Patients most likely to benefit from regional anesthesia are often treated with anticoagulants, which increases the risk of hemorrhagic complications. Importantly, anticoagulated patients are at an increased risk of developing vertebral canal hematoma (VCH), a complication of neuraxial anesthesia which may result in permanent neurological complications if not rapidly recognized and treated. Therefore, the decision-making strategy of patients at risk of bleeding is important when considering neuraxial or regional anesthesia techniques.
INTRODUCTION
Most organized societies of anesthesiologists, such as the American Society of Regional Anesthesia (ASRA), have published a set of recommendations or guidelines for the management of patients being treated with antiplatelet or anticoagulant medications who are planned to receive central neuraxial blocks (CNB). Recommendations by different organized societies may vary somewhat because no firm evidence exists for most recommendations. Regardless, the available guidelines recommend time intervals after stopping the treatment at which performing regional anesthesia technique may be safer. The recommendations also suggest time intervals at which the treatment with anticoagulants and/or antiplatelet agents can be restarted after the procedure or removal of an epidural catheter. Factors that may increase the patient’s risk of bleeding should also be considered, such as female gender, age (>65 years), history of early bruising or excessive (surgical) bleeding, spinal column abnormalities, and renal insufficiency. Furthermore, the risk of VCH in an anticoagulated patient should be weighed against the benefits of regional anesthesia.
ANTIPLATELET AGENTS
Table 1 summarizes the current ASRA guidelines on time intervals before and after neuraxial blocks for antiplatelet agents.
Table 1. Guidelines on time intervals before and after neuraxial blocks for antiplatelet agents (2021)*
| Antiplatelet agent | When neuraxial block can be performed after drug is stopped | Restarting the therapy with neuraxial catheter in situ | Restarting the therapy after neuraxial block/catheter removal |
|---|---|---|---|
| Aspirin | No additional precautions | No additional precautions | No additional precautions |
| NSAIDS | No additional precautions | No additional precautions | No additional precautions |
| Clopidogrel | 5-7 days | OK to maintain for 1-2 days providing no loading dose (start 24 h postoperative) | Immediately (loading dose: 6 h) |
| Prasugrel | 7-10 days | Not recommended | Immediately (loading dose: 6 h) |
| Ticlopidine | 10 days | OK to maintain for 1-2 days providing no loading dose (start 24 h after surgery) | Immediately (loading dose: 6 h) |
| Ticagrelor | 5-7 days | Not recommended | Immediately (loading dose: 6 h) |
| Cangrelor | 3 h | Not recommended | 8 h |
| Abciximab | 24-48 h | Contraindicated within 4 weeks of surgery | No specific guidance |
| Tirofiban | 4-8 h | Contraindicated within 4 weeks of surgery | No specific guidance |
| Eptifibatide | 4-8 h | Contraindicated within 4 weeks of surgery | No specific guidance |
| Dipyridamole | 24 h for extended-release formulation | Not recommended | 6 h |
| Cilostazol | 2 days | Not recommended | 6 h |
Aspirin and NSAIDS
Aspirin and NSAIDS inhibit cyclo-oxygenase (COX), which prevents the formation of the potent platelet aggregation of thromboxane-A2. They are indicated at low doses for primary and secondary prevention of stroke and myocardial infarction. Aspirin affects platelet function for the duration of platelet life; NSAID’s affect function only temporarily. ASRA guidelines recommend no additional precautions in patients treated with these medications before CNB performance.
P2Y12 receptor antagonists
Blocking the P2Y12 receptor inhibits adenosine-diphosphate-mediated platelet aggregation. P2Y12 receptor antagonists include the thienopyridines (clopidogrel, prasugrel, ticlopidine) and the non-thienopyridines (ticagrelor, cangrelor). ASRA guidelines recommend discontinuing all these drugs (excluding cangrelor) for 5-7 days before receiving a CNB (10 days for ticlopidine). Cangrelor should be stopped 3 h before the administration of a neuraxial block. A non-loading dose of clopidogrel, prasugrel, ticlopidine, or ticagrelor can be given immediately after catheter removal or block performance. With an indwelling neuraxial catheter, clopidogrel or ticlopidine can be given from 24 h postoperatively. If a loading dose is not given, the catheter should only be used for 1-2 days.
