affect the cardiovascular outcomes of elderly surgical patients, studies investigating regional techniques should be tailored to match the planned surgery and adjusted for comorbid diseases and perioperative patient management needs (ie, procedure- and patientspecific anesthesia/analgesia). In addition to the mounting evidence of the regional anesthesia (with or without continuous local anesthetic infusion) on perioperative cardiac morbidity and mortality effectively managed postoperative pain could mitigate myocardial dysfunction if catecholamine levels associated with stress and pain are reduced. Regional anesthesia can also may provide superior analgesia compared to systemic opioids. Peripheral nerve blocks and neuraxial anesthesia the elderly can provide preemptive analgesia, reduce the side-effects or eliminate the need for general anesthesia (or completely avoid it in certain surgical settings), reduce sympathetic stimulation and stress responses associated with surgery, and directly inhibit transduction, transmission, and conduction of nociception from the surgical trauma site(s).
Regional techniques that complement multimodal analgesic therapies have been demonstrated to have beneficial effects on acute pain and may lead to a reduction in cardiac morbidity and mortality. Another factor to consider is the duration of postoperative analgesic needs because pain from surgery, surgical stress, and effects on the cardiovascular system often do not subside until several days following surgery. Therefore, the use of an effective regional technique (eg, continuous catheter) may provide sustained benefits by reducing postsurgical pain and its associated sympathetic and neuroendocrine stress responses. However, patients with coexisting cardiovascu-lar disease may be treated with anticoagulants or antiplatelet medications, or both, and careful attention should be paid to this issue prior to the administration of certain regional periph-eral or neuraxial techniques.
TABLE 2. Physiologic cardiovascular changes associated with aging and effects on pharmacokinetic variables.
| Physiologic Process | Magnitude | Variable Kinetic/Dynamic Consequences | General Dosing Strategy |
|---|---|---|---|
| Cardiac output | ↓ 0–20% | ↓ central compartment volume ↑ peak concentration of drug after bolus | Use smaller initial bolus dose Use slower injection rate *Potential for change in clearance and oral bioavailability *Potential for change in cerebral effects |
| Fat | ↑ 10–50%,then ↓ | Drug-specific changes are seen in distribution volume | Drug-specific (dose based on total body weight and/or lean body weight) |
| Muscle mass and blood flow | ↓ 20% | ||
| Plasma volume | Little change | ||
| Total body water | ↓ 10% | ↓ distribution volume (water-soluble drugs) | |
| Plasma albumin | ↓ 20% | ↑ free fraction of drug | Potential for change in clearance and oral bioavailability Potential for change in cerebral effects |
| Alpha-1 glycoprotein | ↑ 30–50% | Variable hepatic clearance of high-extraction drugs ↑ hepatic clearance of low-extraction drugs ↑ cerebral uptake of drugs | |
| Drug binding | Drug specific |
Pulmonary Function
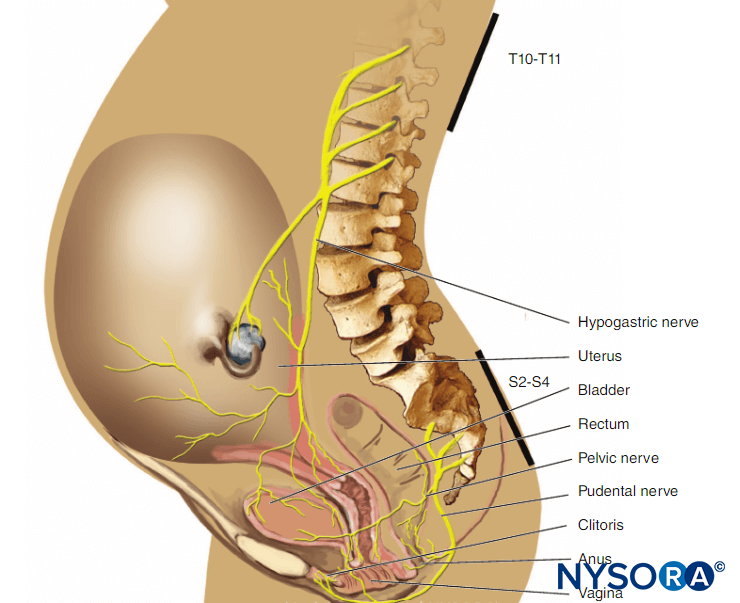
Respiratory compromise and complications among the elderly in the perioperative period can often be explained by functional and structural changes within the pulmonary system. Such alterations are commonly associated with aging as well as physiologic changes in response to hypoxemia and hypercarbia and increased sensitivity to the respiratory depressant effects of anesthetic agents and opioids. With aging, the elastic recoil of the lung parenchyma decreases in a fashion that functionally resembles emphysema, with less efficient alveolar gas exchange due to a loss of alveolar surface area and collapse of small airways. In addition, compliance of the chest wall decreases, which can lead to an increased work of breathing and increased risk for respiratory failure in the postoperative period for older patients. In all patients, there are reductions in functional residual capacity (FRC) created by assuming the supine position, being under the influence of general anesthesia, and experiencing surgery. These negative effects on FRC may persist for 7 to 10 days following surgery. FRC and closing volume gradually increase with age, and by age 45, closing volume exceeds FRC in the supine position. Vital capacity can be reduced by 25% to 50% from inadequate postoperative pain management (ie, splinting), along with the administration of systemic opioid analgesics that also contribute to alterations in tidal volume and respiratory rate and that can impair clearing of secretions (via altered cough mechanics). Elderly also have decreased responsivity to hypoxia and hypercapnia, as well as a greater incidence of COPD and obstructive sleep apnea (OSA). All of the above factors make opioid-sparing approaches to postoperative pain control desirable. However, while regional techniques may be beneficial in providing superior postoperative pain control with opioid-sparing effects, these modalities should be selected carefully given that patients with underlying pulmonary disease may poorly tolerate phrenic nerve dysfunction that can be associated with upper (interscalene and supraclavicular) brachial plexus block approaches. Therefore, patients should be assessed frequently for evidence of any adverse side effects, respiratory dysfunction, and adequate pain control throughout the perioperative period regardless of chosen analgesic methods.
Airway manipulation can be avoided, and respiratory parameters of lung function, respiration rate, tidal volume, respiratory drive (effort), and end-tidal carbon dioxide concentration can be preserved if surgical anesthesia can be achieved with regional modalities. Careful attention to the type of sedation used as an adjunct during these regional block placement procedures should be considered given the potential for increased sensitivity to opioids and benzodiazepines in the elderly, as well as the decreased responses to hypoxemia and hypercapnia and the increased incidence of OSA in this population. Unchanged FRC from baseline has been observed during spinal and lumbar epidural anesthesia. However, intercostal blocks and cervical, thoracic paravertebral, and high thoracic epidural block can be associated with lung volume reductions secondary to intercostal muscle relaxation. Therefore, choice of anesthesia may affect the degree of pulmonary dysfunction. Studies comparing regional versus general anesthesia/analgesia in elderly patients undergoing lower extremity orthopedic and major abdominal surgical procedures have shown that (1) older patients experience fewer hypoxic events with epidural and regional anesthesia (using local alone) com-pared to systemic opioids; (2) general anesthesia in older patients results in lower PaO2 levels (on postoperative day 1) compared to epidural and regional anesthesia; and (3) respira-tory complications are less frequent when comparing general anesthesia with postoperative intravenous morphine analgesia versus general anesthesia with postoperative epidural analge-sia. However, the elderly have increased sensitivity to the respiratory depressant effects of neuraxial opiates, and therefore these should be used with caution.
Pharmacokinetic and Pharmacodynamic Changes in the Elderly
Aging affects the pharmacokinetics and pharmacodynamics of medications (eg, sedative/hypnotics, opiates, nonopioid analgesics, local anesthetics), the physiologic functions of the body, and the composition/characteristics of organs and tissues within the body to variable degrees. The physiologic changes and effects on pharmacokinetics and pharmacodynamics in older patients, as well as some alterations that may be required for drug regimens in older patients, are listed in Tables 1, 2, and 3. Information in these tables addresses a number of issues related to local anesthetics and opioid analgesics in view of their widespread use and importance in perioperative pain management for older patients. The altered response to drugs associated with aging can be highly variable and somewhat unpredictable among individuals and are generally attributable to aging alone, but such responses may be compounded by a higher incidence of degenerative and other coexisting diseases in this patient population.
Multimodal Drug Therapy and the Elderly
A perioperative plan of care that includes a regional technique in an elderly patient must consider the inherent risk of sedation/hypnosis, multimodal drug regimens, and local anesthetic medications. Safety principles of treatment with analgesic and sedative medications for pain management in older patients, specific to regional and regional peripheral nerve block, are discussed and listed in Tables 1, 2, and 3. Sedative drugs (eg, midazolam, propofol) used during block placement should be easy to administer, short-acting, have a high safety margin, and limited adverse effects. Epinephrine can prolong peripheral nerve block duration, but caution must be exercised as epinephrine may cause an ischemic neurotoxicity in peripheral nerves with preexisting neuropathy (eg, in patients with diabetes).
