Steve Roberts
INTRODUCTION
Peripheral nerve blocks have been gaining significant popularity in the daily practice among pediatric anesthesiologists. Nerve blocks in children have an excellent risk–benefit ratio and are readily acceptable by both parents and children. Although the performance of peripheral nerve blocks in anesthetized adults is often debated, such practice is well accepted in pediatric patients. Successive large prospective studies performed by the French-Language Society of Pediatric Anesthesiologists (ADARPEF) have demonstrated no increased incidence of complications when regional anesthesia techniques were performed under general anesthesia. The overall incidence of regional anesthesia–related complications was less than 0.9 of 1000 anesthetic procedures performed. Interestingly, a six-fold increase in the complication rate for central versus peripheral techniques was demonstrated, which should further persuade pediatric anesthesiologists to modify their practice toward more peripherally based regional anesthetic strategies. The complication rate was four times higher in children under 6 months of age; as such, these patients should be managed only by suitably trained specialist pediatric anesthesiologists. Because of the concomitant use of general anesthesia in children, the intraoperative efficacy of nerve blocks is often assessed indirectly using hemodynamic parameters and required depth of anesthesia. Most regional techniques used in children are primarily used for the purpose of providing postoperative pain control rather than surgical anesthesia.
Although most peripheral nerve blocks in children are performed in an operating room environment, their application extends to the emergency department as well as the intensive care unit (ICU) setting. Peripheral nerve blocks are also used in children with chronic pain conditions, such as chronic headache or chronic regional pain syndrome type 1 (CRPS-1). All adult regional anesthetic techniques are possible in children (Table 1); when these procedures are performed with skill and knowledge, their success rates and safety should not significantly differ from those in adults. This chapter will concentrate on the commonly performed pediatric blocks. For each technique, a short description of the relevant anatomy will be followed by descriptions of both landmark-based and ultrasound (US)-guided methods where appropriate. It is assumed for all blocks that appropriate monitoring, intravenous (IV) access, trained assistance, resuscitation equipment, and aseptic precautions are taken.
TABLE 1. Pediatric regional anesthetic techniques: common indications and suggested volume of local anesthetic.
| Block | Indication | Local Anesthetic Volume (mL/kg)a |
|---|---|---|
| Greater auricular | Otoplasty Mastoidectomy | 1.0–3.0 |
| Infraorbital | Cleft lip repair Endoscopic sinus surgery | Infants: 0.5–1.0 Children: 1.0–2.0 |
| Supraorbital and supratrochlear | Frontal scalp incisions; eg, simple minor plastic surgery, frontal craniotomy | 1.0–2.0 |
| Superficial cervical plexus | Otoplasty Tympanomastoid surgery Cochlear implant | 1.0–3.0 |
| Greater occipital | Posterior fossa surgery Occipital neuralgia, migraine headaches | 1.0–2.0 |
| Nerve of Arnold | Myringotomy | 0.5–1.0 |
| Interscalene | Shoulder surgery | 0.3–0.5 |
| Supraclavicular | Upper arm surgery | 0.3–0.5 |
| Infraclavicular | Upper arm surgery | 0.3–0.5 |
| Axillary | Elbow and forearm surgery | 0.3–0.5 |
| Median, ulna, and radial | Syndactyly surgery | 0.1–0.3 |
| TAP, unilateralb TAP, bilateralb | Open appendectomy Inguinal herniorrhaphy Colostomy formation Subumbilical midline laparotomy | 0.3–0.5 per side |
| Subcostal TAP | Cholecystectomy PEG | 0.3–0.5 per side |
| Rectus sheathc | Umbilical herniotomy Pyloromyotomyb | 0.2-0.3 per side |
| Ilioinguinal | Inguinal herniotomy | 0.2–0.3 |
| Penile | Circumcision Distal hypospadias | 0.1 per side |
| Unilateral paravertebral Bilateral Paravertebral | Thoracotomy; eg, TOF Renal surgery Sternotomy Pectus surgery | 0.3–0.5 per side |
| Intercostal | Chest drain insertion Thoroscopy | 0.5 |
| Lumbar plexus | Hip surgery | 0.5 |
| Femoral | Femoral fracture Slipped upper femoral epiphysis (combined with LFC) | 0.2–0.4 |
| Fascia iliaca | Femoral fracture Slipped upper femoral epiphysis | 0.5 |
| Lateral femoral cutaneous | Thigh muscle biopsy | 0.1 |
| Proximal sciaticd | Cruciate ligament repair | 0.3–0.5 |
| Popliteald | Tendon transfers/lengthening | 0.3–0.5 |
| Ankle | Syndactyly surgery | 0.1–0.2 |
| Digital nerve | Distal finger/toe surgery | 0.05–0.1 |
bSystemic analgesia for visceral pain is essential.
cAlways bilateral.
dDepending on the operation, a femoral or saphenous nerve block may be required for complete analgesia.
LFC, lateral femoral cutaneous; PEG, percutaneous endoscopic gastrostomy; TAP, transverse abdominis plane; TOF, tracheoesophageal fistula.
EQUIPMENT
Regional anesthesia in children must be performed only with the appropriate equipment. To this end, a selection of 18-gauge, short-beveled needles must be available; lengths of 40–50 mm and 90–100 mm will cover all patient ages. A short bevel is used as it improves the sensation of passing through tissues. The needle should be connected to a short extension tube to which a syringe can be attached; this prevents the needle being displaced as the injection is being made. Some anesthesiologists prefer to nick the skin with a sharp beveled needle to allow easy passage through the skin and ensure no superficial fascial clicks are missed.
A reliable nerve stimulator can be used to help locate mixed nerves for block. A nerve stimulator with adequate current output capable of eliciting percutaneous stimulation (eg, 5 mA/1 msec) for surface mapping is suggested. Once a needle is placed close to a nerve or plexus and proper stimulation is obtained, the current output is decreased to maintain the motor response at 0.4–0.2 mA to ensure intimate needle–nerve relationship. However, a number of recent human and animal studies have provided compelling evidence that peripheral nerve stimulation is not a specific determinate of the needle–nerve distance; indeed, it is possible for the needle to be placed intraneurally but have no motor response.
As an adjunct to peripheral nerve stimulation, objective injection pressure monitoring during local anesthetic injection may decrease the risk of intraneural injection.
The introduction of US to guide nerve blocks has significantly increased the efficacy of these techniques and may decrease the risk of neurologic and systemic complications (see Complications and Prevention of Neurologic Injury with Peripheral Nerve Blocks). Due to the superficiality of the structures in children, a US machine with a high frequency probe (> 13 MHz) should be available. When scanning children with very superficial structures, a 5-mm sterile US gel pad may allow better focusing of the US beam. Linear probes with a small footprint approximately 25 mm in length are a necessity to allow blocks to be performed on infants and children weighing less than 15 kg, as larger footprints tend to be too cumbersome in such patients. Because of the wide range of ages cared for in pediatric anesthesiology, a curvilinear probe will still need to be purchased to facilitate deep blocks (eg, lumbar plexus blocks in adolescents).
LOCAL ANESTHETICS
This chapter describes the use of local anesthetic solutions in children. It is imperative, however, to remember that the dosage of local anesthetic solutions should be on a milligram-per-kilogram basis and not based on total volume used (see Regional anesthesia in Pediatric Patients: General Considerations, Table 2), as is often the practice in regional anesthesia in adult population. Consideration should be given to using a more modern amino amide local anesthetic (eg, levobupivacaine or ropivacaine), particularly in neonates and infants and when infusions are planned. The dosage should be adjusted downward in infants and neonates owing to the decrease in protein binding and α1-acid glycoprotein, allowing for a greater amount of the free fraction of the drug in the systemic circulation. The addition of epinephrine to the local anesthetic solution may offer additional advantages by revealing intravascular placement, particularly in children under general anesthesia, and by prolonging local anesthetic action when used for peripheral nerve block.
Choosing the most appropriate concentration of local anesthetic for a given situation is imperative. In children, successful blocks can be provided using a medium concentration of amino amide (eg, 0.25% levobupivacaine). However, a weaker solution (eg, 0.125%) is more appropriate for neonates, when ambulation is important, and when there is a significant risk of compartment syndrome. In some circumstances, the administration of stronger concentrations of local anesthetic (eg, 0.5%) may be indicated; for example, when postoperative muscle spasms are a major issue.
NERVE LOCALIZATION METHODS
To assist standard landmark-based methods, a variety of techniques have been developed, including nerve stimulation, surface mapping, and ultrasonography. All techniques require a sound knowledge of anatomy.
Surface Mapping and Percutaneous Peripheral Nerve Stimulation
The most common method of nerve localization involves using a stimulating needle (sheathed needle). Mixed nerves can be identified percutaneously (surface mapping) and/or subcutaneously using a nerve stimulator. Surface mapping may decrease the number of needle insertions required. To elicit stimulation percutaneously, the nerve stimulator must have an adequate current output (eg, 5 mA/1 msec). The negative electrode is attached to the needle (black to block), and the positive electrode is attached to the patient (positive to patient). Prior to inserting the stimulating needle, it is possible to percutaneously stimulate and thus identify a superficial nerve’s position using a higher current and/or duration. To provide effective contact, the skin should be covered with a lubricating jelly or wiped with an alcohol swab. Once the needle is inserted, the nerve is located by trying to position the needle such that a current of 0.5 mA produces an appropriate muscle group response. The disadvantages of nerve stimulation are that it is a “blind” technique, is insensitive to intraneural injection, cannot be used in conjunction with muscle relaxants, is unreliable in children with neuromuscular conditions, and is painful if an awake block is being performed in the trauma setting. For these reasons, neurostimulation is being superseded by ultrasonography.
Ultrasonography
US-guided regional anesthesia has been with us for more than a decade; interest in this technology to aid in nerve localization has significantly increased, coinciding with increasing world-wide experience and the advances made in portable US equipment. US has been shown to reliably identify nerves and fascial planes in children, plan the safest needle trajectory, and visualize the dispersion of local anesthetic within the desired tissue planes. This technology, however, requires significant training and skill for its successful implementation; the success of US techniques is highly operator dependent. The key to the successful use of US is a specific training module and mentorship from a skilled practitioner. Although children are generally easier subjects to scan due to the superficial nature of their nerves, there are challenging morbidities (eg, cerebral palsy; Figure 1).