Platelet glycoprotein IIb/IIIa receptor antagonists (abciximab, tirofiban, eptifibatide)
Platelet glycoprotein IIb/IIIa receptor antagonists inhibit platelet aggregation via interference with platelet fibrinogen and platelet von Willebrand factor binding. The time intervals are based on the time to return to normal platelet aggregation. The intervals are longer for abciximab (24-48 h) than for eptifibatide and tirofiban (4-8 h).
Dipyridamole
Dipyridamole is used to prevent ischemic stroke. ASRA guidelines recommend discontinuing the extended-release formulation 24 h before CNB performance. Moreover, the agent should not be given with a neuraxial catheter in situ.
Cilostazol
Cilostazol inhibits phosphodiesterase IIIa and thus platelet aggregation. ASRA guidelines recommend discontinuation for 48 h before CNB performance.
ANTICOAGULANT AGENTS
Table 2 summarizes the current ASRA guidelines on time intervals before and after neuraxial blocks for anticoagulant agents.
Table 2. Guidelines on time intervals before and after neuraxial blocks for anticoagulant agents (2021)*
| Drug | When neuraxial block can be performed after drug is stopped | Restarting the therapy with neuraxial catheter in situ | Restarting the therapy after neuraxial block/catheter removal |
|---|---|---|---|
| Heparin and LMWH | |||
| UFH s.c. | If >4 days UFH: perform platelet count in addition to following guidance before CNB: - Low-dose prophylaxis (5,000 U b.d./t.d.s.): 4-6 h and after coagulation status assessed - Higher-dose prophylaxis (7,500-10,000 U b.d. or <20,000 U daily total): 12 h and after coagulation status assessed - Therapeutic dose (>10,000 U per dose; >20,000 U daily total): 24 h and after coagulation status assessed | If >days UFH: perform platelet count in addition to following guidance before catheter removal: - Low dose: Acceptable to give whilst catheter in situ; catheter removal 4-6 h after administration - Higher dose (doses >5,000 U or daily total >15,000): Analyze risk/benefit in that patient; if giving, institute neurological observation monitoring regimen | 1 h (low dose; no specific guidance on higher dose) |
| UFH i.v. | If >4 days UFH: perform platelet count in addition to the following guidance before CNB: 4-6 h and normal coagulation status | If >4 days UFH: perform platelet count in addition to the following guidance before catheter removal: 4-6 h after administration | 1 h |
| LMWH | If >4 days LMWH: perform platelet count in addition to the following guidance before CNB: - Prophylactic dose: 12 h - Treatment dose: 24 h and consider anti-factor Xa level | If >4 days LMWH: perform platelet count in addition to the following guidance before CNB: - Prophylactic o.d. dose: Catheters do not represent additional risk; first dose acceptable 24 h after catheter placement; remove catheter 12 h after last dose - Treatment dose: Not recommended | Prophylactic dose: 4 h Treatment dose: 24 h after non-high- bleeding-risk surgery/neuraxial block placement and 48-72 h after high-bleeding-risk surgery; catheters should be removed at least 24 h after needle/catheter placement, and first dose should be given at least 4 h after catheter removal |
| Parenteral heparin alternatives | |||
| Fondaparinux | Only where: single-needle pass, atraumatic needle placement, avoidance of indwelling neuraxial catheters | Avoid | 6 h |
| Argatroban | Avoid | N/A | N/A |
| Bivalirudin | Avoid | N/A | N/A |
| Oral anticoagulant drugs | |||
| Rivaroxaban | 72 h; if earlier, consider rivaroxaban or anti-factor Xa level (safe residual level for CNB is unknown) | Not recommended: with unanticipated administration, hold rivaroxaban dosing for 22-26 h or assess an anti-factor Xa assay calibrated to rivaroxaban before catheter removal | 6 h |