There are several pharmacodynamic changes associated with aging. Understanding of how medications may affect older patients can be complex and unpredictable. Studies that have examined opioid pain management have been somewhat arbitrary, and surrogate measurements of effect other than clinical pain relief have not been adequately studied. An animal study by Piva et al, identified fewer mu-opioid receptors in the hypothalami of older rats, and, in contrast, greater concentrations of kappa-opioid receptors in the thalamus and amygdala of these animals. They also found that concentrations of delta-opioid receptors were not significantly different in young versus old rats. Scott et al. conducted a study of the pharmacokinetics and pharmacodynamics of fentanyl and alfentanil in older men by examining blood samples with a radioimmunoassay and found that the pharmacokinetics of these drugs were unaffected by age. However, the sensitivity of the brain to these opioids as measured by electroencephalogram (EEG) proved to be increased by 50% in these older subjects. Whether this finding can be attributed to a change in the number or function of opioid receptors in the CNS that is associated with aging or due to an increased penetration of opioids in the CNS remains unclear.There is no literature to support the need to alter ketamine doses in older patients. However, in aged animals, changes in composition of the N-methyl-D-aspartate (NMDA) receptor site and function have been reported. If one can extrapolate from these earlier animal studies, older patients may be more sensitive to the effects of ketamine, and doses may need to be decreased in this patient population.
TABLE 3. Physiologic hepatic and renal changes associated with aging and effects on pharmacokinetic variables.
| Physiological Process | Magnitude | Variable Kinetic/Dynamic Consequences | General Dosing Strategy |
|---|---|---|---|
| Liver | |||
| Liver size | ↓ 25–40% | ↓ hepatic clearance of high-extraction drugsEquivocal hepatic clearance of low-extraction drugs ↓ hepatic clearance of some low-extraction drugs | Minimal effect on drug IV bolus dose ↓ maintenance dosePotential for changes in oral bioavailability |
| Hepatic blood flow | ↓ 25–40% | ||
| Phase I (eg, oxidation) | ↓ 25% | ||
| Phase II | Little change | ||
| Kidney | |||
| Nephron mass | ↓ 30% | ↓ clearance of drugsLittle effect on opioids (parent compound) ↓ clearance of some active metabolites (eg, M6G) | ↓ maintenance dose(renally cleared drugs for renal clearance) Assume and monitor for accelerated accumulation of polar active (M6G) or toxic (M3G, norpethidine) metabolites |
| Renal blood flow | ↓ 10% per 10 years | ||
| Plasma flow at 80 years | ↓ 50% | ||
| Glomerular filtration rate | ↓ 30–50% | ||
| Creatinine clearance | ↓ 50–70% |
Clearance of tricyclic antidepressant (TCA) drugs and their active metabolites by hepatic cytochrome P450 and the kidney, respectively, decreases with increasing patient age, and lower initial doses are recommended in older patients. In addition, elderly patients may be particularly prone to the side effects of TCAs, including seda-tion, confusion, orthostatic hypotension, dry mouth, constipation, urinary retention, and gait disturbances (eg, increased risk of falls). As with TCAs, initial doses of anticonvulsant agents used for pain management (pregabalin, gabapentin, and topiramate) should be lower than for younger patients, and increases in dose should be titrated carefully. Adverse side effects such as somnolence and dizziness, especially with pregabalin, may be a problem in this group of patients. As renal function declines with increasing age, elimination of gabapentin and pregabalin may be reduced, and lower doses may be required.
Age-related changes in the body are responsible for alterations seen with systemic absorption, distribution, and clearance of local anesthetics that may result in an increased sensitivity, decreased dose requirement, and change in the onset and duration of action in elderly patients. For example, decreases in neural cell population, nerve conduction velocity, and inter-Schwann cell distance can produce an increased sensitivity to local anesthetics in the elderly. Advancing age also results in a decrease in the clearance of bupivacaine and ropivacaine. Older patients are more sensitive to the effects of local anesthetic agents secondary to a slowing of the conduction velocity (in the spinal cord and peripheral nerves) and a decrease in the number of neurons in the spinal cord.
NYSORA Tips
- The administration of nonsteroidal anti-inflammatory drugs (NSAIDs) and cyclooxygenase-2 (COX-2) inhibitors in elderly patients requires caution; acetaminophen may be the preferred nonopioid analgesic.
- The age-related decrease in opioid requirements in the elderly patient is related to the changes in pharmacodynamics that accompany aging.
Physiology and the Perception of Pain in the Elderly and Clinical Implications
Several review articles have summarized the many age-related changes that occur in pain perception and the neurophysiology of nociception in elderly surgical patients. There are extensive alterations in the structure, neurochemistry, and function of both the PNS and CNS of older patients. Included among these changes is the neurochemical deterioration of opioid and serotonergic systems. Therefore, there may be changes in nociceptive processing, including impairment of the pain inhibitory system, and pain intensity after surgery may be greater or less than otherwise expected from the severity of surgical trauma induced. In one study, older patients matched for surgical procedure reported less pain in the postoperative period, and pain intensity decreased by 10% to 20% for each decade after 60 years of age.
The structural and neurochemical changes that have been described in the PNS and CNS of the elderly continue to compromise optimal pain medicine protocols for these patients. Studies of the elderly nervous systems show a decrease in the density of myelinated and, particularly, unmyelinated peripheral nerve fibers. In addition, there is an increase in the number of nerve tissue fibers with evidence of degeneration and a slowing of nerve conduction velocity in older individuals. Gagliese et al reviewed animal and human experimental evidence on the neurobiology of aging and reported the following findings: (1) reductions in level of the neuropeptide substance P; (2) lowered concentrations of calcitonin gene-related peptide (a vasodilator neuropeptide expressed in a subgroup of small neurons in the dorsal root); and (3) reduced somatostatin levels within the circulatory system. Sensory neuron degenerative changes, loss of myelin in the dorsal horn of the spinal cord, and reductions in neurochemical mediators (substance P, somatostatin, and calcitonin gene-related peptide) have been noted. Once again, the clinical implications of these degenerative changes in many older individuals translate into pain being expressed as less severe along with evidence of increased pain thresholds in older patients.
A decrease in pain tolerance sometimes seen in elderly patients could also be secondary to decreases in noradrenergic and serotonergic neurons that contribute to the impairment of descending inhibitory mechanisms. Age-related loss of neu-rons and dendritic connections, along with changes in neurotransmitter synthesis, axonal transport, and receptor binding seen in the human brain are particularly evident in the cerebral cortex, including areas of the brain involved in nociceptive processing. The density of opioid receptors in the brain is decreased (although not evident in the spinal cord), and there may also be decreases in concentrations of circulating endogenous opioids. Therefore, compared to younger patients having the same type of surgery performed, older patients may report less pain or atypical pain, complain of pain at a later time during recovery, or report no pain from a surgical insult that generally produces at least mild-to-moderate pain scores in younger patients.
NYSORA Tips
- There is an age-related decrease in opioid requirements and significant interpatient variability in pain tolerance in elderly surgical patients.
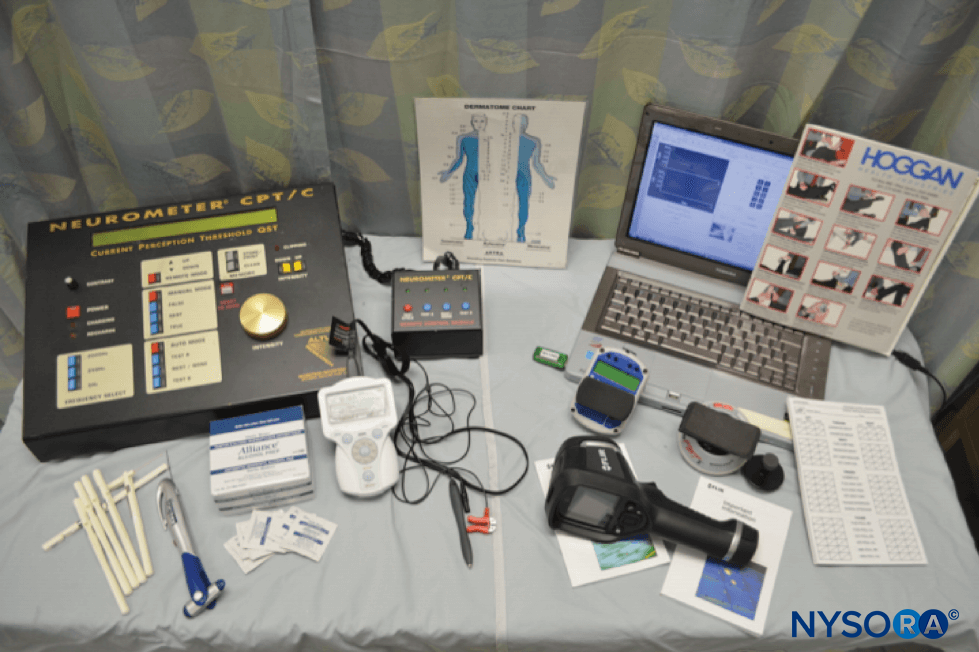
Functional MRI (fMRI) studies performed on older individuals show more similarities than differences in the magnitude of activation in the brain response to acute noxious stimulation. However, the functional consequences of age-related changes in the brain still remain a subject of debate. For example, studies investigating the effects of experimental pain stimuli (short periods of noxious stimuli not resulting in tissue injury) on pain thresholds are conflicting and appear to depend on the type of stimulus used. In addition, elderly individuals tend to have higher pain thresholds for thermal stimuli, but results from mechanical stimulation appear equivocal, and there is evidence that no change is seen in response to electrical stimuli across all age groups. However, in the clinical setting (where pain is often associated with tissue injury), these observations may explain the deficits seen in the early warning function of pain in older patients. For example, in elderly patients experiencing an acute myocardial infarction, a greater intensity of symptoms of chest discomfort and pain was inversely correlated with a lower pain threshold. There also appears to be a gap between identification of pain stimulus and recognition of the stimulus as being capable of causing tissue injury. Therefore, differences in the perception and reporting of pain by older surgical patients may result in pain therapy, medications, and regional analgesic interventions being delayed or deemed unnecessary.