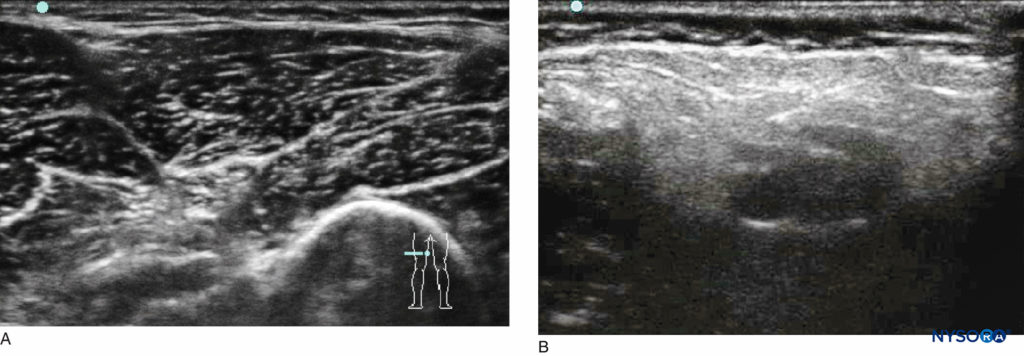
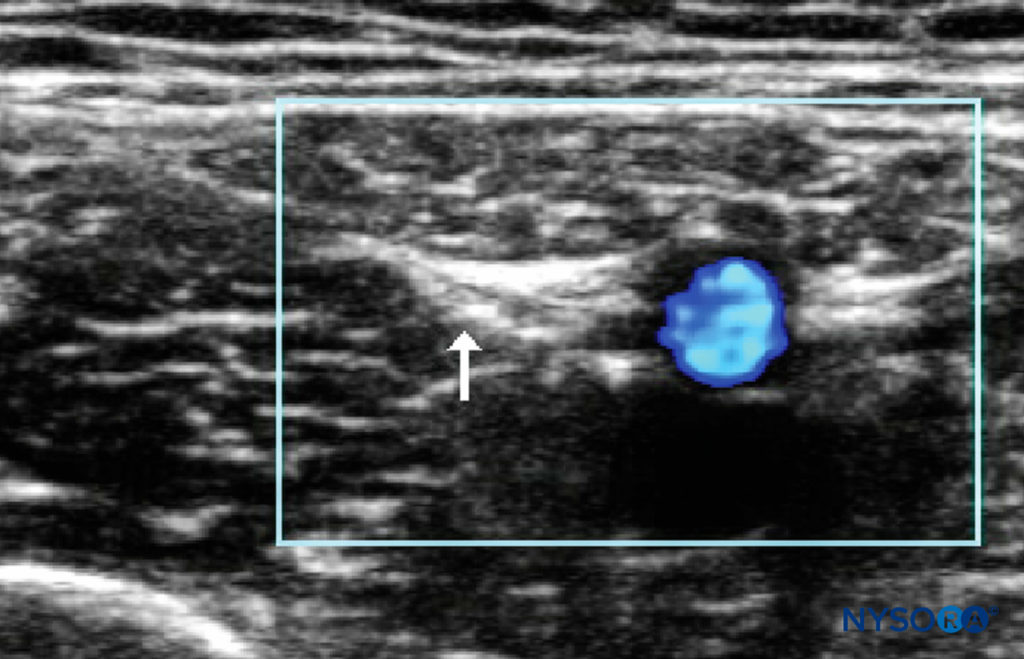
FIGURE 1. Comparison of US images of the popliteal fossae in (A) a healthy child and (B) a child with cerebral palsy.
To succeed with these difficult patients, the operator must have an established routine for each block, such that similar scan-ning conditions are used each time so that the expected US pattern is easily recognized.
For very superficial nerves, it may be beneficial to use a 5-mm sterile US gel pad to allow the US beam to better focus on the target nerve. When learning, and particularly with small children, it is useful to initially use saline to identify correct needle placement; in this way, no local anesthetic is wasted. (See Introduction to Ultrasound-Guided Regional Anesthesia for a detailed discussion of general US techniques.) Table 2 summarizes the advantages of US-guided regional anesthesia in children.
TABLE 2. Specic advantages of pediatric ultrasound-guided regional anesthesia.
| No ionizing radiation. |
| Because of the lower levels of ossification in pediatric patients, there are larger echo windows that can be used to visualize inside the spinal column. |
| Ultrasound allows for far lower doses of local anesthetic to be used, thereby reducing the risk of local anesthetic toxicity. |
| A lower volume of local anesthetic allows for multiple blocks to be performed within the maximum dose of local anesthetic. |
| In infants, the anatomy is compact and the risk of damage is greater; therefore, visualization of the nerve and adjacent structures makes for an inherently safer technique. |
Peripheral Nerve Catheter Techniques
Peripheral catheters are becoming increasingly popular in pediatric anesthesia, providing prolonged analgesia for surgery associated with moderate to severe postoperative pain. They are predominantly used for limb surgery, though they can be inserted for abdominal fascial plane blocks or indeed for simple wound irrigation. Other indications for the use of peripheral nerve catheters include the following:
- To facilitate intensive physiotherapy post–limb surgery
- To potentiate perfusion following reimplantation surgery
- To treat CRPS-1
- To manage nonsurgical pain (eg, epidermolysis bullosa)
- For palliative care (if the catheter is fixed correctly, it is the author’s experience that patients can be managed at home for as many months as is required)
Infective complications are rare and also less common than in adults; nevertheless, a strict aseptic technique should be used when placing peripheral nerve catheters. It is debatable whether it is helpful to make a space around the nerve for the catheter to be inserted into. With US, an advantage of making a space with local anesthetic is that the anesthesiologist knows that he or she has at least provided a reliable single injection of local anesthetic. The position of the catheter is confirmed by using a neurostimulating catheter or US. However, neurostimulating catheters are expensive, and their advantages are insignificant. When using US, it is often helpful to identify the catheter tip by scanning in both the transverse and longitudinal planes; local anesthetic or saline can then be injected and the spread assessed. Generally, no more than 2–3 cm of the catheter is inserted beyond the needle tip.
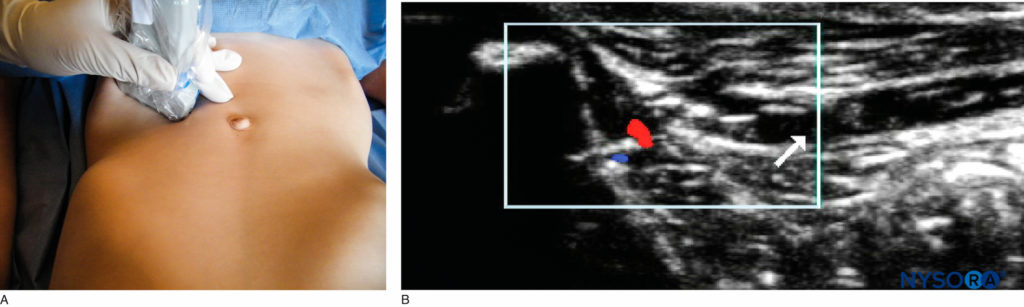
To ensure catheter security, tunneling should be performed for the majority of techniques (Figure 2). In addition, tissue glue should be applied to the original and secondary puncture sites to stop local anesthetic solution from leaking during infusion. Leakage of infusion causes the dressing to become wet and lift off the skin, leading to catheter dislodgement. Indermil or Dermabond glue can be used; the advantage of the latter is that it can be easily removed with yellow paraffin. It is usually a good idea to flush the catheter once it is tunneled and secured to ensure no kink has formed under the skin. The local anesthetic pump should be run intraoperatively so that any occlusion is detected prior to the patient being recovered.
As confidence has grown with nerve catheter techniques, their use in older children at home is being increasingly described; this has been aided by the development of disposable elastomeric pumps. A typical infusion prescription of 0.125% levobupivacaine or ropivacaine runs at 0.1–0.3 mL/kg/h. For fascial plane blocks that require volume to work, a local anesthetic bolus regime may be preferable to running an infusion. The postoperative analgesia management should be clearly documented and verbally handed over to the ward staff and parents or caregivers. It should include rescue analgesia (eg, Oramorph or diazepam 0.1mg/kg to a maximum of 5 mg) for muscle spasms, an antiemetic, and a proposed time and date to stop the peripheral nerve catheter infusion. When the peripheral nerve catheter infusion is stopped, the patient should be loaded with simple analgesics. If the patient is managing their pain 4–6 hours later, the catheter can be removed.
NYSORA Tips
- Children under 6 months of age should undergo regional anesthetic techniques only by anesthesiologists with specific training in pediatric regional anesthesia.
- Always use the most peripheral technique possible.
- When learning catheter techniques, begin with easier sites for catheter insertion, such as the femoral nerve.
- When learning US-guided techniques, and particularly with small children, it is useful to initially use saline to identify correct needle placement; in this way, no local anesthetic is wasted and overdose is prevented.
- For the best US images of very superficial structures, a 5-mm jelly pad is useful.
- Local anesthetic absorption may be greater with US-guided fascial blocks.
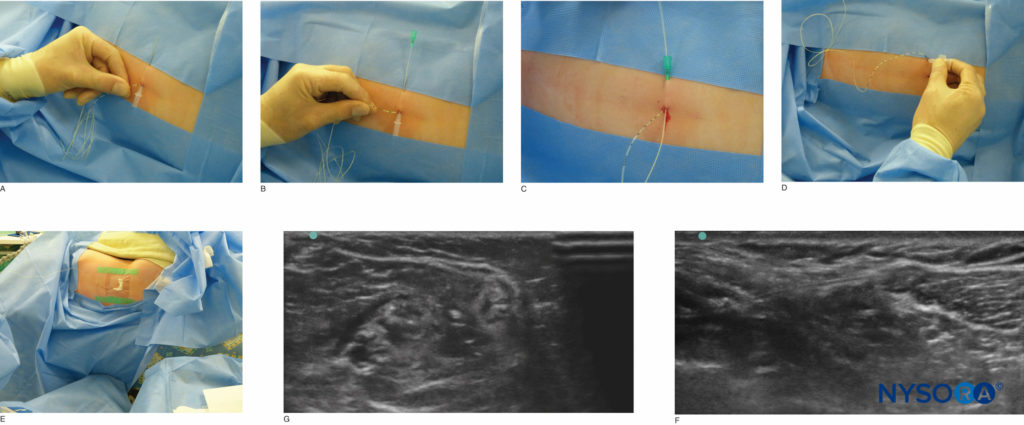
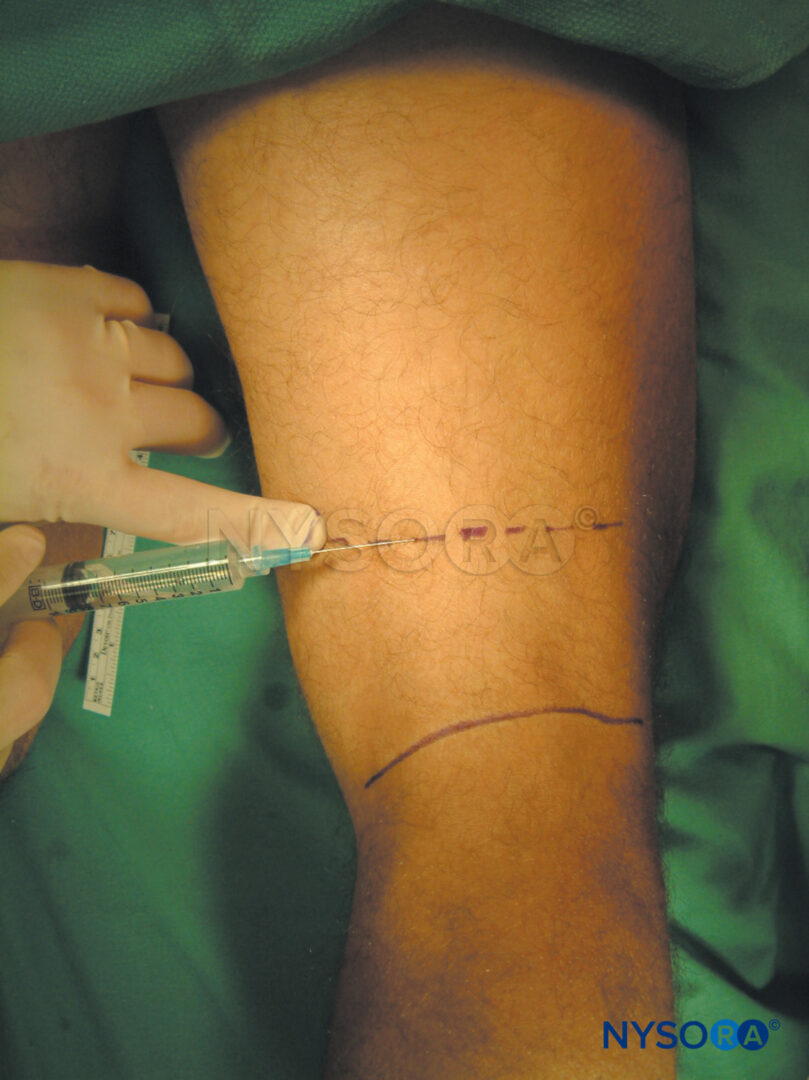
FIGURE 2. Tunneling of the popliteal catheter. The image in (F) illustrates an in-plane approach, whereas (G) illustrates an out-of-plane approach.
