Ultrasound-guided superficial cervical plexus blocks for post-craniotomy pain
Persistent incisional pain is a common and debilitating complication following suboccipital craniotomies, affecting recovery and quality of life. Current pain management strategies, including systemic opioids and local infiltration, have shown limited efficacy. This study evaluated the efficacy of ultrasound-guided superficial cervical plexus blocks (SCPBs) with ropivacaine in reducing persistent pain three months after craniotomy.
Study objective and methods
The primary goal of this randomized, double-blind, placebo-controlled trial was to assess whether preoperative SCPBs with ropivacaine reduce persistent incisional pain three months post-surgery.
- Participants: 292 adults undergoing suboccipital craniotomy for benign conditions.
- Intervention: Patients were randomly assigned to receive either 10 mL of 0.5% ropivacaine or an equivalent volume of saline under ultrasound guidance.
- Primary outcome: Incidence of persistent pain three months post-surgery.
- Secondary outcomes: Acute postoperative pain, neuropathic pain, sleep quality, and patient satisfaction.
Key findings
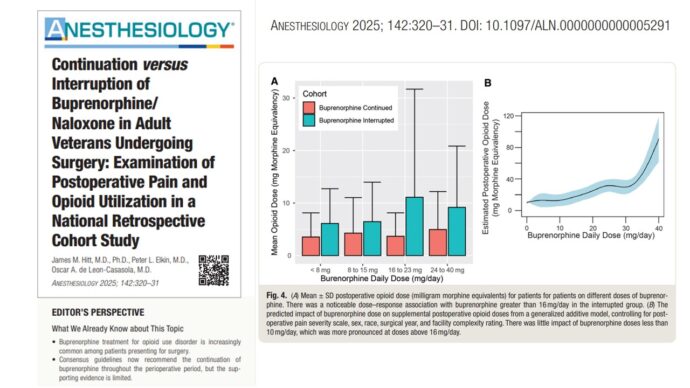
- Primary outcome: Persistent pain was significantly lower in the ropivacaine group (34%) compared to the saline group (51%), with a relative risk reduction of 34% (p = 0.003).
- Pain severity: Mild pain was reported in 29% of the ropivacaine group versus 42% in the saline group. Moderate-to-severe pain occurred in 5% of the ropivacaine group compared to 9% in the saline group.
- Acute pain: Ropivacaine patients reported lower median pain scores at 24 and 48 hours post-surgery, though differences were modest.
Other outcomes: Sleep quality and patient satisfaction were similar between groups. No significant adverse events were associated with the block.
Conclusion
SCPBs with ropivacaine significantly reduced the incidence of persistent pain three months after suboccipital craniotomies, with a number needed to treat of 5.8 patients to prevent one case of persistent pain. While acute pain relief was modest, the long-term benefits highlight the potential of SCPBs as an effective preemptive analgesia strategy in neurosurgical settings.
Future research
Future studies should explore the long-term benefits of SCPBs beyond three months and assess their effectiveness in broader neurosurgical populations. Investigating optimized dosages and combining SCPBs with other analgesic techniques may further improve outcomes and refine best practices.
For more detailed information, refer to the full article in Anesthesiology.
Zeng M, Zheng M, Ren Y, et al. Ultrasound-guided Superficial Cervical Plexus Blocks for Persistent Pain after Suboccipital Craniotomies: A Randomized Trial. Anesthesiology. 2025;142(1):166-175.
Download the Nerve Blocks App HERE for in-depth insights on the cervical plexus block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Blocks Manual Course on NYSORA’s LMS!