A review of studies on age-related changes in pain tolerance (involving a variety of experimental pain stimuli) has shown a reduced ability of older individuals to endure or tolerate strong painful stimuli. This may have deleterious effects in the more vulnerable elderly patient and could mean that severe pain may have a greater negative impact if not effectively treated. In addition, elderly individuals show smaller increases in pain thresholds following prolonged noxious stimulation and evidence of prolonged recovery from hyperalgesia.
NYSORA Tips
- The assessment of pain and evaluation of pain management therapies in older patients present problems arising from differences in (1) reporting mechanisms; (2) cognitive dysfunction; (3) end-organ impairment/compromise (affecting medication metabolism and excretion); (4) variations in medication tolerance and abuse; and (5) inherent difficulties in the assessment of pain.
Assessment of Pain in Older Cognitively Impaired Patients
Inadequate treatment of acute pain is more likely to occur in older patients, especially those that are cognitively impaired. Even though cognitively impaired patients are just as likely as others of the same age and younger to experience painful conditions, the number of pain complaints, along with reported pain intensity, has been shown to be inversely related to the degree of cognitive impairment (due to diminished memory, impairment of capacity to report, or because less pain is experienced). However, studies in patients with dementia suggest that pain perception and processing are not diminished, and it would be false to assume that these patients experience less pain with surgery. Therefore, careful consideration must be given to the ways in which pain is assessed in older cognitively impaired individuals. While cognitively intact elderly patients can use a range of unidimensional pain scales (visual analog scale [VAS], verbal rating scale [VRS], numeric rating scale [NRS], or facial pain scale [FPS]), in patients with mild to moderate or severe cognitive impairment, a VRS or behavioral scale (eg, Doloplus-2 or Algoplus) may prove to be better pain assessment tools.
NYSORA Tips
- Elderly patients often describe pain as being less intense and often provide atypical descriptions of perioperative pain.
- The reported frequency and description of intensity of acute pain in clinical situations may often be reduced in older patients.
- Unidimensional measurements of pain can be used in older patients in the acute pain setting; in the clinical setting, VRS and NRS measurements provide the best validity in older adults.
- The undertreatment of acute pain is more likely to occur in cognitively impaired older patients than in those who are cognitively intact.
- Obtaining a history regarding past experiences with pain can be challenging in patients with cognitive impairment; the observations of caregivers may be helpful in these situations.
Considerations for the Use of Peripheral Regional and Neural block in Elderly Patients
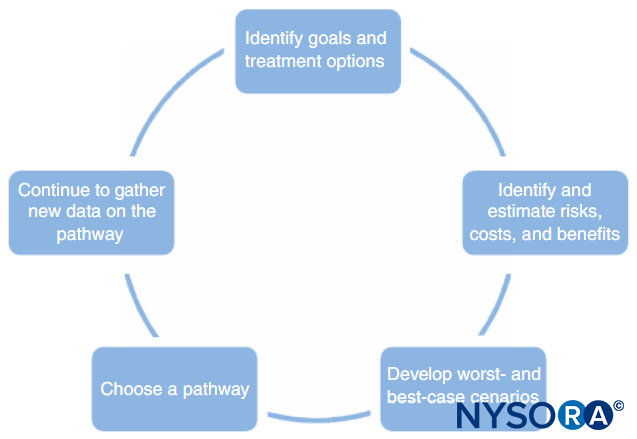
There are limited evidence-based guidelines regarding the use of specific regional analgesic modalities in older patients due to a host of secondary concerns, such as patient age, comorbidities, safety profile issues, and concurrent medications, which often exclude elderly individuals from clinical trials. However, many of these factors, along with several other concerns related to advanced age, need to be taken into consideration when choos-ing a procedure-specific analgesic regimen that may prove more advantageous than other more conventional pain management options, such as unimodal opioid analgesics. Decisions regarding regional options and peripheral nerve block choice should take into account the health status of the older patient, the operation being performed, and the expertise of the perioperative pain management healthcare providers. Therefore, to ensure safe use and conduct evidence-based research on regional and peripheral nerve block techniques in the elderly, needs should be assessed on a patient-to-type-of-surgery basis and geared toward regional pain medicine options that target the surgical site.
The number of elderly patients that present for anesthesia and surgery has increased exponentially in recent years, and neuraxial and peripheral nerve block techniques are frequently used in this patient population. Elderly patients can benefit from regional modalities of perioperative pain management. One important clinical observation that has emerged from the literature on regional anesthesia/analgesia is evidence that the use of regional techniques allows for the minimization or elimination of the negative side effect profiles of other systemic pain management options, such as bowel and bladder dysfunction, hemodynamic derangements, and cognitive effects often experienced with opiates and other analgesic adjuncts and sedative/hypnotics, to which older patients are often more sensitive.A multitude of factors can influence surgical outcomes in older patients, such as the type, duration, and invasiveness of an operation, coexisting medical or mental status dysfunction, and the skill and expertise of both the anesthesiologist and surgeon. These factors and others often make it difficult to decide if and when one regional analgesic technique is unequiv-ocally better than another. Therefore, until evidence-based research can provide conclusive guidelines on regional anesthesia/analgesia in the elderly, it is important to focus on optimiz-ing the overall perioperative pain management choices for elderly patients by implementing patient- and procedure-specific modes of regional anesthesia.
Anatomic changes associated with aging may make performing neuraxial and regional peripheral nerve anesthesia/analgesia more technically difficult in the geriatric population. Elderly individuals may have dorsal kyphosis, a tendency to flex their hips and knees because of osteoarthritic changes, decreased range of motion in the extremities, issues associated with advanced osteoporosis and rheumatoid arthritis, and calcification of cartilage. All of these issues may make positioning elderly patients for regional block placement more challenging. Neuraxial techniques may be complicated not only by difficultly with positioning patients, but also by degenerative disk and vertebral joint changes, along with the distortion and compression of intervertebral and epidural spaces associated with aging. The ligamentum flavum often becomes more calcified with age, such that attempts to accomplish an epidural block or dural puncture may be more challenging due to difficult needle placement and advancement through such dense, calcified ligaments. The presence of osteophytes may also decrease the size of the intervertebral space, which limits access to the subarachnoid space. A lateral (paramedian) needle approach to the epidural or subarachnoid space may avoid issues caused by vertebral midline ligament calcification and distortion of dorsal vertebrae. In addition, access to the epidural or subarachnoid space in patients with severe osteoarthritis and ossified ligaments may be more easily achieved by approaching the L5–S1 interspace, which is typically the largest intervertebral space.
NYSORA Tips
- A paramedian approach may facilitate needle placement to the epidural or subarachnoid space in patients with age-related changes to the vertebral anatomy.
Epidural Anesthesia and Analgesia
Epidural anesthesia/analgesia can provide an effective modality for pain management in a host of perioperative settings. The heterogeneity of studies regarding the use of epidural anesthesia/analgesia makes it difficult to draw conclusive evidence for optimal use in elderly patients. However, the consistent efficacy of epidural analgesia in the elderly has been well demonstrated, regardless of analgesic agent, location of catheter (if used), type of surgery, and type or time of pain assessment, and has been shown to provide superior pain relief compared to parenteral opioid administration.
A host of additional outcome studies have noted reductions in morbidity with regional techniques provided to elderly patients undergoing certain surgical procedures. For example, following hip fracture surgery, a continuous epidural infusion (local anesthetic and opioid) provided better pain relief, both at rest and with movement, but did not lead to improved rehabilitation. A meta-analysis reviewed studies that included a wide variety of epidural regimens and surgical procedures and examined the benefits of combining epidural analgesia with general anesthesia. The author reported a reduction in a range of adverse outcomes with epidural analgesia, including a reduced incidence of arrhythmias, earlier extubation times, a reduced need for and time spent in the ICU, reduced stress hormone levels, lower cortisol and glucose concentrations, and a reduced incidence of renal failure, when local anesthetics were used in thoracic epidurals. Another meta-analysis compared systemic opioids delivered via PCA versus epidural analgesia (both patient-controlled epidural analgesia [PCEA] and continuous infusion) and concluded that epidural analgesia provided superior pain relief at rest and with movement and was superior in terms of overall pain management. Further, a lower incidence of nausea and vomiting and sedation following all types of surgery was found with epidural analgesia. However, this meta-analysis also revealed that epidural analgesia was associated with a higher incidence of pruritus and motor block. Other studies have also supported the finding that older patients treated with neuraxial versus general anesthesia had lower pain scores at rest and with movement, higher satisfaction scores, improved mental status, more rapid recovery of bowel function, and a decreased risk of deep vein thrombosis and pulmonary embolism.