ANATOMICAL DIVISIONS
Head & Neck Blocks
The use of nerve blocks for various head and neck procedures is gaining in popularity, particularly in the pediatric popula-tion. Most of these blocks are sensory nerve blocks, which are easy to administer (field blocks) and virtually devoid of complications. They can, however, provide quality analgesia in the postoperative period, facilitating immediate postoperative recovery and pain management. Most of the innervation for the face and scalp is derived from the trigeminal nerve (cranial nerve V) and the cervical plexus (C2–C4).
V1 Division of the Trigeminal Nerve The supraorbital and supratrochlear nerves are branches of the first division of the trigeminal nerve that exit from the supraorbital foramen. The supraorbital nerve provides sensory innervation to the anterior portion of the scalp, except for the midportion of the forehead, which is innervated by the supratrochlear nerve. This block can be used for frontal craniotomies as well as for minor surgical procedures, including excision of scalp nevi.
Technique The supraorbital nerve can be easily blocked as it exits the supraorbital foramen; the block location is easily correlated to the midpoint of the pupil. When the foramen is located, a subcutaneous injection of local anesthetic solution (1–2 mL 0.25% bupivacaine with 1:200,000 epinephrine) is performed. Once the local anesthetic solution is injected, gentle pressure is maintained to decrease the risk of hematoma formation. Complications with this block are rare.
V2 Branch of the Trigeminal Nerve The second division of the trigeminal nerve is also referred to as the maxillary division of the trigeminal nerve. It exits from the maxillary foramen or the infraorbital foramen, which is located about 2 cm from the midline, and is usually aligned with the midpoint of the pupils. This nerve provides sensory supply to the upper lip, choana, maxillary sinus, part of the nasal septum, and tip of the nose. This block can be used to provide analgesia for cleft lip surgery, nasal septal repair, and endoscopic sinus surgery.
Technique There are two approaches to the maxillary division of the trigeminal nerve:
- Extraoral route: The needle is directed into the infraorbital foramen from an external location of the nerve. The foramen is located externally, and a 27-gauge needle is inserted into the foramen. After aspiration to rule out intravascular injection, 1–2 mL of local anesthetic solution is injected.
- Intraoral route: The nerve is accessed through the subsulcal area in the buccal mucosa. This is our preferred modality for blocking the infraorbital nerve. The upper incisor or the second bicuspid on the side to be blocked is located; a needle is passed via a subsulcal route toward the location of the infraorbital foramen. After careful aspiration, local anesthetic solution is injected. For infants scheduled for cleft lip repairs, we use 0.5 mL of local anesthetic solution for each side; for older children and adolescents, we use 1.5–2 mL of local anesthetic solution. The upper lip is likely to remain numb for several hours after the block, which can be disconcerting to patients. Care should be provided to prevent biting of the upper lip during the period of emergence from anesthesia.
V3 Mandibular Division of the Trigeminal Nerve The mandibular division of the trigeminal nerve provides analgesia for the lower jaw, lower lip, and portions of the temporo-parietal portions of the scalp. The most common nerve targeted in children is the mental nerve, which exits from the mental foramen located at the level of the midline in line with the pupil and the supraorbital and infraorbital foramina.
Technique An intraoral route is again preferred for placement of the mental nerve block. The needle is directed at the level of the lower incisor toward the infraorbital foramen; 1.5 mL of local anesthetic solution is then injected after careful aspiration. Gentle massage of the area is carried out after the injection.The auriculotemporal nerve supplies the lateral scalp and is blocked at the midpoint between the pinna and the angle of the eye. A block of this nerve involves a subcutaneous injection of 1–2 mL of local anesthetic solution.
Greater Occipital Nerve The greater occipital nerve is a branch of cervical root C2. The nerve pierces the aponeurosis and traverses medially to the occipital artery inferiorly and crosses over to the lateral aspect of the artery superiorly by the nuchal line as it innervates the posterior portions of the scalp. A greater occipital nerve block can be used for providing adequate block of the scalp for posterior fossa craniotomies as well as for patients with chronic occipital neuralgia.
Technique The occipital protuberance is palpated. The midline is identified, and the occipital artery is palpated. A 27-gauge needle is inserted, and a subcutaneous injection of local anesthetic solution is performed (1.5–2 mL of 0.25% bupivacaine with 1:200,000 epinephrine). The area is massaged gently after the injection. Complications are rare with this technique.
Ultrasound-Guided Technique The US-guided technique is the same as that used for adults (see Nerve Blocks of the Face). A linear probe of 10 MHz or more is used to identify the obliquus capitis, and the nerve can be found superficial to the muscle.
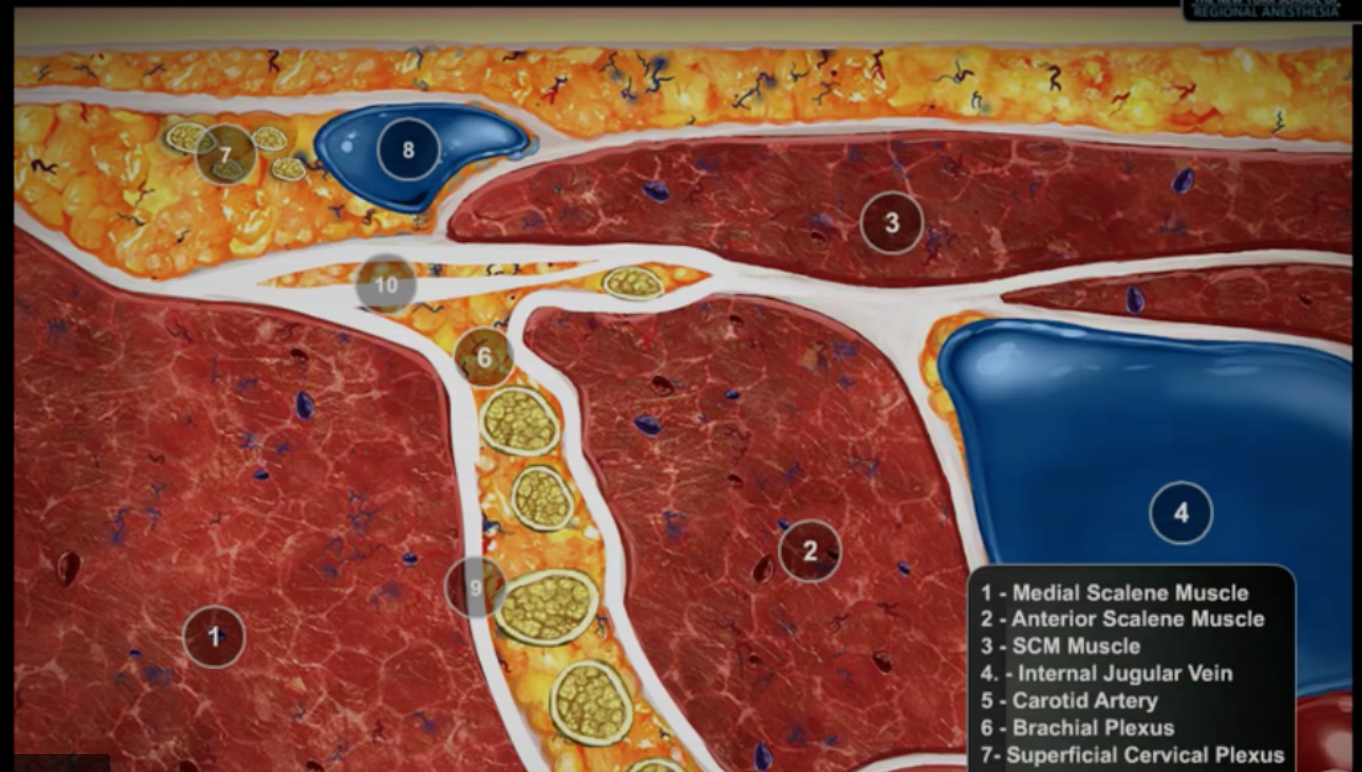
Superficial Cervical Plexus The superficial cervical plexus is a pure sensory nerve derived from the C2–C4 nerve roots. It wraps around the belly of the sternocleidomastoid at the level of the cricoid and divides into four branches: the lesser occipital supplying the posterior auricular area; the great auricular supplying the mastoid area and the pinna; the transverse cervical supplying the anterior portion of the neck; and the superficial cervical supplying the skin over the shoulder in a cape-like distribution over the shoul-der joint. block of the superficial cervical plexus can provide good postoperative analgesia for tympanomastoid surgery, otoplasty, thyroid surgery, and for procedures performed on the anterior portion of the neck. The use of this nerve block decreases the use of opioids in the perioperative period, thereby decreasing the incidence of nausea and vomiting.
Technique The technique is essentially identical to that used in the adult patient. The clavicular head of the sternocleidomastoid is identified, and a line drawn from the cricoid cartilage to intersect the posterior border of the sternocleidomastoid is identified. A subcutaneous injection of local anesthetic solution (1–3 mL of 0.25% bupivacaine with epinephrine 1:200,000) is performed. Caution must be exercised during injection because of the close proximity of the nerve to the external jugular vein. Deep injections should be avoided to prevent potential injection into the deep cervical plexus, which is associated with adverse effects including recurrent laryngeal nerve paralysis, paralysis of the hemidiaphragm, and Horner syndrome as a result of unilateral sympathetic ganglion block. Complications, though rare, are related to deep cervical plexus block and intravascular injection. (See Cervical Plexus Block for a more detailed description of this technique.)
Ultrasound-Guided Technique The US-guided is the same as that used for adults (see Ultrasound-Guided Cervical Plexus Block).
Nerve of Arnold The nerve of Arnold is the auricular branch of the vagus nerve; it supplies sensory innervation to the auditory canal and the lower half of the tympanic membrane. A block of this nerve provides analgesia for myringotomy. Using a fine needle, 0.5–1 mL of local anesthetic is injected into the cartilage of the posterior tragus.
Upper Extremity Blocks
A complete review of the anatomy of the brachial plexus is provided in Functional Regional Anesthesia Anatomy and Ultrasound-Guided Interscalene Brachial Plexus Block, Supraclavicular Brachial Plexus Block, Infraclavicular Brachial Plexus Block and Axillary Brachial Plexus Block. There are multiple approaches to the brachial plexus in children. Although the interscalene block is often used in adults for surgical procedures of the shoulder, this approach is used infrequently in children. This is due to the limited indications and increased incidence of complications associated with the use of the interscalene approach in children. The most common approaches to the brachial plexus in children include the supraclavicular, infraclavicular, and axillary approaches. The complications described include hematoma, intravascular injection, intraneural injection, and pneumothorax for the periclavicular blocks. Except for the axillary approach, all approaches should always be performed under US guidance. Often, these blocks are being performed on children with severe musculoskeletal complaints (eg, fixed contractures, muscles absent or fibrosed); in these patients, US is superior to neurostimulation in terms of its ability to define individual anatomy. For prolonged analgesia, peripheral catheters can be easily fixed in the supraclavicular or infraclavicular region.