| Edoxaban | 72 h; if earlier, consider edoxaban or anti-factor Xa level (safe residual level for CNB is unknown) | Not recommended: with unanticipated administration, hold edoxaban dosing for 20-28 h or assess an anti-factor Xa assay calibrated to edoxaban before catheter removal | 6 h |
| Apixaban | 72 h; if earlier, consider apixaban or anti-factor Xa level (safe residual level for CNB is unknown) | Not recommended: with unanticipated administration, hold apixaban dosing for 26-30 h or assess an anti-factor Xa assay calibrated to apixaban before catheter removal | 6 h |
| Dabigatran | 120 h; if no additional risk factors for bleeding: - CrCl >80 mL/min: 72 h - CrCl 50-79 mL/min: 96 h - CrCl 30-49 mL/min: 120 h - CrCl 30 mL/min: avoid | Not recommended: with unanticipated administration, hold dabigatran dosing for 34-36 h or assess the dTT or ECT before catheter removal | 6 h |
| Warfarin | Ideally stop INR 5 days before and INR “normalized” | - Low-dose therapy: Check INR daily and routine sensory and motor neurological testing - INR 1.5-2.9: Catheter acceptable with caution - INR ≥3.0: Hold warfarin | After catheter removal, suggest continuing neurological observations for 24 h |
| Thrombolytic drugs | |||
| Thrombolytic drugs (e.g., alteplase and streptokinase) | 48 h and documented normal clotting (including fibrinogen) | Not recommended; if unexpectedly given, measure fibrinogen to guide timing of catheter removal | No recommendation, but note that original contraindications to these drugs state should not be given for 10 days after puncture of non-compressible vessels |
APTTR, activated partial thromboplastin time ratio; CNB, central neuraxial block; CrCl, creatinine clearance; dTT, dilute thrombin time; ECT, ecarin clotting time; INR, international normalized ratio; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin.
Heparin and low-molecular-weight heparins (LMWH)
Unfractionated heparin (UFH)
UFH binds to antithrombin, leading to the inactivation of thrombin (factor IIa), factor Xa, and factor IXa. Intravenous (i.v.) UFH acts immediately while subcutaneously (s.c.) administered 5,000 I.U. exerts its effects after 1 h. The ASRA guidelines recommended time intervals are dependent on the route of administration and for s.c. UFH on the dose. Time intervals before CNB for s.c. UFH can be up to 24 h after the last dose. Furthermore, patients receiving UFH >4 days should have a platelet count before CNB or catheter removal to exclude heparin-induced thrombocytopenia.
LMWH
LMWHs inhibit factor Xa and are indicated for venous thromboembolism prophylaxis and treatment. Guidelines by ASRA recommend against routine testing of anti-factor Xa levels since there is no known safe level for performing CNBs. A 12 h time interval should be considered after neuraxial puncture until the first prophylactic dose and a 24 h time interval for therapeutic LMWH. Maintain catheters if the patient receives a prophylactic dose daily. The catheter should be removed 12 h after the last daily prophylactic dose.
Parenteral heparin alternatives
Factor Xa inhibitors (fondaparinux)
A CNB is only appropriate in the following circumstances for a patient treated with fondaparinux: single-needle pass, atraumatic procedure, and no neuraxial catheter.
Direct thrombin inhibitors (argatroban, bivalirudin)
Direct thrombin inhibitors’ effects are monitored via activated partial thromboplastin time (APTT) and last for 3 h after i.v. administration. Neuraxial techniques are not recommended in patients taking argatroban or bivalirudin.
Direct oral anticoagulants
Oral factor Xa inhibitors (rivaroxaban, edoxaban, apixaban)
For rivaroxaban, the time intervals depend on the dose and the patient’s renal function. Edoxaban and apixaban have similar time intervals as rivaroxaban (i.e., 72 h).