Epidural opioid requirements can be decreased as patient age increases. Some studies have revealed that older patients require a lower dose of opioid than younger patients to achieve the same degree of pain relief. However, a large degree of interpatient variability remains, and doses should be titrated cautiously and to effect in all elderly patients. The decreased need for epidural opioids in elderly patients appears greater than would be predicted by age-related alterations in physiology alone and may also have pharmacodynamic components. A comparison of fentanyl PCEA in patients over 65 years of age versus patients 20–64 years of age showed no difference in fentanyl PCEA requirements, pain scores at rest, or incidence of pruritus. However, dynamic pain (coughing) experienced from the abdominal surgery being performed was significantly better controlled in patients over age 65.
Decreased glomerular filtration rate (GFR) in older patients can result in a more rapid accumulation of active opioid metabolites (eg, M6G, M3G, hydromorphone-3-glucuronide, nor-dextropropoxyphene, norpethidine, desmethyl-tramadol) following continuous epidural administration. In addition, concerns for respiratory depression in elderly patients, particularly those with obesity, OSA, or other respiratory disease, can sometimes lead to inadequate neuraxial opioid doses being administered. However, respiratory depression is rare if appropriate concentration guidelines are followed and appropriate monitoring is implemented. In addition, the incidence of nausea and vomiting and pruritus in the postoperative period seems to lessen with increasing age. Some additional evidence shows that neuraxial fentanyl may cause less POCD than morphine, along with less potential for confusion. While the elderly may be more sensitive to the effects of opiates and require lower doses for analgesia, adequate postoperative pain control is also important to prevent delirium and maintain preoperative levels of cognitive function.
Age is a factor when determining spread of injected local anesthetic into the neuraxial space and the subsequent sensory level and degree of motor block achieved. Thus, the systemic absorption and disposition of long-acting local anes-thetics dictate that smaller volumes are needed to cover the same number of dermatomes than in younger patients. The same bolus volume of epidural local anesthetic administered to all patients revealed that the concentration required to achieve an effective motor block decreased as patient age increased. Therefore, older patients may be more susceptible to some of the adverse effects of epidural analgesia, including hypotension, if patient age and local anesthetic concentration/volume are not taken into consideration.In addition, combinations of local anesthetic and opioid are commonly used for epidural analgesia and may provide an additive/synergistic effect, so it is reasonable to use lower infusion rates in older patients.
NYSORA Tips
- The L5–S1 vertebral interspace is typically the largest intervertebral location to target for neuraxial techniques.
Intrathecal Opioid Analgesia
Subarachnoid administration of opioids (at varying doses) combined with local anesthetics during neuraxial techniques can provide effective anesthesia and perioperative analgesia, can create a synergistic effect with the local anesthetic, may prolong analgesic effects without associated motor block, and often provides for more effective targeted pain relief than with other routes (eg, intramuscular, PCA) of opioid administration. In addition, when used in combination with general anesthesia for major surgery, a spinal injection of opioid and local anesthetic can reduce the intraoperative requirement for inhalational anesthetic agents. However, caution must be exercised as the additional systemic administration (intravenous bolus or PCA) of opioid medications can create a risk of respiratory depression and pruritus. Therefore, secondary to advanced patient age, the potential for respiratory depression effects can be considered a serious enough risk factor to warrant consideration of postoperative admission and recovery in a monitored environment or ICU setting for patients over the age of 70 years. However, it has been reported that the subarachnoid administration of up to 200 mcg of intrathecal morphine with a local anesthetic for peripheral vascular surgery in older patients (average age 69 years) can be safely performed with minimal adverse respiratory sequelea. In addition, it has also been shown that respiratory depression can be minimized through the implementation of respiratory safety protocols, education of nursing and other healthcare providers on general wards, and postoperative management by an acute pain medicine service following strict respiratory parameter guidelines.
Intrathecal morphine provides excellent postoperative analgesia but may cause side effects such as postoperative nausea and vomiting, pruritus, and respiratory depression, particularly at larger doses; older patients may be at an increased risk of such side effects. The ideal or optimal dose of intrathecal opioid that should be mixed with local anesthetic during spinal anesthesia procedures for elderly patients is currently unknown. Despite a lack of evidence-based data, a subarachnoid morphine dose of 200 mcg has been suggested. Intrathecal morphine (200 mcg mixed with a local anesthetic) administration during spinal anesthesia in addition to general anesthesia in older patients (average age 70 years) undergoing abdominal aortic surgery resulted in improved postoperative analgesia along with a reduced need for postoperative analgesics when compared to elderly patients given general anesthesia alone. In a dose-response study by Murphy et al, three different doses of intrathecal morphine for elective hip arthroplasty surgery in elderly patients (patients aged > 65 years) were studied. Patients received either 50, 100, or 200 mcg of subarachnoid morphine, along with 15 mg of bupivacaine hydrochloride. The investigators concluded that 100 mcg of morphine added to the spinal anesthetic during hip surgery provided the most optimal balance between analgesia, pain relief, and pruritus. In addition, they observed that there was no difference in the incidence of nausea and vomiting or respiratory depression among the three groups of patients.
Evidence has shown that the strategic use of a low-dose opioid as an adjunct to local anesthetics during spinal anesthesia can reduce the concentration of inhalation agents required during general anesthesia. In addition, intrathecal morphine is a widely used method for postoperative pain relief after major abdominal and lower extremity orthopedic surgery. In many cases, it provides more effective perioperative analgesia with fewer side effects than intravenous opioid analgesics. In a randomized study of patients over age 70 who underwent colorectal surgery, Beaussier et al. compared preoperative intrathecal morphine (300 mcg) in addition to postoperative PCA with morphine (study group) with PCA morphine alone (control group). The investigation concluded that intrathecal morphine plus intravenous PCA, as compared with intravenous PCA morphine alone, improves immediate postoperative pain intensity and significantly reduces daily parenteral morphine consumption following surgery.
NYSORA Tips
- Intrathecal morphine at a dose below 200 mcg can be a useful adjunct for pain management following surgery with acceptable risk of respiratory depression.
Regional Anesthesia and Analgesia Using Peripheral Nerve and Nerve Plexus block
One approach to perioperative pain management in geriatric patients is to consider the postoperative complications commonly associated with routine surgical procedures and then evaluate how one might mitigate these complications using peripheral nerve and nerve plexus block. Elderly patients are more likely to have underlying neurologic, pulmonary, and cardiovascular disease, all of which can lead to serious complications in any surgical setting. While there are established clinical practices and theoretical indications regarding the use of safe and effective regional techniques for elderly patients, a lack of consistency among studies has prevented the development of firm recommendations to guide which regional anesthetics and analgesia techniques offer the greatest advantages for elderly patients undergoing particular surgical procedures.
Peripheral nerve block can be a supplemental analgesic technique for medical interventions and satisfactory analgesia for a host of surgical procedures on the upper and lower extremities, abdomen, groin, and chest wall. Definitions and descriptions of regional peripheral nerve block techniques are variable, as are the definitions of the various techniques of analgesia and anesthesia (Table 4). Clinical investigations often use neuraxial anesthesia (with or without analgesia) in the definition of regional anesthesia. However, other studies include only peripheral nerve and nerve plexus block, local anesthetic infiltration, and local anesthetic injection in the definition of regional anesthesia. When strategically applied (ie, procedure- and patient-specific) and with effective results, regional peripheral nerve and nerve plexus block techniques may offer distinct advantages in the care of older surgical and medical patients. In particular, regional peripheral nerve and nerve plexus block techniques may allow for a reduction in the incidence of adverse side effects compared to other conven-tional pain management therapies (intramuscular, oral, and parenteral analgesics and central neuraxial block).
Some clinicians feel that epidural analgesia remains the standard of care for pain relief for a host of surgical procedures in the elderly, but peripheral nerve and nerve plexus block have proven to be as effective and are gaining popularity since the incidence of potential side effects associated with neuraxial techniques may be less. Systematic reviews and meta-analyses of randomized trials comparing epidural analgesia with peripheral nerve block for major knee surgery have shown similar relative analgesic efficacy between both pain management strategies (neuraxial versus peripheral nerve block). And, although pain profiles from peripheral nerve block techniques compared favorably with lumbar epidural analgesia for major knee surgery with no significant difference in pain scores at rest, complications such as hemodynamic variability, nausea and vomiting, urinary retention and bowel dysfunction, increased dynamic (ie, movement, rehabilitation) pain scores and an increased need for supplemental opioid analgesics for break-through pain occurred more frequently in the epidural group. Rehabilitation indices were similar between groups, but patient satisfaction was higher in the groups that received peripheral nerve blocks, and these modalities are not likely to cause neur-axial complications.