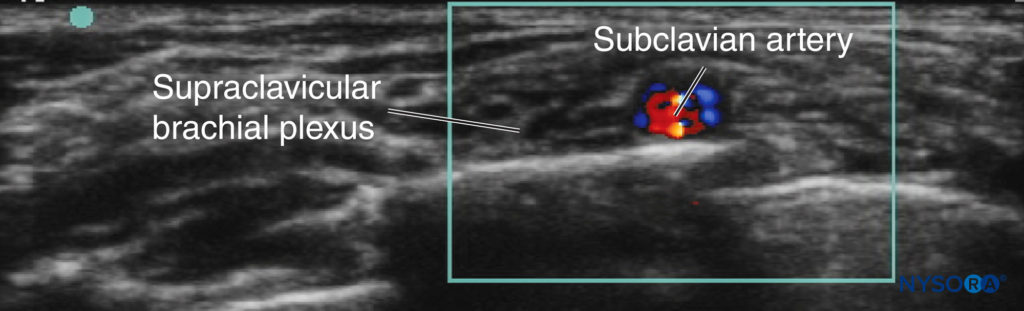
Supraclavicular Approach In the close anatomical relationships of children, only small probe movements are required to change from an interscalene view to a supraclavicular view. Prior to US, this block had been underused in children due to the close proximity of the cervical pleura. However, with appropriate training and mentorship, the sonoanatomy (Figure 3) becomes easy to understand, and the block generally becomes technically easy to perform. It is recommended that this block be performed only with the use of US.
Ultrasound-Guided Technique In the US-guided supraclavicular approach, the child is placed supine with a head ring and shoulder roll; this arrangement creates enough room for the anesthesiologist’s needling hand to approach from the posterior aspect. In the younger child, the first rib may not be fully ossified. Always use Doppler to identify potentially dangerous vessels in the proposed needle trajectory. The probe is positioned parallel to and touching the clavicle and is angled caudad, aiming into the thorax. An in-plane needling technique from the posterolateral to anteromedial direction is employed (see Figure 3).
Infraclavicular Approach The US-guided infraclavicular approach is second choice to the supraclavicular approach as the brachial plexus is generally deeper at this point and an out-of-plane technique is employed. However, an infraclavicular approach is indicated if the supraclavicular fossa is inaccessible or there is local infection. US guidance is recommended for this approach (see Ultrasound-Guided Infraclavicular Brachial Plexus Block for more detail).
Axillary Approach The axillary approach to the brachial plexus is the most commonly used landmark-based approach in children and adolescents and is used for procedures on the arm and hand. The primary advantage of the axillary approach is the relatively lower risk of complications. However, there is a 40–50% chance of missing the musculocutaneous nerve with this approach, owing to the proximal exit of this nerve from the axillary sheath. Hence, while performing a block using this approach, the musculocutaneous nerve should be blocked separately when analgesia of the biceps and anterior forearm is sought. Peripheral nerve catheters in the axilla are difficult to immobilize and protect from bacterial colonization. A US-guided technique has been described but differs little from the adult technique described in Ultrasound-Guided Axillary Brachial Plexus Block.
Technique There are several techniques for placing an axillary block. The commonly used approaches include the transar-terial approach and the nerve stimulation approach. Although greater success with the transarterial approach has been reported in adults, this approach is not often used in children, due to the higher incidence of vessel spasm and increased potential for ischemia in children versus adults. Although many methods have been reported in adults, the simple, common single-injection technique seems to be effective in children.
For this technique, the patient is positioned with the arm abducted 90 degrees. The elbow is flexed, and the arm is placed above the head. A stimulating needle is inserted superior to the axillary artery at an angle of 30 degrees, with the tip pointed toward the midpoint of the clavicle. A “pop” may be felt as the needle enters the axillary sheath. After eliciting a response to nerve stimulation at 0.5 mA, local anesthetic solution is injected. A volume of 0.3–0.5 mL/kg is recommended, to a maximum of 20 mL. When anesthesia of the musculocutaneous nerve is required to augment this block, the needle is directed above the pulse of the axillary artery and toward the belly of the coracobrachialis muscle. Contraction of the biceps confirms placement of the needle close to the musculocutaneous nerve.
Nerve Block at the Wrist block of the radial, ulnar, and median nerves can be accomplished at the level of the wrist. The advantage of these peripheral blocks is the absence of motor block. They are used primarily for surgery on the hand, such as syndactyly repair. These blocks are performed in conjunction with general anesthesia, since tourniquet pain cannot be eliminated with this block alone. (See Ultrasound-Guided Wrist Block and Wrist Block for more information on the US-guided and landmark-based techniques, respectively; these techniques are essentially identical to those used in adults.) With US, the nerves can be blocked at any point along their path. The following discussion outlines some specific issues that relate to the landmark application of wrist blocks in pediatric patients.
Radial Nerve The radial nerve is a superficial sensory nerve proximal to the radial head. The radial nerve divides into two branches: the thenar branch and the dorsal branch. This division takes place proximal to the distal end of the radius. This block is performed for children undergoing trigger thumb release or minor surgical procedures involving the thumb and index finger.
Technique The anatomical “snuff box” is identified, and local anesthetic is infiltrated subcutaneously approximately 2 cm proximal to the this location. A volume of 2 mL is adequate to provide good analgesia in the postoperative period.
Median Nerve The median nerve is located between the tendons of the palmaris longus and the flexor carpi radialis. The nerve can be blocked at the level of the flexor retinaculum or at midforearm level. One of the important anatomical advantages of blocking the median nerve at the wrist is the presence of a bursa at the level of the flexor retinaculum. This bursa encompasses the median nerve; hence, block of this nerve can be carried out without damage to the nerve.
Technique The tendons of the flexor carpi radialis and the palmaris longus are identified. Flexion of the wrist identifies the tendons. A 27-gauge needle is inserted at the medial border of the palmaris longus tendon. A “pop” is felt as the bursa is entered. An injection of 2 mL of local anesthetic solution is made. Smaller quantities are used in younger children and infants.
Ulnar Nerve The palmar cutaneous branch of the ulnar nerve accompanies the ulnar artery to the wrist. It perforates the flexor retinaculum and ends in the palm, communicating with the median nerve.
Technique The nerve is easily blocked at the wrist. The flexor carpi ulnaris tendon is identified. The nerve is blocked under the flexor carpi ulnaris tendon, just proximal to the pisiform bone. A 27-gauge needle is passed under the flexor carpi ulnaris, proximal to the pisiform bone, about 0.5 cm. After aspiration, 2 mL of local anesthetic solution is injected.
Lower Extremity Blocks
The lumbar plexus and sacral plexus supply the lower extremity. The lumbar plexus is contained in the psoas compartment and consists of a small portion of T12 and lumbar nerves L1–L4. The femoral, lateral femoral cutaneous, and obturator nerves are branches of the lumbar plexus and supply most of the thigh and upper leg. The lower leg is innervated by the sacral plexus, which is derived from the anterior rami of L4, L5, S1, S2, and S3. The sacral plexus gives rise to the sciatic nerve, which is the largest nerve in the body. The complications of lower extremity blocks described include hematoma, intravascular injection, and intraneural injection. The landmark/nerve stimulation method is made difficult in cerebral palsy patients in whom there are limb contractures and absent or hypoplastic or fibrosed muscles. The contractures are occasionally so severe that it is nearly impossible to gain access to perform the block.
Femoral Nerve The femoral nerve block is the most commonly performed lower extremity peripheral nerve block in children. It is used to provide pain relief after femoral fractures, Ilizarov frame placement, patellar ligament realignment, and slipped upper femoral epiphysis fixation. The femoral nerve is located at the level of the crease at the groin, lateral to the pulsation of the femoral artery.
Technique The technique for this block is similar to that used in adults (see Femoral Nerve Block). The femoral artery pulse is located, and the needle is inserted immediately lateral to the pulse to elicit a quadriceps muscle contraction. The nerve stimulator is initially set at 1 mA and then reduced to 0.5 mA while observing the quadriceps contraction. The location of the needle is stabilized and aspiration performed repeatedly as 0.2–0.4 mL/kg of local anesthetic is injected.
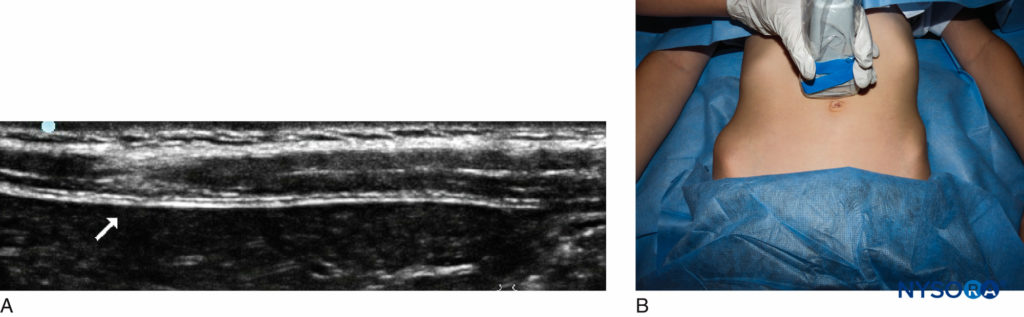
Ultrasound-Guided Technique The patient is positioned supine, with the anesthesiologist on the side of the intended nerve block, facing the US machine opposite. The linear probe is placed just below and parallel to the inguinal ligament. Using minimal transducer pressure to avoid collapsing vessels, Doppler is used to identify the superficial circumflex iliac artery, as this artery frequently passes superficially to the femoral nerve (Figure 4). The needle is introduced in plane from a lateral to medial direction, aiming to just “pop” the fascia iliaca as it spreads over the femoral nerve. Note that more than two “pops” are often felt and that repeated test injections of 0.5 mL may be required to ensure that the correct plane has been located. If required, the needle can then be rotated 180 degrees to block the lateral femoral cutaneous nerve.
Lateral Femoral Cutaneous Nerve The lateral femoral cutaneous nerve is derived from L3 and L4 segments of the lumbar plexus. It is a pure sensory nerve and passes superficially along the lateral border of the iliac crest. It appears from beneath the inguinal ligament medial to the anterior superior iliac spine, travelling between the fascia lata and the fascia iliaca. It supplies the skin of the lateral aspect of the buttock and the anterolateral aspect of the thigh below the greater trochanter. A lateral femoral cutaneous nerve is useful for providing analgesia for surgery on the lateral aspect of the thigh, including muscle biopsies and graft excisions.
Note that the lateral femoral cutaneous nerve does not supply the skin of the thigh above the greater trochanter; this area is supplied by branches of the L1 and T12 nerve roots. If the incision is to extend this cephalad, a superficial infiltration around the upper lateral aspect of the thigh or a transverse abdominis plane (TAP) (T12–L1) block may be required. Where children have undergone previous hip surgery, scarring can make both the landmark- and US-based techniques difficult. The technique for this block is similar to that used in adults (see Ultrasound-Guided Lateral Femoral Cutaneous Nerve Block).