Oral thrombin inhibitors (dabigatran)
Dabigatran is indicated for the prevention and treatment of venous thromboembolism and to lower the risk of a stroke. The time intervals largely depend on the patient’s renal function as >80% is excreted by the kidneys. ASRA guidelines recommend a time interval of 120 h after the last dose before neuraxial puncture in the absence of renal function measurement. A graduated approach based on creatinine clearance should be followed if there are no additional risk factors and a renal function measurement is available. ASRA guidelines advise against administering dabigatran when a neuraxial catheter is in situ. Moreover, the catheter must be removed 6 h before administering the agent again.
Warfarin
Warfarin inhibits the vitamin-K-dependent clotting factors II, VII, IX, and X synthesis. ASRA guidelines recommend a normal international normalized ratio (INR; i.e., ≤1.1). Administration of the drug with a neuraxial catheter in place is acceptable with caution (e.g., neurological observations of sensory and motor function) when the INR is 1.5-3.0. Catheters can be removed with an INR <1.5 and continued neurological observations for 24 h.
Warfarin can be reversed with vitamin K in the absence of major bleeding, an i.v. infusion acts within 6-8 h. Prothrombin complex concentrate (Octaplex and Beriplex) can also be used.
Thrombolytic/fibrinolytic agents (alteplase, streptokinase)
Thrombolytic/fibrinolytic agents interact with plasminogen to produce plasmin that lyses links between fibrin molecules to dissolve clots. These drugs are used in acute myocardial infarction, pulmonary embolism, and cerebrovascular accidents. A neuraxial puncture should only be considered 48 h after administration of these agents in patients where clotting studies (including fibrinogen count) are normal. In addition, patients should be neurologically monitored, ideally every 2 h.
HOW TO USE THE GUIDELINES IN PERIPHERAL NERVE BLOCKS?
Even less objective information is available regarding the frequency and outcome of hemorrhagic complications after peripheral nerve blocks (PNBs).
The ASRA guidelines of 2021 include a summary of 32 case reports of patients having severe hemorrhagic complications after PNBs and observed the following trends:
- Patients suffering from neurological deficits all completely recovered within 12 months.
- Patients requiring hospitalization after developing complications had a prolonged stay.
- Complications in anticoagulated patients resulted more from blood loss than from neurological damage.
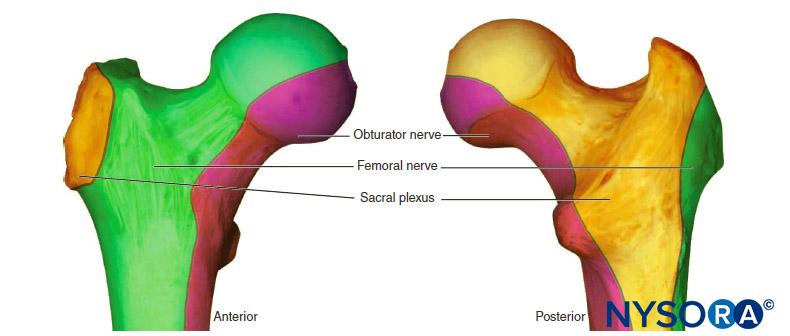
- Deep plexus (e.g., lumbar plexus block) and deep peripheral blocks (e.g., proximal sciatic nerve block) carried a higher risk.
- There was often no evidence of vessel trauma.
In conclusion, anticoagulated patients receiving perineuraxial, deep plexus, or deep peripheral nerve blocks should be managed as if they are undergoing neuraxial anesthesia. Clinical discretion should be used for decision-making regarding the safety of other regional anesthesia techniques, such as superficial plexus blocks and nerve blocks. As an example, the vascularity and compressibility of the anatomical site where the blocks are being performed and the potential consequences of bleeding at those sites should be kept in mind. The risks of discontinuing anticoagulation therapy in these patients should be weighed versus the benefits of neuraxial and nerve block anesthesia and analgesia.