TABLE 4. Analgesia and anesthesia techniques.
| Local Monitored Anesthesia Care (LMAC) (LMAC) | LMAC with or without Intravenous and Oral Sedatives, Hypnotics, Analgesics (Opioid and Nonopioid) |
|---|---|
| General Anesthesia and analgesia Anesthesia Analgesia | With or without perioperative medicationsInhalation agents, intravenous agents, and/or total intravenous anesthesia (TIVA) Systemically administered analgesia with opioids, nonopioids, and other adjuncts • Intramuscular injections • Intravenous boluses • Patient-controlled analgesia (PCA) • Transdermal, mucous membrane, and oral routes |
| Regional Anesthesia and Analgesia Neuraxial Peripheral nerve/nerve plexus block Infiltration/field block | With or without other intravenous perioperative medications (analgesics, sedation)Spinal (subarachnoid) and/or epidural anesthesia and/or analgesia • Single injection, with or without catheters • Local anesthetic (type, concentration) with or without opioids and other adjuncts • Vertebral level of block placement/initiation • Level of block achieved • Length or duration of postoperative anesthesia and analgesia Peripheral nerve block • Local anesthetic with or without additives • Single injection or continuous catheter technique Brachial plexus block • Femoral block • Sciatic/popliteal block • Paravertebral block • Transverse abdominis plane block, etc. Local anesthetic infiltration/injection (diffusion block) • With or without indwelling catheters |
In an investigation by Zaric et al, epidural analgesia was compared to combined femoral and sciatic peripheral nerve block following total knee replacement surgery. Primary outcome measures included the incidence of side effects, including urinary retention, moderate to severe degrees of dizziness, pruritus, sedation, and nausea and vomiting during the postoperative period. Intensity of motor block, pain at rest and on mobilization, and rehabilitation indices were also registered for three days after surgery. Side effects in the epidural group were present in 87% of patients (one or more side effects), whereas only 35% of patients in the femoral and sciatic block group were affected. In addition, motor block was more intense (operated and nonoperated limb) on the day of surgery and the first postoperative day in the epidural group. Pain on mobilization was well controlled in both groups, rehabilitation indices were similar, and there were no differences in the length of hospital stay between groups. The results demonstrate a reduced incidence of side effects in the femoral and sciatic nerve block group compared to the epidural group.Similarly, epidural analgesia is considered to be a superior method of pain relief after major thoracic surgery. However, placement of a paravertebral block (PVB) using a PVB catheter can offer comparable analgesic effectiveness and a better side effect profile than neuraxial options with an epidural catheter. In addition to there being no significant difference between each group in terms of pain relief, these systematic reviews and meta-analyses of relevant randomized trials comparing PVB with epidural analgesia for thoracic surgery revealed that hemodynamic variability, urinary retention, increased plasma cortisol concentrations (as a marker of post-operative stress), nausea, pruritus, respiratory depression (atelectasis, pneumonia), prolonged operative time, reports of incomplete (or failed) epidural, and paraplegia (in rare cases) were reported far more frequently in the epidural groups when compared to those in the paravertebral groups. The most common and often serious compromising side effect profiles of respiratory complications, nausea and vomiting, and hypotension were less common with PVBs, as were a lower rate of failed blocks and a reduced incidence of urinary retention.
Elderly patients may also benefit when they receive procedure-specific regional techniques for postoperative pain management as doses of intravenous opioid drugs may be reduced. In addition, optimal target-specific perioperative anal-gesic management and the potential to reduce negative cognitive effects is possible by incorporating regional anesthesia procedure-specific pain therapy. POCD can be a common complication after cardiac and major noncardiac surgery with general anesthesia in the elderly, and it has been hypothesized that POCD may occur less often with regional anesthesia. The incidence of cognitive dysfunction after general or regional anesthesia in elderly patients raises the questions of whether a causative relationship exists between certain types of anesthesia and long-term POCD and whether regional anesthesia may decrease mortality and the incidence of POCD early after surgery. In another study of older hip fracture patients, those who received a femoral nerve block for perioperative analgesia, in addition to regularly scheduled nonopioid analgesics, were less likely to develop postoperative delirium, were able to sit up at the bedside sooner, and required no supplemental opioid analgesics compared to patients administered only nonopioid analgesics (28% of whom required supplemental morphine analgesia).
Proper patient selection and surgery-specific peripheral nerve and nerve plexus block when effectively administered (timed correctly and matched with appropriate type of surgical intervention) can provide excellent perioperative pain management in all patient populations. However, there is some evidence to suggest that the effects of peripheral nerve block can be prolonged in some elderly patients, thereby reducing or eliminating the need for opioid medications for breakthrough pain following hospital discharge. In addition, when considering prolonged duration of peripheral nerve block effects, elderly patients should be counseled appropriately regarding such effects prior to block placement, and care should be taken to ensure that older patients have appropriate assistance in their home if peripheral nerve blocks are to be placed for outpatient surgery. With these safeguards in place, efficacious adminis-tration of regional analgesic modalities can result in a reduction or elimination of opioid analgesics for breakthrough pain in the postoperative period. For example, two studies showed a pro-longed duration of effective analgesia in older patients following (1) a sciatic nerve block for lower extremity surgery; and (2) brachial plexus block for upper extremity surgery.
As mentioned previously, there are factors affecting the spread of both local anesthetics and adjuncts when placed into the epidural space. Therefore, could a paravertebral approach provide effective anesthesia or analgesia without unwanted spread of local anesthetics when placed in the neuraxial space of older patients? In a study by Akin et al, patients older than 65 years of age who underwent urological surgery following administration of a paravertebral lumbar plexus block (using ropivacaine or bupivacaine) showed improved pain scores, reduced incidence of cognitive dysfunction, and a stable heart rate and blood pressure. Cheema et al. investigated patients undergoing paravertebral nerve block procedures for the treatment of chronic pain conditions. Findings from this study revealed that, unlike the variable spread of local anesthetics administered for epidural analgesia, the age of the patient did not influence the spread of bupivacaine when placed in the thoracic paravertebral space.
An additional important factor to consider in all patients is the contraindication to regional anesthesia in anesthetized patients. Unlike neuraxial anesthesia, it may be safe to perform paravertebral blocks in heavily sedated or anesthetized patients without any apparent increased risk of neurological injury. Therefore, in elderly patients who experience pain or discomfort during positioning for neuraxial or paravertebral block techniques, paravertebral blocks may be placed under heavy sedation or general anesthesia without concern for significant compromise of neurologic injury. Studies have also addressed whether a paravertebral block is as effective as epidural analgesia for pain management in elderly patients undergoing thoracic surgery. In a review of the literature (184 papers found with seven representing the best evidence), all studies agreed that a paravertebral block was at least as effective as epidural analgesia for post-thoracotomy pain control but with a more favorable side effect profile and lower complication rates. Pain assessed via VAS at rest and with coughing was signifi-cantly lower in the paravertebral groups compared to the epidural groups (P = 0.02 and P = 0.0001, respectively). Pul-monary function assessed by peak expiratory flow rate (PEFR) was better preserved in the paravertebral groups; the lowest PEFR as a fraction of preoperative control was 0.73 in the paravertebral groups in contrast with 0.54 in the epidural groups (P < 0.004), and oxygen saturation was better in the paravertebral groups of patients compared to the epidural groups (P = 0.0001). Plasma concentrations of cortisol (marker of postoperative stress) increased markedly in both groups, but the increments were statistically different and more favorable in the paravertebral groups of patients (P = 0.003). Patients in the epidural block groups were associated with more frequent side effects such as (1) urinary retention (42%); (2) nausea (22%); (3) itching (22%); and (4) hypotension (3%). The epidural block groups experienced prolonged operative times and were associated with more technical failures and epidural displacement (8%) compared to the paravertebral groups. In addition, the epidural groups also experienced a higher complication of atelectasis and pneumonia compared to the paravertebral block groups, and the paravertebral block groups were found to experience a quicker return to normal pulmonary function.
The incidence of cancer and cancer surgery is significantly greater in the elderly patient population. Some evidence from animal and retrospective human studies has emerged indicating that regional analgesia may attenuate the immunosuppressive effects of surgery, anesthesia, and perioperative pain and may therefore improve patient outcomes. Metastatic disease remains an important cause of cancer-related death, and the likelihood of tumor metastases depends on the balance between antimetastatic host defenses (eg, cell-mediated immunity, natural killer cell function) and the metastatic potential of any given tumor. Snyder et al suspected anesthetic technique along with other perioperative factors could have the potential to affect the long-term outcome after cancer surgery since surgery can inhibit important host defenses, thus increasing the likelihood of the development of metastases. The investigators questioned whether anesthetic technique and medication choices (eg, intravenous anesthetics, volatile agents) could interact with the cellular immune system and affect long-term outcome. The investigators had a particular interest in whether there was any beneficial effect from regional anesthesia and whether regional anesthesia may play a role in pain and stress reduction, along with other potentially important perioperative risk factors that might impact cancer recurrence. In addition, opioid analgesia is suspected to induce some degree of suppression of cell-mediated immunity (notably natural killer cell activity). Therefore, using opioid-sparing anesthetic and analgesic tech-niques during the perioperative period could potentially have a positive effect on long-term survival and cancer disease recur-rence.147 Data regarding anesthetic technique and cancer sur-vival or recurrence has been mixed, and further prospective studies are still needed to further elucidate these relationships.
SUMMARY
People over 65 years of age represent a fast-growing segment of society, and these older individuals have surgery more frequently than younger age-group populations. Effective postoperative analgesia remains essential in older patients because inadequate pain control after surgery is often associated with a host of well-documented adverse outcomes. Management of postoperative pain in older patients can be complicated by a number of vari-ables, including a higher risk of age- and disease-related changes in physiology and anatomy, disease–drug and drug–drug interactions, altered cognitive baseline, potential negative effects from acute trauma (surgical or accidental), and lack of evidence-based, procedure-specific regional anesthesia and analgesia tech-niques for elderly individuals. Therefore, the concept of “diligence, start low, and go slow” should be adopted for any chosen analgesic strategy in the elderly surgical population.