Technique The anterior superior iliac spine is identified. A point 1–2 cm below and medial to the anterior superior iliac spine is identified. After careful aseptic preparation of the area, a blunt needle is introduced into the marked site. Once the needle is through the skin, a “pop” is felt as the needle pierces the fascia lata. Once the needle is lodged within this space, loss of resistance may be felt as the local anesthetic solution is injected. A total volume of 0.1 mL/kg (to a maximum of 5 mL) of local anesthetic solution is injected.
Ultrasound-Guided Technique A reliable location to identify the nerve is 10–20 mm below the anterior superior iliac spine, in the groove between the sartorius muscle and the tensor fascia lata. The lateral femoral cutaneous nerve is a small hyperechoic nerve (Figure 5). Note that the nerve may pass through the ligament or laterally to the anterior superior iliac spine.
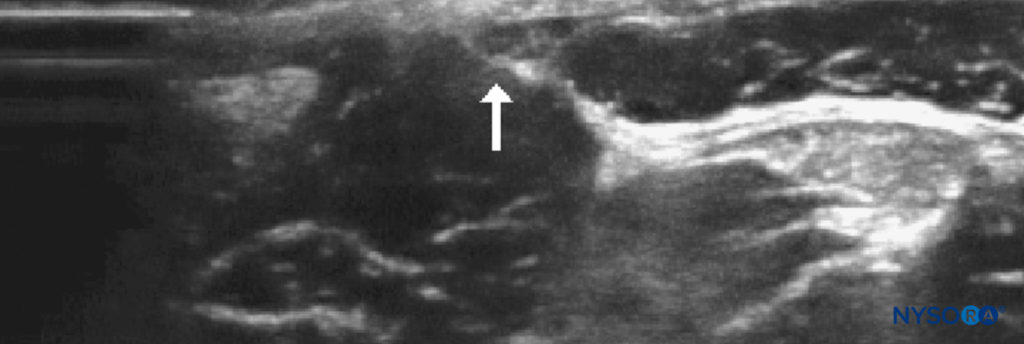
FIGURE 5. Lateral cutaneous nerve of the thigh in a 6-year-old: probe position and relevant sonoanatomy.
Sciatic Nerve The sacral plexus comprises the sciatic nerve and provides inner-vation to the posterior thigh, leg, and most of the foot, except the medial portion, which is innervated by the femoral nerve. A number of techniques are used in children for a sciatic nerve block. When choosing which level to block the nerve, it is essential that the most distal approach be chosen. Tourniquet pain is rarely a problem in children, as they are under general anesthesia. Further, distal nerve components are more likely to be missed if a proximal block is performed, thus creating a “patchy” block. We will address two techniques: the subgluteal and the popliteal fossa approaches. However, with US, the sciatic nerve can essentially be blocked at whichever level is appropriate to the surgery and where the nerve is easiest to visualize.
Subgluteal Approach This approach is indicated for hamstring releases and anterior cruciate ligament repairs. Catheter placement is straightforward; it is helpful to tunnel the catheter laterally subcutaneously 30–40 mm. Placing a tourniquet over the catheter is not problematic, though care should be taken on removal of the tourniquet to prevent catheter dislodgement by the surgeon.
Technique The subgluteal sciatic nerve block can be per-formed either in the lateral (operative side uppermost) or supine position with the limb elevated. The subgluteal line where the gluteal crease is present is marked. The biceps femoris tendon is identified, and a point inferior to the gluteal crease, just medial to the biceps femoris tendon, is delineated. A sheathed needle connected to a nerve stimulator is introduced in an anterior plane and cephalad at an angle of 60–70 degrees. Inversion of the foot indicates block of the tibial nerve.
The current is then reduced to 0.4 mA, and if inversion is still present, the local anesthetic solution is injected. If eversion is noted, the needle is withdrawn to the skin and inserted medially. If the biceps femoris tendon is contracting, the needle is drawn back to the skin and inserted medially, away from the muscle belly of the biceps femoris tendon. Plantar flexion is also an indicator of adequate block placement, although this yields a potential for failed block. A volume of 0.3–0.5 mL/kg (to a maximum of 20 mL) is injected into the space. On initial injection of 1 mL of local anesthetic solution, the twitch disap-pears, confirming correct needle placement.
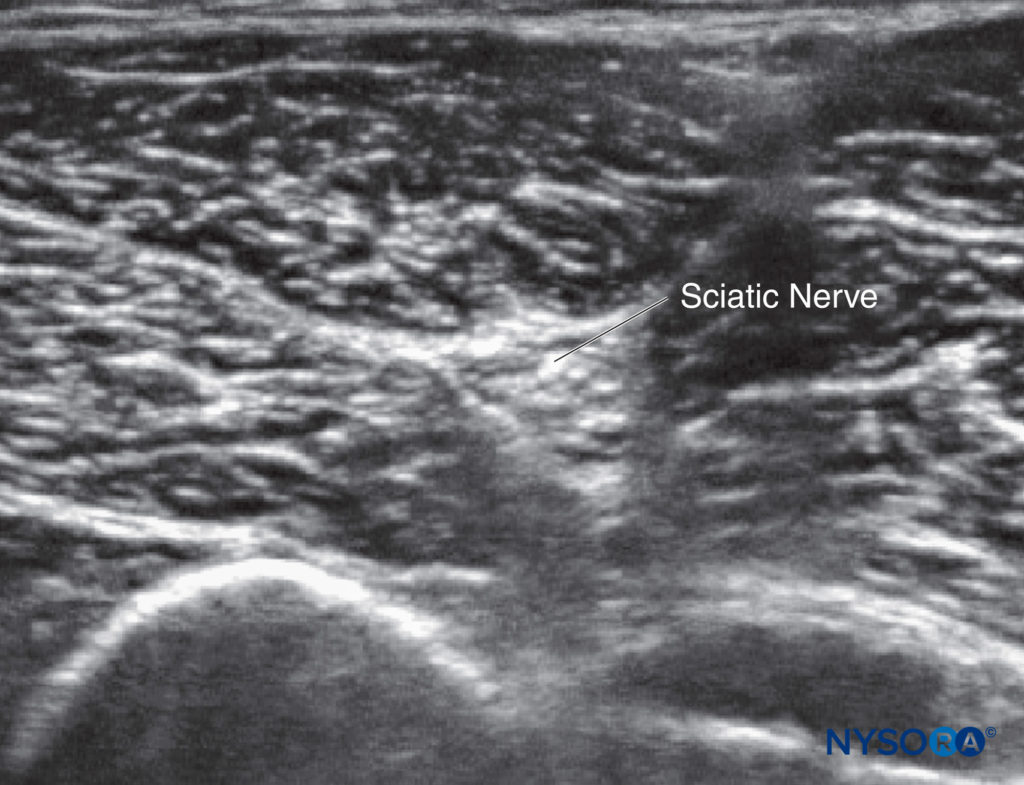
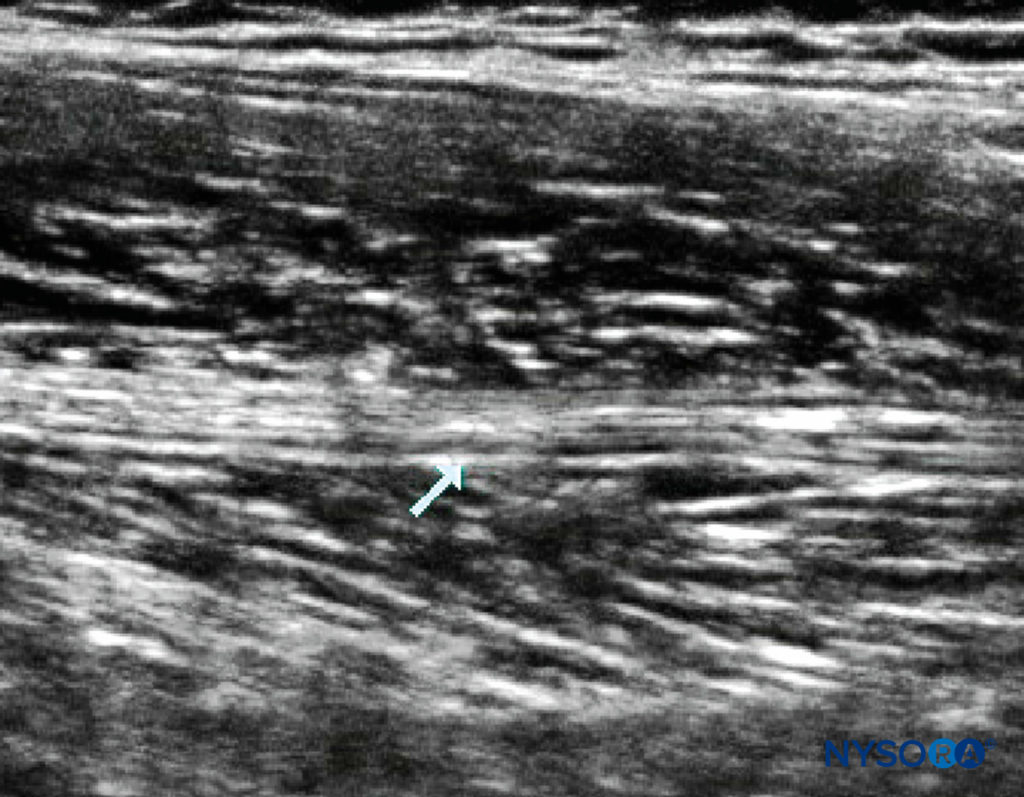
Ultrasound-Guided Technique A linear probe suffices in all but the largest adolescent. Applying probe pressure improves the US image, as this brings the sciatic nerve closer to the probe (Figure 6). Visualizing the nerve may be difficult in arthrogrypotic children, in whom it may be obscured by fibrosis. Where there is difficulty identifying the nerve, a longitudinal scan from medial to lateral and back may be attempted, looking for a band of hyperechogenicity (Figure 7). Once the sciatic nerve identified, rotate the probe back into the transverse plane. Alternatively, track down distally to the popliteal fossa, and identify the nerve before retracing your steps. With US, it is often possible to see the posterior cutaneous branch of the thigh, medial and superficial to the sciatic nerve, and it is important to ensure the local anesthetic covers it. An in-plane technique is advisable for single injections, whereas an out-of-plane technique is often better for catheter placement. When placing catheters, first inject one-third of the available local anesthetic by the lateral aspect of the nerve; the remaining two-thirds is used medially to make space for the catheter. This technique ensures the nerve is surrounded.
Popliteal Fossa Block The indications for popliteal block include trauma surgery and correction of congenital abnormalities. In conjunction with a saphenous nerve block, the lower limb below the knee can be completely anesthetized.