READ MORE about Anticoagulants at this link on NYSORA: Neuraxial Anesthesia and Peripheral Nerve Blocks in Patients on Anticoagulants
ADDITIONAL READING
- Ashken T, West S. Regional anesthesia in patients at risk of bleeding. BJA Educ 2021; 21:84-94.
- Smith LM, Cozowicz C, Uda Y, Memtsoudis SG, Barrington MJ. Neuraxial and combined neuraxial/general anesthesia compared to general anesthesia for major truncal and lower limb surgery. Anesth Analg 2017; 125:1931-45.
- Johnson RL, Kopp SL, Burkle CM et al. Neuraxial vs general anaesthesia for total hip and total knee arthroplasty: a systematic review of comparative-effectiveness research. Br J Anaesth 2016; 116: 163-76.
- Neal JM, Barrington MJ, Brull R et al. The second ASRA practice advisory on neurologic complications associated with regional anesthesia and pain medicine. Reg Anesth Pain Med 2015; 40: 401-30.
- Maier C, Gleim M, Weiss T, Stachetzki U, Nicolas V, Zenz M. Severe bleeding following lumbar sympathetic block in two patients under medication with irreversible platelet aggregation inhibitors. Anesthesiology 2002; 97: 740-3.
- Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blocks in Sweden 1990-1999. Anesthesiology 2004; 101: 950-9.
- Royal College of Anaesthetists. NAP 3 complications of neuraxial block. 2009. Available from: https://www.nationalauditprojects.org.uk/NAP3_home. [Accessed 7 January 2021].
- Pitkanen MT, Aromaa U, Cozanitis DA, Forster JG. Serious complications associated with spinal and epidural anaesthesia in Finland from 2000 to 2009. Acta Anaesthesiol Scand 2013; 57: 553-64.
- Ruppen W, Derry S, McQuay H, Moore RA. Incidence of epidural hematoma, infection, and neurologic injury in obstetric patients with epidural analgesia/anesthesia. Anesthesiology 2006; 105: 394-9.
- Filipovic M. New antiplatelet drugs and new oral anticoagulants. Br J Anaesth 2016; 117: 74-84.
- Mcilmoyle K, Tran H. Perioperative management of oral anticoagulation. BJA Educ 2018; 18: 259-64.
- Harrop-Griffiths W, Cook T, Gill H et al. Regional anaesthesia and patients with abnormalities of coagulation. Anaesthesia 2013; 68: 966-72.
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy. Reg Anesth Pain Med 2018; 43: 263-309.
- Gogarten W, Vandermeulen E, Van Aken H, Kozek S, Llau JV, Samama CM. Regional anaesthesia and antithrombotic agents: recommendations of the European Society of Anaesthesiology. Eur J Anaesthesiol 2010; 27: 999-1015.
- Breivik H, Bang U, Jalonen J, Vigfusson G, Alahuhta S, Lagerkranser M. Nordic guidelines for neuraxial blocks in disturbed haemostasis from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand 2010; 54: 16-41.
- 15. Ramalingam G, Jones N, Besser M. Platelets for anaesthetists part 2: pharmacology. BJA Educ 2016; 16: 140-5.
- Keeling D, Baglin T, Tait C et al. Guidelines on oral anticoagulation with warfarin fourth edition. Br J Haematol 2011; 154: 311-24.
- Joubert F, Gillois P, Bouaziz H, Marret E, Iohom G, Albaladejo P. Bleeding complications following peripheral regional anaesthesia in patients treated with anticoagulants or antiplatelet agents: a systematic review. Anaesth Crit Care Pain Med 2019; 38: 507-16.
- Tsui BCH, Kirkham K, Kwofie MK et al. Practice advisory on the bleeding risks for peripheral nerve and interfascial plane block: evidence review and expert consensus. Can J Anaesth 2019; 66: 1356-84.