With knowledge, skill, and comprehension of limitations, postoperative analgesic treatment using most medications (acetaminophen, NSAIDs, opioids, local anesthetics), analgesic techniques (intravenous or epidural PCA, intrathecal opioid, peripheral nerve and nerve plexus block), and pain management strategies (pre-emptive or multimodal analgesia) can be used effectively for acute perioperative pain management in older patients. The physiologic changes of aging need to be carefully considered because mammalian aging is often individualized and progressive. Proper assessment of pain management in the elderly must take into account chronological age, biological age, individual profiles of pathology, and prescribed medications, along with regard to organ system function and compromise. Methods of assessing pain in older individuals must also be carefully considered, particularly in those with cognitive impairment. Treatment options must be carefully adjusted and tailored to each patient in view of the pharmacokinetic and pharmacodynamic changes that occur in older individuals. In addition, since there is often a higher incidence of comorbidities and a greater use of concurrent medications in elderly versus younger populations, careful selection from among the multitude of analgesic options must be considered. Therefore, consistent and frequent evaluation of treatment efficacy of any selected regional technique along with monitor-ing and adjusting for incidence and severity of any adverse events should be thoughtfully and vigilantly controlled in the elderly.
REFERENCES
- White PF, White LM, Monk T, et al: Perioperative care for the older outpatient undergoing ambulatory surgery. Anesth Analg 2012;114:1190–1215.
- Konttinen N, Rosenberg PH: Outcome after anaesthesia and emergency surgery in patients over 100 years old. Acta Anaesthesiol Scand 2006; 50:283–289.
- Kojima Y, Narita M: Postoperative outcome among elderly patients after general anesthesia. Acta Anaesthesiol Scand 2006;50:19–25.
- Soltow QA, Jones DP, Promislow DE: A network perspective on metabolism and aging. Integr Comparative Biol 2010;50:844–854.
- Schwab CW, Kauder DR: Trauma in the geriatric patient. Arch Surg 1992;127:701–706.
- Troncale JA: The aging process. Physiologic changes and pharmacologic implications. Postgrad Med 1996;99:111–114, 120–112.
- Turnheim K: When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol 2003;38:843–853.
- Morrison JH, Hof PR: Life and death of neurons in the aging brain. Science 1997;278:412–419.
- Collins KJ, Exton-Smith AN, James MH, Oliver DJ: Functional changes in autonomic nervous responses with ageing. Age and ageing. 1980;9: 17–24.
- Meier-Ruge W, Ulrich J, Bruhlmann M, Meier E: Age-related white matter atrophy in the human brain. Ann N Y Acad Sci 1992;673:260–269.
- Salat DH: The declining infrastructure of the aging brain. Brain Connect 2011;1:279–293.
- Madden DJ, Bennett IJ, Song AW: Cerebral white matter integrity and cognitive aging: contributions from diffusion tensor imaging. Neuropsychol Rev 2009;19:415–435.
- Bekker AY, Weeks EJ: Cognitive function after anaesthesia in the elderly. Best Pract Res Clin Anaesthesiol 2003;17:259–272.
- Bitsch MS, Foss NB, Kristensen BB, Kehlet H: Acute cognitive dysfunction after hip fracture: frequency and risk factors in an optimized, multimodal, rehabilitation program. Acta Anaesthesiol Scand 2006;50: 428–436.
- Fong HK, Sands LP, Leung JM: The role of postoperative analgesia in delirium and cognitive decline in elderly patients: a systematic review. Anesth Analg 2006;102:1255–1266.
- Greene NH, Attix DK, Weldon BC, Smith PJ, McDonagh DL, Monk TG: Measures of executive function and depression identify patients at risk for postoperative delirium. Anesthesiology 2009;110:788–795.
- Hovens IB, Schoemaker RG, van der Zee EA, Heineman E, Izaks GJ, van Leeuwen BL: Thinking through postoperative cognitive dysfunction: How to bridge the gap between clinical and pre-clinical perspectives. Brain Behav Immun 2012;26:1169–1179.
- Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM: Postoperative delirium: the importance of pain and pain management. Anesth Analg 2006;102:1267–1273.
- Casati A, Fanelli G, Pietropaoli P, et al: Monitoring cerebral oxygen saturation in elderly patients undergoing general abdominal surgery: a prospective cohort study. Eur J Anaesthesiol 2007;24:59–65.
- Morimoto Y, Yoshimura M, Utada K, Setoyama K, Matsumoto M, Sakabe T: Prediction of postoperative delirium after abdominal surgery in the elderly. J Anesth 2009;23:51–56.
- Newman S, Stygall J, Hirani S, Shaefi S, Maze M: Postoperative cognitive dysfunction after noncardiac surgery: a systematic review. Anesthesiology 2007;106:572–590.
- North BJ, Sinclair DA: The intersection between aging and cardiovascular disease. Circ Res 2012;110:1097–1108.
- Taddei S, Virdis A, Ghiadoni L, Versari D, Salvetti A: Endothelium, aging, and hypertension. Curr Hypertens Rep 2006;8:84–89.
- Atanassoff PG: Effects of regional anesthesia on perioperative outcome. J Clin Anesth 1996;8:446–455.
- Roy RC: Choosing general versus regional anesthesia for the elderly. Anesthesiol Clin North America 2000;18:91–104, vii.
- Park WY, Thompson JS, Lee KK: Effect of epidural anesthesia and analgesia on perioperative outcome: a randomized, controlled Veterans Affairs cooperative study. Ann Surg 2001;234:560–569; discussion 569–571.
- Schmidt C, Hinder F, Van Aken H, et al: The effect of high thoracic epidural anesthesia on systolic and diastolic left ventricular function in patients with coronary artery disease. Anesth Analg 2005;100: 1561–1569.
- Jakobsen CJ, Nygaard E, Norrild K, et al: High thoracic epidural analgesia improves left ventricular function in patients with ischemic heart. Acta Anaesthesiol Scand 2009;53:559–564.
- Lagunilla J, Garcia-Bengochea JB, Fernandez AL, et al: High thoracic epidural block increases myocardial oxygen availability in coronary surgery patients. Acta Anaesthesiol Scand 2006;50:780–786.
- Nygard E, Kofoed KF, Freiberg J, et al: Effects of high thoracic epidural analgesia on myocardial blood flow in patients with ischemic heart disease. Circulation 2005;111:2165–2170.
- Barrington MJ, Kluger R, Watson R, Scott DA, Harris KJ: Epidural anesthesia for coronary artery bypass surgery compared with general anesthesia alone does not reduce biochemical markers of myocardial damage. Anesth Analg 2005;100:921–928.
- Perlas A, Chan VW, Beattie S. Anesthesia Technique and Mortality after Total Hip or Knee Arthroplasty: A Retrospective, Propensity Score-matched Cohort Study. Anesthesiology. 2016 Oct;125(4):724–31.
- Richman JM, Liu SS, Courpas G, et al: Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg 2006;102:248–257.
- Sprung J, Gajic O, Warner DO: Review article: age-related alterations in respiratory function – anesthetic considerations. Can J Anaesth 2006; 53:1244–1257.
- Don HF, Wahba M, Cuadrado L, Kelkar K: The effects of anesthesia and 100 per cent oxygen on the functional residual capacity of the lungs. Anesthesiology 1970;32:521–529.
- Corcoran TB, Hillyard S: Cardiopulmonary aspects of anaesthesia for the elderly. Best Pract Res Clin Anaesthesiol 2011;25:329–354.
- Urmey WF, Talts KH, Sharrock NE: One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991;72: 498–503.
- Werawatganon T, Charuluxanun S: Patient-controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev 2005:CD004088.
- Hudcova J, McNicol E, Quah C, Lau J, Carr DB: Patient-controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev 2006:CD003348.
- Rigg JR, Jamrozik K, Myles PS, et al: Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet 2002;359: 1276–1282.
- Meylan N, Elia N, Lysakowski C, Tramer MR: Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth 2009; 102:156–167.
- Snoeck MM, Vree TB, Gielen MJ, Lagerwert AJ: Steady state bupivacaine plasma concentrations and safety of a femoral “13-in-1” nerve block with bupivacaine in patients over 80 years of age. Int J Clin Pharmacol Ther 2003;41:107–113.
- Hebl JR, Kopp SL, Schroeder DR, Horlocker TT: Neurologic complications after neuraxial anesthesia or analgesia in patients with preexisting peripheral sensorimotor neuropathy or diabetic polyneuropathy. Anesth Analg 2006;103:1294–1299.
- Hogikyan RV, Wald JJ, Feldman EL, Greene DA, Halter JB, Supiano MA: Acute effects of adrenergic-mediated ischemia on nerve conduction in subjects with type 2 diabetes. Metabolism 1999;48:495–500.
- Vuyk J: Pharmacodynamics in the elderly. Best Pract Res Clin Anaesthesiol 2003;17:207–218.
- Piva F, Celotti F, Dondi D, et al: Ageing of the neuroendocrine system in the brain of male rats: receptor mechanisms and steroid metabolism. J Reprod Fertil Suppl 1993;46:47–59.