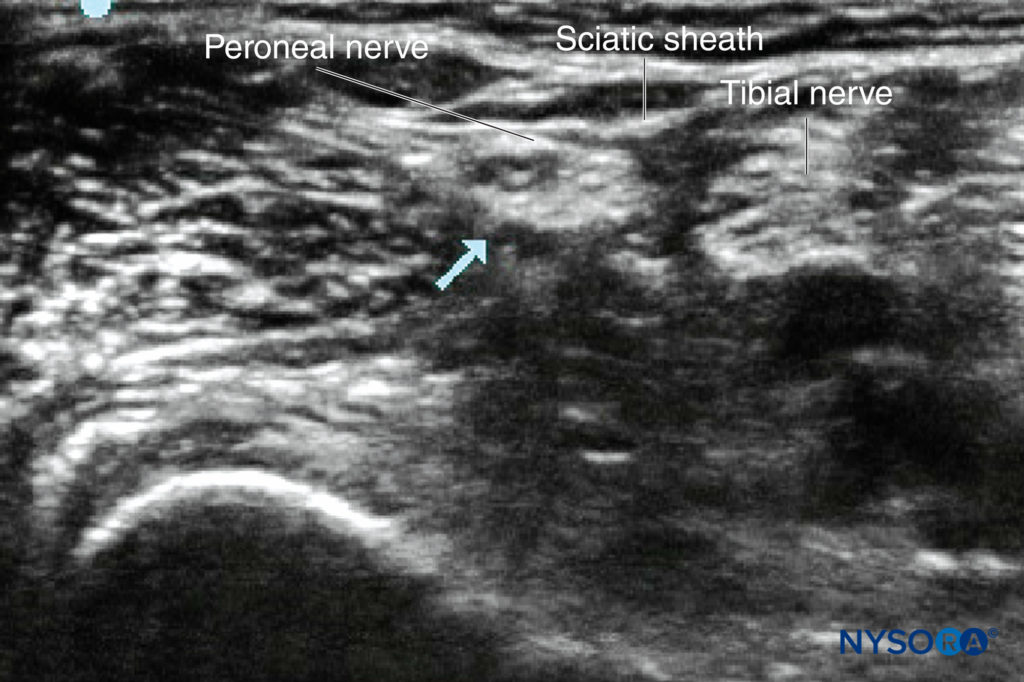
The popliteal fossa is a diamond-shaped area with the superior triangle formed by the tendons of the semitendinosus and semimembranosus medially and the biceps femoris tendon laterally. The sciatic nerve divides into the common peroneal nerve and the tibial nerve. The common peroneal nerve exits the popliteal fossa laterally, and the tibial nerve exits medially. The branching of the sciatic nerve takes place at varying levels above the popliteal crease. A common epineural sheath is present that envelops both the tibial and common peroneal nerve; as a result, complete block of both branches may result.
Technique The patient is positioned laterally (operative side uppermost to allow for better needle access), with the lower knee flexed or prone. The needle is inserted at the apex of the popliteal fossa, lateral to the artery. A response to nerve stimulation at 0.4 mA confirms the position of the needle and its proximity to the sciatic nerve. The tibial nerve is localized by the presence of inversion and plantar flexion (internal nerve = inversion); the common peroneal nerve is localized by the presence of eversion and dorsiflexion (external nerve = eversion). After aspiration to rule out intravascular placement, local anesthetic solution is injected. A volume of 0.5 mL/kg is injected (to a maximum volume of 20 mL).
Ultrasound-Guided Technique The patient is positioned as described above, though, when supine, in many children with cerebral palsy, the leg will rotate externally sufficiently to allow the nerves to be approached medially. Children with flexed flexion deformities will not display the “see-saw” sign. For a single injection, an in-plane technique is recommended, from either the medial or lateral aspect of the leg. With US, the exact level of sciatic nerve branching can be identified; at this point, the combined circumference of the two nerves will be greater than the circumference of the “sciatic” nerve; a block at this location provides greater local anesthetic–nerve contact (Figure 8). For catheter insertion, an out-of-plane approach is preferred by the author; with a view to threading the catheter along the axis of the nerve, position can be checked in the longitudinal view. The catheter should be inserted at the level of sciatic nerve division.
Ankle The ankle block is a very common and easy block to perform in children undergoing foot surgery. There are five main nerves to be blocked: the posterior tibial, deep peroneal, superficial peroneal, saphenous, and sural (Figure 9). All these nerves are distal branches of the sciatic nerve, except for the saphenous nerve, which is a branch of the femoral nerve. The nerves are superficial and therefore do not require much volume. Epinephrine should not be added to the local anesthetic solution because end arteries are present at the site of injection (see Ankle Block for illustrations and a detailed description of the ankle block).
A US-guided approach is also possible. Ideally, a probe with a small footprint and a frequency of 15 MHz or more should be readily available, but unfortunately, many of the highest-frequency probes have large footprints and do not readily sit on a small ankle. Once again, a sterile US gel pad may aid visualization.

FIGURE 9. Transducer position for a block of the (A) posterior tibial nerve; (B) superficial peroneal nerve; and (C) deep peroneal nerve.
Tibial Nerve The tibial nerve is the largest nerve supplying the plantar aspect of the foot and is an important nerve to be blocked for any foot surgery. We routinely use surface mapping with a current of 5 mA to locate the tibial nerve before injection. The nerve is located behind the posterior tibial pulsation, below the medial malleolus. A 27-gauge needle is advanced to the bone and slightly withdrawn to avoid injection into the periosteum; 2–5 mL of local anesthetic solution is then injected. Alternatively, a sheathed needle can be used, and plantar flexion or inversion can be elicited before injection.
Saphenous Nerve The saphenous nerve is the distal cutaneous branch of the femoral nerve. It is located superficially, anterior to the medial malleolus. A superficial ring is injected along the medial malleolus, and 2–5 mL of local anesthetic solution is injected. Caution must be exercised to avoid intravascular injection, as the saphenous vein courses alongside the nerve. The saphenous nerve supplies the skin over the medial aspect of the leg below the knee and ankle. When performing a US-guided saphenous nerve block, it may be easier to find the nerve lateral to the artery, at the level of the adductor canal in the thigh, just before the vessels enter the posterior compartment (Figure 10). At this level, the nerve to the vastus medialis will also be blocked.
Deep Peroneal Nerve The peroneal nerve innervates the first web space of the foot. It can be blocked by depositing local anesthetic solution lateral to the extensor hallucis longus tendon. The needle is advanced until the periosteum of the tibia is encountered, then drawn back slightly. A volume of 2–3 mL of local anesthetic solution is then injected. When using US, the nerve is more easily found by identifying the dorsalis pedis artery and tracking the artery proximally until it lies on the distal tibia; at this point, the nerve can be seen travelling over the artery.
Superficial Peroneal Nerve The superficial peroneal nerve supplies sensory supply to the dorsum of the foot. It is superficial and can be easily blocked by injecting a superficial ring of local anesthesia between the lateral malleolus and the extensor hallucis longus tendon. This nerve is more easily visualized with US at the midcalf level, where it lies subcutaneously; it can be readily tracked back into the popliteal fossa, where it joins to form the common peroneal nerve.
Sural Nerve The sural nerve supplies sensory innervation to the lateral aspect of the foot. It can be easily blocked by injecting local anesthetic solution between the lateral malleolus and the calcaneus. This nerve is very difficult to visualize with US.
Digital Nerve Blocks
A digital nerve block is provided for analgesia of the fingers and toes. It is an ideal block for simple procedures such as trigger finger release and ingrown toenail excision and for foreign body removal and minor lacerations requiring suturing. We have used these blocks successfully for analgesia after laser therapy for warts in children. The digital nerve block technique is addressed in Digital block.
Hand Anatomy The common digital nerves of the hand are derived from the median and ulnar nerves and divide in the palm to supply the fingers. All digital nerves are accompanied by digital vessels. The median nerve provides three digital nerves. The first common palmar digital nerve divides into the three palmar digital nerves that supply the side of the thumb; the second common palmar digital nerve supplies the web space between the index and middle fingers, and the third common palmar digital nerve communicates with the ulnar nerve to supply the web space between the middle and ring fingers. These nerves then become the proper digital nerves that supply the skin of the distal phalanx. There are also smaller digital nerves derived from the radial and ulnar nerves that supply the dorsum of the fingers. The four dorsal digital nerves are located on the ulnar side of the thumb and the radial side of the index finger, adjacent to the index and middle fingers. All digital nerves terminate in two main branches: one supplying the skin under the fingertips, and the other supplying the pulp under the nail.
Technique The digital nerves are blocked using non–epinephrine-containing solution on each side of the finger at the bifurcation between the metacarpal heads. A dorsal or volar injection accomplishes similar results. A needle is inserted into the web space between the thumb and index finger to a distance of about 1 cm. A second needle is inserted into the thenar eminence on the radial aspect of the thumb. For the other fingers, the needle is inserted between the metacarpal heads. A needle is inserted proximal to the thenar web space at the distal palmar crease. After aspiration, 1 mL of local anesthetic solution (without epinephrine) is injected.
Complications A large volume of local anesthetic solution is contraindicated as it can cause vascular compromise.
Feet Anatomy The digital nerves to the feet are derived from the plantar cutaneous branch of the tibial nerve. The proper digital nerve of the toe supplies the medial aspect of the great toe. The three common digital nerves split into two proper digital nerves each. The first supplies the adjacent areas of the great and second toes, the second supplies the adjacent sides of the second and third toes, and the third supplies the adjacent sides of the third and fourth toes. Each of these terminates at the tip of the toe. A branch from the superficial peroneal nerve supplies the dorsum of the foot. This is derived from two nerves: (1) the dorsal cutaneous nerve, which divides into two branches, a medial branch supplying the great toe and a lateral branch supplying the adjacent sides of the second and third toes; and (2) the intermediate dorsal cutaneous nerve, which passes along the lateral part of the foot, supplying the lateral aspect of the foot and communicating with the sural nerve. The two dorsal digital terminal branches supply the adjacent parts of the third and fourth toes and another branch supplying the adjacent sides of the fourth and fifth toes.
Technique It is easy to block the digital nerves by accessing the web space on the dorsolateral aspect of the foot. It is best to avoid these blocks in children who may have compromised blood flow to the toes. Vasoconstrictors are to be avoided for all these blocks.
Trunk Blocks
For most surgery involving truncal blocks, there will be an element of visceral pain that is not covered. Therefore, all children should receive some systemic analgesic adjuncts (eg, paracetamol and ibuprofen). Remember that with US-guided fascial blocks, local anesthetic absorption may be greater than with standard landmark-based techniques.
Ilioinguinal/Iliohypogastric Nerve The ilioinguinal/iliohypogastric nerve block is indicated for inguinal hernia, orchidopexy, and varicocele surgery.
Anatomy The ilioinguinal and iliohypogastric nerves origi-nate from the T12 (subcostal nerve) and L1 (ilioinguinal, iliohypogastric) nerve roots of the lumbar plexus. These nerves pierce the internal oblique aponeurosis 2–3 cm medial to the anterior superior iliac spine. The ilioinguinal nerve travels between the internal oblique and the external oblique aponeuroses. Here, it accompanies the spermatic cord and is part of the neurovascular bundle to the genital area. US studies have shown that there is no relationship between a child’s weight and the depth or position of the nerves.
Technique A line is drawn between the umbilicus and anterior superior iliac spine. A point is marked 2 mm medial from the anterior superior iliac spine. The needle is advanced toward the inguinal canal and passed in until a “pop” is felt. Local anesthetic solution is then injected into the area after aspiration. US studies have shown that blind administration usually does not inject the local anesthetic into the correct fascial plane between the internal oblique and transversus abdominis muscles; yet, clinically, the majority of blocks work, presumably due to the diffusion of the local anesthetic. Alternatively, an ilioinguinal nerve block can be performed by the surgeon; the disadvantage of this is the need for a deeper plane of general anesthesia intraoperatively.
Ultrasound-Guided Technique The probe is placed on a line from the anterior superior iliac spine to the umbilicus, with the lateral end of the probe resting on the bone (Figures 11). With practice, the nerves can be tracked more proximally toward the midaxillary line, which prevents the local anesthetic spreading too far into the surgeon’s field and disrupting their tissue planes. Experts in this field have managed to successfully block these nerves with a volume of local anesthetic as little as 0.075 mL/kg.
Complications An ilioinguinal/iliohypogastric nerve block is relatively safe. Perforation of the bowel wall can occur, however, and has been reported. Femoral nerve block may occur in up to 11% of cases; therefore, all ambulant children should be tested for weight bearing prior to discharge.
Rectus Sheath A rectus sheath block (Figure 12) is useful in children for umbilical area surgery (eg, umbilical hernia, pyloromyotomy, duodenal atresia). It must be performed bilaterally, as the nerves cross over the midline from each side. The technique is essentially the same as that used in adults but requires a greater degree of finesse when performed in neonates, in whom muscle thickness may be as little as 2 mm.
Anatomy The umbilical area is innervated by the tenth thoracoabdominal intercostal nerves from the right and left sides. Each nerve passes behind the costal cartilage and between the transverse abdominis and the internal oblique muscles. The nerve runs between the sheath and the posterior wall of the rectus abdominis muscle and ends at the anterior cutaneous branch, supplying the skin of the umbilical area. The rectus muscle is attached anteriorly to the sheath at three intertendinous intersections; however, posteriorly there are no attachments, and it is this which allows the spread of local anesthetic.
Technique The aim of this block is to deposit local anesthetic solution between the muscle and the posterior aspect of the sheath. The technique has been well described by Ferguson et al. A 23-gauge needle is inserted above or below the umbilicus, 0.5 cm medial to the linea semilunaris in a perpendicular plane. The anterior rectus sheath is identified by moving the needle in a back-and-forth motion until a scratching sensation is felt and the rectus sheath is identified and entered. After the belly of the muscle is entered, the needle is farther advanced until the posterior aspect of the rectus sheath is appreciated with a scratching sensation as the needle is moved again in a back-and-forth motion. Once the sheath is felt, it is entered, and local anesthetic solution is deposited posterior to the sheath. The usual depth of needle entry is about 5–15 mm. After aspiration, 0.2–0.3 mL/kg of bupivacaine 0.25%–0.5% is injected on each side.
If resistance to injection is felt, the needle is advanced deeper, as resistance may indicate that the needle is within the body of the muscle. Caution should be taken, as US studies have shown that the depth from the skin to the posterior sheath is independent of age and weight. Indeed, the distance is rarely greater than 10 mm in children under 10 years of age.
Ultrasound-Guided Technique This block can be performed with a greater degree of precision with the assistance of US. The anatomy is easy to understand, and the sonoanatomy is simple, with no anisotropy to contend with. As such, this block is an ideal one to teach a beginner, though initially older children should be practiced on. With practice, the anesthesiologist should be able to block both sides without having to swap his or her position or that of the US machine. An in-plane technique is ideally suited to this block, aiming from lateral to medial. Care should be taken when choosing the needle insertion point; it should be sufficiently lateral to allow a shallow needle trajectory. In this way, the needle tip can be slid into the potential space between muscle and sheath and avoid a trajectory down toward the abdominal cavity. Prior to needling, Doppler should be used to assess the position of the inferior epigastric artery; this is easily found lying deep to the muscle at the level of the arcuate line. It can then be tracked cephalad into the muscle belly. A volume of 0.1 mL/kg is sufficient to provide analgesia for an umbilical hernia; more extensive midline incisions will require greater volume. Holding the probe in a paramedian longitudinal plane, the local anesthetic spread can be readily assessed passing beneath the intertendinous intersections caudad and cephalad.
Anatomy The lateral abdominal wall consists of three muscles. From the peritoneum outward are the fascia transversalis and then the transversus abdominis, internal oblique, and external oblique muscles. The neurovascular plexus is fixed to the outer surface of transversus abdominis by a thick fascial sheet. It is unclear whether this must be breached for the block to be successful. Local anesthetic injected into the TAP will usually cover the T11–L1 segmental nerves and will also cover T10 50% of the time.
Ultrasound-Guided Technique The patient is positioned supine, with the anesthesiologist standing on the side to be blocked and the US machine placed opposite. For bilateral blocks, it is unnecessary to change positions. The probe is placed over the midaxillary line, between the iliac crest and costal margin in a transverse plane. Count the muscle layers from inside out; if the layers are identified from out to in, it is easy to mistake a subcutaneous layer for a muscle layer, particularly in obese patients. An in-plane technique is used (Figure 13). If it is difficult to place the needle tip within the correct plane, insert the needle carefully into the transversus abdominis muscle; as you withdraw, have an assistant inject. As the needle tip enters the correct plane, loss of resistance will be felt.
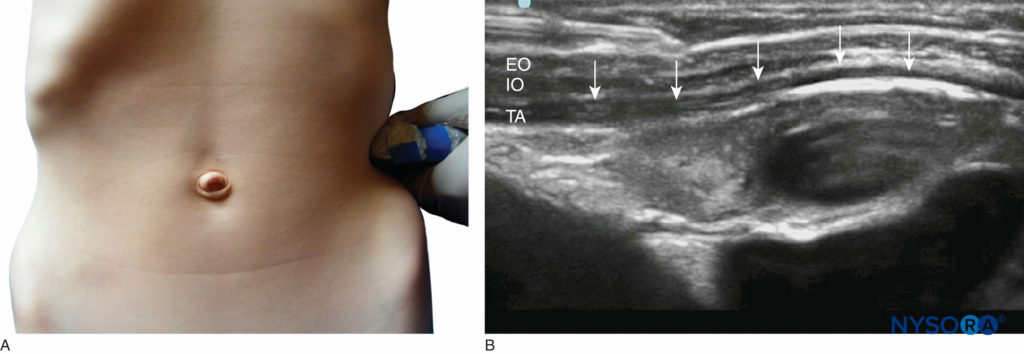
FIGURE 13. Transverse abdominis plane block: (A) probe position; (B) sonoanatomy. Arrows indicate TAP plane between transverse abdominis (TA); internal oblique muscles (IO); and external oblique (EO).
Penile Nerve A penile nerve block is indicated for circumcision and distal hypospadias repair (where a caudal block is contraindicated). The sensory innervation of the penis is derived from the pudendal nerve. The pudendal nerve gives rise to the dorsal nerves of the penis; these are accompanied by vessels medially as they enter the subpubic space at the level of the symphysis pubis before traveling distally to supply sensation to the shaft of the penis. The two nerves and their accompanying vessels are separated from one another by the suspensory ligament of the penis, hence the requirement for a bilateral approach. The subpubic space is roofed by Scarpa’s fascia, a deep membranous continuation of the superficial abdominal fascia. A US-guided technique has been described but did not improve on the efficacy of the landmark-based technique. Epinephrine-containing solutions and ropivacaine, with its intrinsic vasoconstrictive properties, should not be used for penile nerve blocks.
Technique The subpubic approach requires the penis to be gently retracted downward to make the Scarpa’s fascia taut. Just below the symphysis pubis, a needle is inserted 5–10 mm lateral to the midline and advanced slightly caudally until a “pop” is felt as the needle enters the fascial compartment bounded superficially by Scarpa’s fascia. Depth varies from 5–30 mm and is independent of both the age and weight of the child. After careful aspiration, 0.1 mL/kg of plain local anesthetic is injected (to a maximum of 5 mL). The injection is then repeated on the other side of the midline. Some anesthesiologists recommend infiltrating the ventral aspect of the shaft of the penis for a more reliable block.An alternative approach is to place a subcutaneous ring block around the base of the penile shaft. Although a simpler technique, it is associated with a higher incidence of inadequate postoperative pain relief.
Complications The most feared complication associated with penile nerve block is hematoma formation.
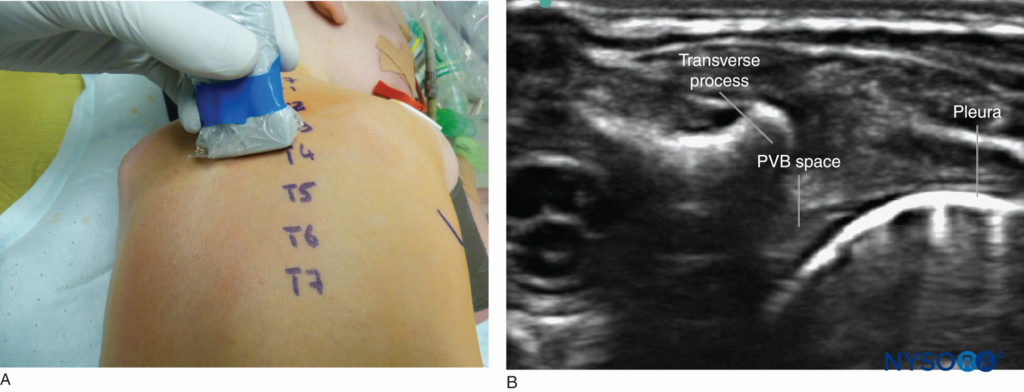
Thoracic Paravertebral Space Thoracic paravertebral blocks should be performed only by specialist pediatric regional anesthesiologists. Both single-injection and catheter techniques have been described. Indications for this block include postoperative thoracotomy pain, sternotomy, and unilateral abdominal surgery (eg, open splenectomy, nephrectomy). Contraindications for this technique include severe coagulopathy, local infection, previous ipsilateral thoracic surgery (a relative contraindication), and previous total pleurectomy, as local anesthetic will not stay within the paravertebral space. Empyema or localized tumor near the injection site should be carefully considered to avoid seeding malignant cells or infection. An 18-gauge pediatric (50-mm length with 5-mm markings) epidural kit is suitable for all pediatric patients, except for infants and neonates, for whom a 19-gauge kit is preferred.
Anatomy The thoracic paravertebral space is wedge-shaped. The base of the wedge is formed by the vertebral body and intervertebral discs. Posteriorly, it is bound by the costotransverse ligament; anterolaterally, it is bordered by parietal pleura. The costotransverse ligament is attached from the inferior edge of the transverse process to the superior edge of the rib tubercle. Laterally, it is continuous with the internal intercostal membrane (the aponeurosis of the internal intercostal muscle). The paravertebral space is filled with fatty tissue, through which the intercostal nerves and vessels, dorsal rami, rami communicantes, and sympathetic chain pass. The paravertebral space is connected laterally to the intercostal space and medially to the epidural space. The paravertebral space is limited inferiorly at T12 by the origin of the psoas major muscle.
Technique The patient is positioned in the lateral decubitus position in the neutral position, with the operative side uppermost; for bilateral blocks, the patient is positioned prone. Needle insertion should be at the level of T4 for sternotomy (a bilateral block is required), T6 for thoracotomy, T9 for renal surgery, and T12 and L1 for inguinal surgery. The needlepoint is typically positioned 1–2 cm lateral to the midline or equivalent to the interspinous process distance of the patient. The depth to the paravertebral space is estimated as 20 + (0.5 × weight in kg) mm. The needle is inserted through the skin, and the stylet is removed. A syringe of saline is attached for assessment of loss of resistance. The needle is advanced until the transverse process is contacted. At this point, the needle is advanced 1 cm past the transverse process. Alternatively, the syringe is advanced until the loss of resistance is appreciated. A bolus of 0.3–0.5 mL/kg of 0.25% bupivacaine is injected. The same technique can be used to insert a paravertebral catheter for continuous infusion.