- Scott JC, Stanski DR: Decreased fentanyl and alfentanil dose requirements with age. A simultaneous pharmacokinetic and pharmacodynamic evaluation. J Pharmacol Exp Ther 1987;240:159–166.
- Clayton DA, Grosshans DR, Browning MD: Aging and surface expression of hippocampal NMDA receptors. J Biol Chem 2002; 277:14367–14369.
- Fu L, Mao YH, Gao Y, Liu L, Wang ZP, Li LC: [Expression of NR1 mRNA of NMDA receptor by gastrodine on hypoxia injury in cultured rat cerebral cortical neurons]. Zhongguo Zhong Yao Za Zhi [China Journal of Chinese Materia Medica] 2008;33:1049–1052.
- Ahmad M, Goucke CR: Management strategies for the treatment of neuropathic pain in the elderly. Drugs & Aging 2002;19:929–945.
- Fine PG: Pharmacological management of persistent pain in older patients. Clin J Pain 2004;20:220–226.
- Argoff CE: Pharmacotherapeutic options in pain management. Geriatrics 2005;Suppl:3–9.
- Guay DR: Pregabalin in neuropathic pain: a more “pharmaceutically elegant” gabapentin? American J Geriatr Pharmacother 2005;3:274–287.
- McGeeney BE: Pharmacological management of neuropathic pain in older adults: an update on peripherally and centrally acting agents. J Pain Symptom Manage 2009;38:S15–27.
- Veering BT, Burm AG, van Kleef JW, Hennis PJ, Spierdijk J: Epidural anesthesia with bupivacaine: effects of age on neural block and pharmacokinetics. Anesth Analg 1987;66:589–593.
- Veering BT, Burm AG, Vletter AA, van den Hoeven RA, Spierdijk J: The effect of age on systemic absorption and systemic disposition of bupivacaine after subarachnoid administration. Anesthesiology 1991; 74:250–257.
- Olofsen E, Burm AG, Simon MJ, Veering BT, van Kleef JW, Dahan A: Population pharmacokinetic-pharmacodynamic modeling of epidural anesthesia. Anesthesiology 2008;109:664–674.
- Simon MJ, Veering BT, Vletter AA, Stienstra R, van Kleef JW, Burm AG: The effect of age on the systemic absorption and systemic disposition of ropivacaine after epidural administration. Anesth Analg 2006;102: 276–282.
- Sadean MR, Glass PS: Pharmacokinetics in the elderly. Best Pract Res Clin Anaesthesiol 2003;17:191–205.
- Gibson SJ, Farrell M: A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin J Pain 2004; 20:227–239.
- Gagliese L, Weizblit N, Ellis W, Chan VW: The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain 2005;117:412–420.
- Gibson SJ, ed: Pain and Aging: The Pain Experience Over the Adult Life Span. Seattle: IASP, 2003; Dostrovsky JO, Carr DB, Koltzenburg M, eds. Proceedings of the 10th World Congress on Pain. Progress in Pain Research and Management 24.
- Thomas T, Robinson C, Champion D, McKell M, Pell M: Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain 1998;75:177–185.
- Sato A, Sato Y, Suzuki H: Aging effects on conduction velocities of myelinated and unmyelinated fibers of peripheral nerves. Neurosci Lett 1985;53:15–20.
- Rivner MH, Swift TR, Malik K: Influence of age and height on nerve conduction. Muscle Nerve 2001;24:1134–1141.
- Gagliese L, Ferrell M: The neurobiology of ageing, nociception and pain: an integration of animal and human experimental evidence. In: Gibson SJ, Weiner DK (eds): Progress in Pain Research and Management: Pain in the Older Person. Seattle: IASP, 2005, pp 25–44.
- Gagliese L, Gauthier LR, Macpherson AK, Jovellanos M, Chan VW: Correlates of postoperative pain and intravenous patient-controlled analgesia use in younger and older surgical patients. Pain Med 2008;9:299–314.
- Long X, Liao W, Jiang C, Liang D, Qiu B, Zhang L: Healthy aging: an automatic analysis of global and regional morphological alterations of human brain. Acad Radiol 2012;19:785–793.
- Fjell AM, Walhovd KB: Structural brain changes in aging: courses, causes and cognitive consequences. Rev Neurosci 2010;21:187–221.
- Gibson SJ: Older people’s pain. In Pain: Clinical Updates. Volume 14. Seattle: IASP, 2006, pp 147–164.
- Ralston HJ, 3rd: Pain and the primate thalamus. Prog Brain Res 2005; 149:1–10.
- Knyihar E, Csillik B: Plasticity of nociception: recent advances in function-oriented structural pain research. Ideggyogy Sz 2006;59:87–97.
- Onur OA, Piefke M, Lie CH, Thiel CM, Fink GR: Modulatory effects of levodopa on cognitive control in young but not in older subjects: a pharmacological fMRI study. J Cog Neurosci 2011;23:2797–2810.
- Pickering G: Age differences in clinical pain states. In: Gibson SJ, Weiner DK (eds): Progress in Pain Research and Management: Pain in the Older Person. Seattle: IASP Press, 2005.
- Cole LJ, Farrell MJ, Gibson SJ, Egan GF: Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging 2010;31:494–503.
- Peyron R, Laurent B, Garcia-Larrea L: Functional imaging of brain responses to pain. A review and meta-analysis (2000). Neurophysiol Clin 2000;30:263–288.
- Seifert F, Maihofner C: Representation of cold allodynia in the human brain—a functional MRI study. Neuroimage 2007;35:1168–1180.
- Granot M, Khoury R, Berger G, et al: Clinical and experimental pain perception is attenuated in patients with painless myocardial infarction. Pain 2007;133:120–127.
- Zheng Z, Gibson SJ, Khalil Z, Helme RD, McMeeken JM: Age-related differences in the time course of capsaicin-induced hyperalgesia. Pain 2000;85:51–58.
- Feldt KS, Ryden MB, Miles S: Treatment of pain in cognitively impaired compared with cognitively intact older patients with hip-fracture. J Am Geriatr Soc 1998;46:1079–1085.
- Forster MC, Pardiwala A, Calthorpe D: Analgesia requirements following hip fracture in the cognitively impaired. Injury 2000;31:435–436.
- Morrison RS, Siu AL: A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage 2000;19:240–248.
- Ardery G, Herr K, Hannon BJ, Titler MG: Lack of opioid administration in older hip fracture patients (CE). Geriatr Nurs 2003;24:353–360.
- Farrell MJ, Katz B, Helme RD: The impact of dementia on the pain experience. Pain 1996;67:7–15.
- Herr K, Bjoro K, Decker S: Tools for assessment of pain in nonverbal older adults with dementia: a state-of-the-science review. J Pain Symptom Manage 2006;31:170–192.
- Cole LJ, Farrell MJ, Duff EP, Barber JB, Egan GF, Gibson SJ: Pain sensitivity and fMRI pain-related brain activity in Alzheimer’s disease. Brain 2006;129:2957–2965.
- Benedetti F, Arduino C, Costa S, et al: Loss of expectation-related mechanisms in Alzheimer’s disease makes analgesic therapies less effective. Pain 2006;121:133–144.
- Day A, Fawcett WJ, Scott MJ, Rockall TA: Fast-track surgery and the elderly. Br J Anaesth 2012;109():124; author reply 124.
- Zwakhalen SM, Hamers JP, Abu-Saad HH, Berger MP: Pain in elderly people with severe dementia: a systematic review of behavioural pain assessment tools. BMC Geriatr 2006;6:3.
- While C, Jocelyn A: Observational pain assessment scales for people with dementia: a review. Br J Community Nurs 2009;14:438–442.
- Tsui BC, Wagner A, Finucane B: Regional anaesthesia in the elderly: a clinical guide. Drugs Aging 2004;21:895–910.
- Guay J: The benefits of adding epidural analgesia to general anesthesia: a meta-analysis. J Anesth 2006;20:335–340.
- Nishimori M, Low JH, Zheng H, Ballantyne JC: Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev 2012;7:CD005059.
- Marret E, Remy C, Bonnet F: Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. Br J Surg 2007;94: 665–673.
- Falzone E, Hoffmann C, Keita H: Postoperative analgesia in elderly patients. Drugs Aging 2013;30:81–90.
- Foss NB, Kristensen MT, Kristensen BB, Jensen PS, Kehlet H: Effect of postoperative epidural analgesia on rehabilitation and pain after hip fracture surgery: a randomized, double-blind, placebo-controlled trial. Anesthesiology 2005;102:1197–1204.
- Wu CL, Cohen SR, Richman JM, et al: Efficacy of postoperative patient-controlled and continuous infusion epidural analgesia versus intravenous patient-controlled analgesia with opioids: a meta-analysis. Anesthesiology 2005;103:1079–1088; quiz 1109–1010.
- Mann C, Pouzeratte Y, Boccara G, et al: Comparison of intravenous or epidural patient-controlled analgesia in the elderly after major abdominal surgery. Anesthesiology 2000;92:433–441.
- Luger TJ, Kammerlander C, Gosch M, et al: Neuroaxial versus general anaesthesia in geriatric patients for hip fracture surgery: does it matter? Osteoporosis Int 2010;21:S555–572.