Ultrasound-Guided Technique The patient is positioned as for the landmark-based technique. The probe is placed in a transverse plane over the spinous process at the desired level of needle insertion. The level is easily determined by counting down from C7 (the vertebra prominens). The probe is slid laterally to identify the transverse process and then moved caudad, between the transverse processes, to visualize the paravertebral space. The pleura is readily identifiable moving with respiration; superficial to this, forming the posterior border of the paravertebral space, is the internal intercostal membrane (Figure 14).
An in-plane lateral-to-medial needling technique is employed, which requires excellent needle visualization skills, as the needle is being directed toward the spinal cord. A “pop” is seen and felt as the needle penetrates the membrane. Local anesthetic spread caudad and cephalad can be assessed by scanning in a paramedian longitudinal plane. In neonates, it may be possible to see spread into the epidural space.
Complications The potential complications of this block are serious and include pneumothorax. As such, this block should be performed only by or under the supervision of a pediatric regional anesthesiologist. Other complications include hypotension (4.6% of cases), vascular puncture, and inadvertent epidural or intrathecal injection.
SUMMARY
Peripheral nerve blocks can be performed with ease in children and adolescents. Adequate knowledge of the anatomy of the area along with appropriate indications and knowledge of complications facilitate the use of peripheral nerve blocks in children. The fear of the use of peripheral nerve blocks in children under general anesthesia is not unfounded, but US guidance may make complications even less frequent than reported with current methods. With time, US-guided approaches will become the gold standard of regional anesthesia techniques.
REFERENCES
- Giaufre E, Dalens B, Gombert A: Epidemiology and morbidity of regional anesthesia in children: A one-year prospective survey of the French-LanguageSociety of Pediatric Anesthesiologists. Anesth Analg 1996;83:904–912.
- Ecoffey C, Lacroix F, Giaufre E et al. Epidemiology and morbidity of regional anesthesia in children: a follow-up one year prospective survey ofthe French-Language Society of Pediatric Anaesthesiologists (ADARPEF). Pediatr Anesth 2010; 20:1061–1069.
- Berde CB, Sethna NF, Levin L, et al: Regional analgesia on pediatric medical and surgical wards. Intensive Care Med 1989;15(Suppl 1):S40–S43.
- Tobias JD: Continuous femoral nerve block to provide analgesia following femur fracture in a paediatric ICU population. Anaesth Intensive Care 1994;22:616–618.
- Urmey WF, Stanton J. Inability to consistently elicit a motor response following sensory paresthesia during interscalene block administration. Anesthesiology 2002; 96: 5.
- Chan VW, Brull R, McCartney CJL et al. An Ultrasonographic and Histological Study of Intraneural Injection and Electrical Stimulation in Pigs. Anesth Analg 2007;104:1281-4 52–4.
- Hadzic A, Dilberovic F, Shah S, et al: Combination of intraneural injection and high injection pressure leads to fascicular injury and neurologicdeficits in dogs. Reg Anesth Pain Med 2004;29:417–423.
- Freid EB, Bailey A, Valley R: Electrocardiographic and hemodynamic changes associated with unintentional intravascular injection of bupivacainewith epinephrine in infants. Anesthesiology 1993;79:394–398.
- Bosenberg AT, Raw R, Boezaart AP: Surface mapping of peripheral nerves in children with a nerve stimulator. Paediatr Anaesth 2002;12:398–403.
- Marhofer P, Sitzwohl C, Greher M, Kapral S: Ultrasound guidance for infraclavicular brachial plexus anaesthesia in children. Anaesthesia 2004;59:642–646.
- Tsui B and Suresh S. Ultrasound Imaging for Regional Anaesthesia in Infants, Children and Adolescents. Anaesthesiology 2010;112: 473–492.
- Kirchmair L, Enna B, Mitterschiffthaler G, et al: Lumbar plexus in children. A sonographic study and its relevance to pediatric regionalanesthesia. Anesthesiology 2004;101:445–450.
- Dadure C and Capdevila X. Peripheral catheter techniques. Paediatric Anaesthesia 2012; 22: 93–101.
- Suresh S, Bellig G: Regional anesthesia in a very low-birth-weight neonate for a neurosurgical procedure. Reg Anesth Pain Med 2004;29:58–59.
- Suresh S, Wagner AM: Scalp excisions: Getting “ahead” of pain. Pe-diatr Dermatol 2001;18:74–76.
- Prabhu KP, Wig J, Grewal S: Bilateral infraorbital nerve block is superior to peri-incisional infiltration for analgesia after repair of cleft lip. Scand J Plastic Reconst Surg Hand Surg 1999;33:83–87.
- Molliex S Navez M, Baylot D, et al: Regional anesthesia for outpatient nasal surgery. Br J Anaesth 1996;76:151–153.
- Suresh S, Patel AS, Dunham, ME, et al. A randomized double-blind controlled trial of infraorbital nerve block versus intravenous morphine sulfatefor children undergoing endoscopic sinus surgery: Are postoperative outcomes different? Anesthesiology 2002;97:A-1292.
- Yasan H, Dogru H: Effect of infraorbital nerve block under general anesthesia on consumption of isoflurane and postoperative pain in endoscopicendonasal maxillary sinus surgery by Higashizawa and Koga. J Anesth 2003;17:68.
- Higashizawa T, Koga Y: Effect of infraorbital nerve block under general anesthesia on consumption of isoflurane and postoperative pain inendoscopic endonasal maxillary sinus surgery. J Anesth 2001;15:136–138.
- Suresh S, Barcelona SL, Young NM, et al: Postoperative pain relief in children undergoing tympanomastoid surgery: Is a regional block better thanopioids? Anesth Analg 2002;94:859–862.
- Cregg N, Conway F, Casey W: Analgesia after otoplasty: Regional nerve block vs local anaesthetic infiltration of the ear. Can J Anaesth 1996;43(2):141–147.
- Dieudonne N, Gomola A, Bonnichon P, Ozier YM: Prevention of postoperative pain after thyroid surgery: Adouble-blind randomized study of bilateralsuperficial cervical plexus blocks. Anesth Analg 2001;92:1538–1542.
- Suresh S, Templeton L: Superficial cervical plexus block for vocal cord surgery in an awake pediatric patient. Anesth Analg 2004;98:1656–1657.
- De Jose Maria B, Banus E, Navarro Egea M et al. Ultrasound-guided supraclavicular vs infraclavicular brachial plexus blocks in children. Pediatr Anesth 2008; 18: 838–844.
- Ting PL, Sivagnanaratnam V: Ultrasonographic study of the spread of local anaestheticduring axillary brachial plexus block. Br J Anaesth 1989;63:326–329.
- Aantaa R, Kirvela O, Lahdenpera A, Nieminen S: Transarterial brachial plexus anesthesia for hand surgery: A retrospective analysis of 346 cases. JClin Anesth 1994;6:189–192.
- Carre P, Joly A, Cluzel FB, et al: Axillary block in children: Single or multiple injection? Paediatr Anaesth 2000;10:35–39.
- Dalens B, Tanguy A, Vanneuville G: Lumbar plexus block in children: A comparison of two procedures in 50 patients. Anesth Analg 1988;67: 750–758.
- Grossbard GD, Love BR: Femoral nerve block: A simple and safe method of instant analgesia for femoral shaft fractures in children. Aust N Z J Surg 1979;49:592–594.
- Johnson CM: Continuous femoral nerve block for analgesia in children with femoral fractures. Anaesth Intensive Care 1994;22:281–283.
- Ronchi L, Rosenbaum D, Athouel A, et al: Femoral nerve block in children using bupivacaine. Anesthesiology 1989;70:622–624.
- Flack S, Anderson C. Ultrasound guided lower extremity blocks. Pediatr Anesth 2012; 22:72–80.
- Maccani RM, Wedel DJ, Melton A, Gronert GA: Femoral and lateral femoral cutaneous nerve block for muscle biopsies in children. Paediatr Anaesth 1995;5:223–227.
- Sukhani R, Candido KD, Doty R Jr, et al: Infragluteal-parabiceps sciatic nerve block: An evaluation of a novel approach using a single-injectiontechnique. Anesth Analg 2003;96:868–873.
- Vloka JD, Hadzic A, April E, Thys DM: The division of the sciatic nerve in the popliteal fossa: Anatomical implications for popliteal nerveblock. Anesth Analg 2001;92:215–217.
- Vloka JD, Hadzic A, Lesser JB, et al: A common epineural sheath for the nerves in the popliteal fossa and its possible implications for sciaticnerve block. Anesth Analg 1997;84:387–390.
- Schwemmer U, Markus CK, Greim CA et al. Sonographic imaging of the sciatic nerve and its division in the popliteal fossa in children. PaediatrAnaesth 2004; 14(12):1005–1008.
- van Schoor A-N, Bosman MC, Bosenberg AT. Revisiting the anatomy of the ilio-inguinal/iliohypogastric nerve block. Paediatr Anaesth 2013;23(5): 390–394.
- Weintraud M, Marhofer P, Bosenberg A et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic withoutdirect visualization? Anesth Analg 2008; 106:89–93.
- Willschke H, Marhofer P, Bosenberg AT et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth 2005; 95:226–30.
- Willschke H, Bosenberg AT, P. Marhofer, et al. Ultrasonographic-Guided Ilioinguinal/Iliohypogastric Nerve Block in Pediatric Anesthesia: What isthe Optimal Volume? Anesth Analg 2006;102:1680–4.
- Amory C, Mariscal A, Guyot E, et al: Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth 2003;13:164–136.
- Leng SA: Transient femoral nerve palsy after ilioinguinal nerve block. Anaesth Intensive Care 1997;25:92.
- Ferguson S, Thomas V, Lewis I: The rectus sheath block in paediatric anaesthesia: New indications for an old technique? Paediatr Anaesth 1996;6:463–466.
- De Jose Maria B, Gotzens V, Mabrok M. Ultrasound-guided umbilical nerve blocks in children: a brief description of a new technique. Pediatr Anesth 2007; 17:44–50.
- Carney J, Finnerty O, Rau J et al. Ipsilateral transversus abdominis plane block provides effective analgesia after appendicectomy in children: arandomised controlled trial. Anesth Analg 2010;111(4):998–1003.
- Hebbard P. Subcostal Transversus Abdominis Plane Block Under Ultrasound Guidance. Anesth Analg 2008;106(2):673–674.
- Carney J, Finnerty O, Rauf J et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011; 66:1023–1030.
- Holder KJ, Peutrell JM, Weir PM: Regional anaesthesia for circumcision. Subcutaneous ring block of the penis and subpubic penile block compared. Eur J Anaesthesiol 1997;14:495–498.
- Richardson J and Lonnqvist PA. Thoracic Paravertebral Block. Br J Anaesth 1998; 81: 230–238.
- Lönnqvist PA. Continuous paravertebral block in children. Initial experience. Anaesthesia 1992 Jul;47(7):607–9.
- Riain SC, Donnell BO, Harmon DC et al. Thoracic Paravertebral Block Using Real-Time Ultrasound Guidance. Anesth Analg 2010; 110 (1): 248–251.
- Marhofer P, Kettner SC, Hajbok L et al. Lateral ultrasound-guided paravertebral block: an anatomical-based description of a new technique. Br JAnaesth 2010; 105 (4): 526–32.