- Ready LB, Chadwick HS, Ross B: Age predicts effective epidural morphine dose after abdominal hysterectomy. Anesth Analg 1987; 66:1215–1218.
- McLachlan AJ, Bath S, Naganathan V, et al: Clinical pharmacology of analgesic medicines in older people: impact of frailty and cognitive impairment. Br J Clin Pharmacol 2011;71:351–364.
- Macintyre PE, Upton R: Acute pain management in the elderly patient. In: Macintyre PE, Walker, SM, Rowbotham, DJ (eds): Clinical Pain Management: Acute Pain, 2nd ed. London: Hodder Arnold; 2008.
- Macintyre PE, Jarvis DA: Age is the best predictor of postoperative morphine requirements. Pain 1996;64:357–364.
- Woodhouse A, Mather LE: The influence of age upon opioid analgesic use in the patient-controlled analgesia (PCA) environment. Anaesthesia 1997;52:949–955.
- Gagliese L, Jackson M, Ritvo P, Wowk A, Katz J: Age is not an impediment to effective use of patient-controlled analgesia by surgical patients. Anesthesiology 2000;93:601–610.
- Upton RN, Semple TJ, Macintyre PE, Foster DJR: Population pharmacokinetic modelling of subcutaneous morphine in the elderly. Acute Pain 2006;8:109–116.
- Ishiyama T, Iijima T, Sugawara T, et al: The use of patient-controlled epidural fentanyl in elderly patients. Anaesthesia 2007;62:1246–1250.
- Coldrey JC, Upton RN, Macintyre PE: Advances in analgesia in the older patient. Best Pract Res Clin Anaesthesiol 2011;25:367–378.
- Herrick IA, Ganapathy S, Komar W, et al: Postoperative cognitive impairment in the elderly. Choice of patient-controlled analgesia opioid. Anaesthesia 1996;51:356–360.
- Narayanaswamy M, Smith J, Spralja A: Choice of opiate and incidence of confusion in elderly postoperative patients. Paper presented at: Annual Scientific Meeting of the Australian and New Zealand Society of Anaesthetists 2006; Adelaide, Australia.
- Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER: The impact of postoperative pain on the development of postoperative delirium. Anesth Analg 1998;86:781–785.
- Aubrun F, Marmion F: The elderly patient and postoperative pain treatment. Best Pract Res Clin Anaesthesiol 2007;21:109–127.
- Simon MJ, Veering BT, Stienstra R, van Kleef JW, Burm AG: The effects of age on neural block and hemodynamic changes after epidural anesthesia with ropivacaine. Anesth Analg 2002;94:1325–1330, table of contents.
- Simon MJ, Veering BT, Stienstra R, van Kleef JW, Burm AG: Effect of age on the clinical profile and systemic absorption and disposition of levobupivacaine after epidural administration. Br J Anaesth 2004;93: 512–520.
- Li Y, Zhu S, Bao F, Xu J, Yan X, Jin X: The effects of age on the median effective concentration of ropivacaine for motor block after epidural anesthesia with ropivacaine. Anesth Analg 2006;102:1847–1850.
- Crawford ME, Moiniche S, Orbaek J, Bjerrum H, Kehlet H: Orthostatic hypotension during postoperative continuous thoracic epidural bupivacaine-morphine in patients undergoing abdominal surgery. Anesth Analg 1996;83:1028–1032.
- Veering BT: Hemodynamic effects of central neural block in elderly patients. Can J Anaesth 2006;53:117–121.
- Gwirtz KH, Young JV, Byers RS, et al: The safety and efficacy of intrathecal opioid analgesia for acute postoperative pain: seven years’ experience with 5969 surgical patients at Indiana University Hospital. Anesth Analg 1999;88:599–604.
- Lim PC, Macintyre PE: An audit of intrathecal morphine analgesia for non-obstetric postsurgical patients in an adult tertiary hospital. Anaesth Intensive Care 2006;34:776–781.
- Blay M, Orban JC, Rami L, et al: Efficacy of low-dose intrathecal morphine for postoperative analgesia after abdominal aortic surgery: a double-blind randomized study. Reg Anesth Pain Med 2006;31: 127–133.
- Murphy PM, Stack D, Kinirons B, Laffey JG: Optimizing the dose of intrathecal morphine in older patients undergoing hip arthroplasty. Anesth Analg 2003;97:1709–1715.
- Rebel A, Sloan P, Andrykowski M: Retrospective analysis of high-dose intrathecal morphine for analgesia after pelvic surgery. Pain Res Manag 2011;16:19–26.
- Bujedo BM, Santos SG, Azpiazu AU: A review of epidural and intrathecal opioids used in the management of postoperative pain. J Opioid Manag 2012;8:177–192.
- Sultan P, Gutierrez MC, Carvalho B: Neuraxial morphine and respiratory depression: finding the right balance. Drugs 2011;71:1807–1819.
- Beaussier M, Weickmans H, Parc Y, et al: Postoperative analgesia and recovery course after major colorectal surgery in elderly patients: a randomized comparison between intrathecal morphine and intravenous PCA morphine. Reg Anesth Pain Med 2006;31:531–538.
- Zaric D, Boysen K, Christiansen C, Christiansen J, Stephensen S, Christensen B: A comparison of epidural analgesia with combined continuous femoral-sciatic nerve blocks after total knee replacement. Anesth Analg 2006;102:1240–1246.
- Fowler SJ, Symons J, Sabato S, Myles PS: Epidural analgesia compared with peripheral nerve block after major knee surgery: a systematic review and meta-analysis of randomized trials. Br J Anaesth 2008;100: 154–164.
- Paul JE, Arya A, Hurlburt L, et al: Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology 2010;113:1144–1162.
- Helms O, Mariano J, Hentz JG, et al: Intra-operative paravertebral block for postoperative analgesia in thoracotomy patients: a randomized, double-blind, placebo-controlled study. Eur J Cardiothorac Surg 2011;40: 902–906.
- Davies RG, Myles PS, Graham JM: A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural block for thoracotomy—a systematic review and meta-analysis of randomized trials. Br J Anaesth 2006;96:418–426.
- Scarci M, Joshi A, Attia R: In patients undergoing thoracic surgery is paravertebral block as effective as epidural analgesia for pain management? Interact Cardiovasc Thorac Surg 2010;10:92–96.
- Anwer HM, Swelem SE, el-Sheshai A, Moustafa AA: Postoperative cognitive dysfunction in adult and elderly patients-general anesthesia vs subarachnoid or epidural analgesia. Middle East J Anesthesiol 2006;18: 1123–1138.
- Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W: Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013; 118:934–944.
- Papaioannou A, Fraidakis O, Michaloudis D, Balalis C, Askitopoulou H: The impact of the type of anaesthesia on cognitive status and delirium during the first postoperative days in elderly patients. Eur J Anaesthesiol 2005;22:492–499.
- Rasmussen LS, Johnson T, Kuipers HM, et al: Does anaesthesia cause postoperative cognitive dysfunction? A randomised study of regional versus general anaesthesia in 438 elderly patients. Acta Anaesthesiol Scand 2003;47:260–266.
- Mason SE, Noel-Storr A, Ritchie CW: The impact of general and regional anesthesia on the incidence of post-operative cognitive dysfunction and post-operative delirium: a systematic review with meta-analysis. J Alzheimers Dis 2010;22:67–79.
- Del Rosario E, Esteve N, Sernandez MJ, Batet C, Aguilar JL: Does femoral nerve analgesia impact the development of postoperative delirium in the elderly? A retrospective investigation. Acute Pain 2008; 10:59–64.
- White PF, Kehlet H: Improving postoperative pain management: what are the unresolved issues? Anesthesiology 2010;112:220–225.
- Ilfeld BM: Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg 2011;113:904–925.
- Hanks RK, Pietrobon R, Nielsen KC, et al: The effect of age on sciatic nerve block duration. Anesth Analg 2006;102:588–592.
- Paqueron X, Boccara G, Bendahou M, Coriat P, Riou B: Brachial plexus nerve block exhibits prolonged duration in the elderly. Anesthesiology 2002;97:1245–1249.
- Akin S, Aribogan A, Turunc T, Aridogan A: Lumbar plexus block with ropivacaine for postoperative pain management in elderly patients undergoing urologic surgeries. Urol Int 2005;75:345–349.
- Cheema S, Richardson J, McGurgan P: Factors affecting the spread of bupivacaine in the adult thoracic paravertebral space. Anaesthesia 2003; 58:684–687.
- Daly DJ, Myles PS: Update on the role of paravertebral blocks for thoracic surgery: are they worth it? Curr Opin Anaesthesiol 2009; 22:38–43.
- Gao W, Ho YK, Verne J, Glickman M, Higginson IJ: Changing patterns in place of cancer death in England: a population-based study. PLoS Med 2013;10:e1001410.
- Snyder GL, Greenberg S: Effect of anaesthetic technique and other perioperative factors on cancer recurrence. Br J Anaesth 2010;105:106–115.
- Heaney A, Buggy DJ: Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis? Br J Anaesth 2012;109:i17–i28.
- Forget P, De Kock M: [Could anaesthesia, analgesia and sympathetic modulation affect neoplasic recurrence after surgery? A systematic review centred over the modulation of natural killer cells activity]. Ann Fr Anesth Reanim 2009;28:751–768.