Thomas F. Bendtsen, Sherif Abbas, and Vincent Chan
FACTS
- Indications: carotid endarterectomy, superficial neck surgery (Figure 1)
- Transducer position: transverse over the midpoint of the sternocleidomastoid muscle (posterior border)
- Goal: local anesthetic spread around the superficial cervical plexus or deep to the sternocleidomastoid muscle
- Local anesthetic: 5–15 mL
GENERAL CONSIDERATIONS
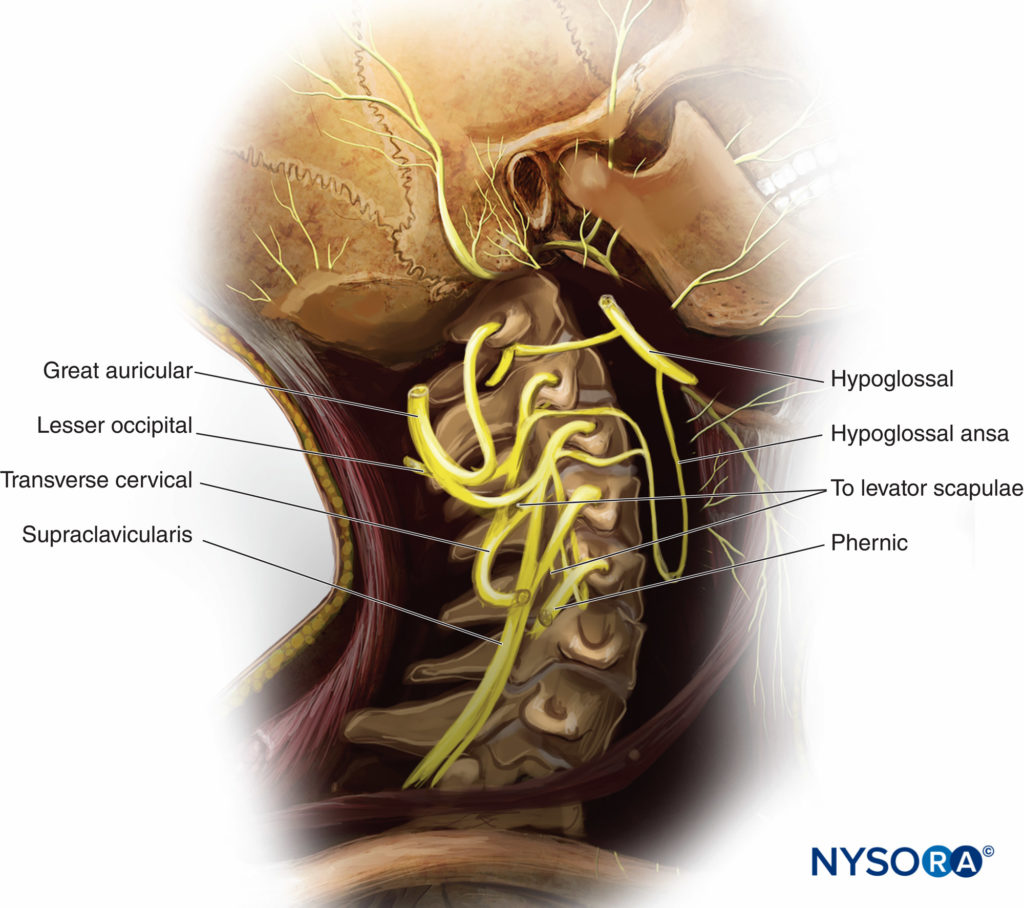
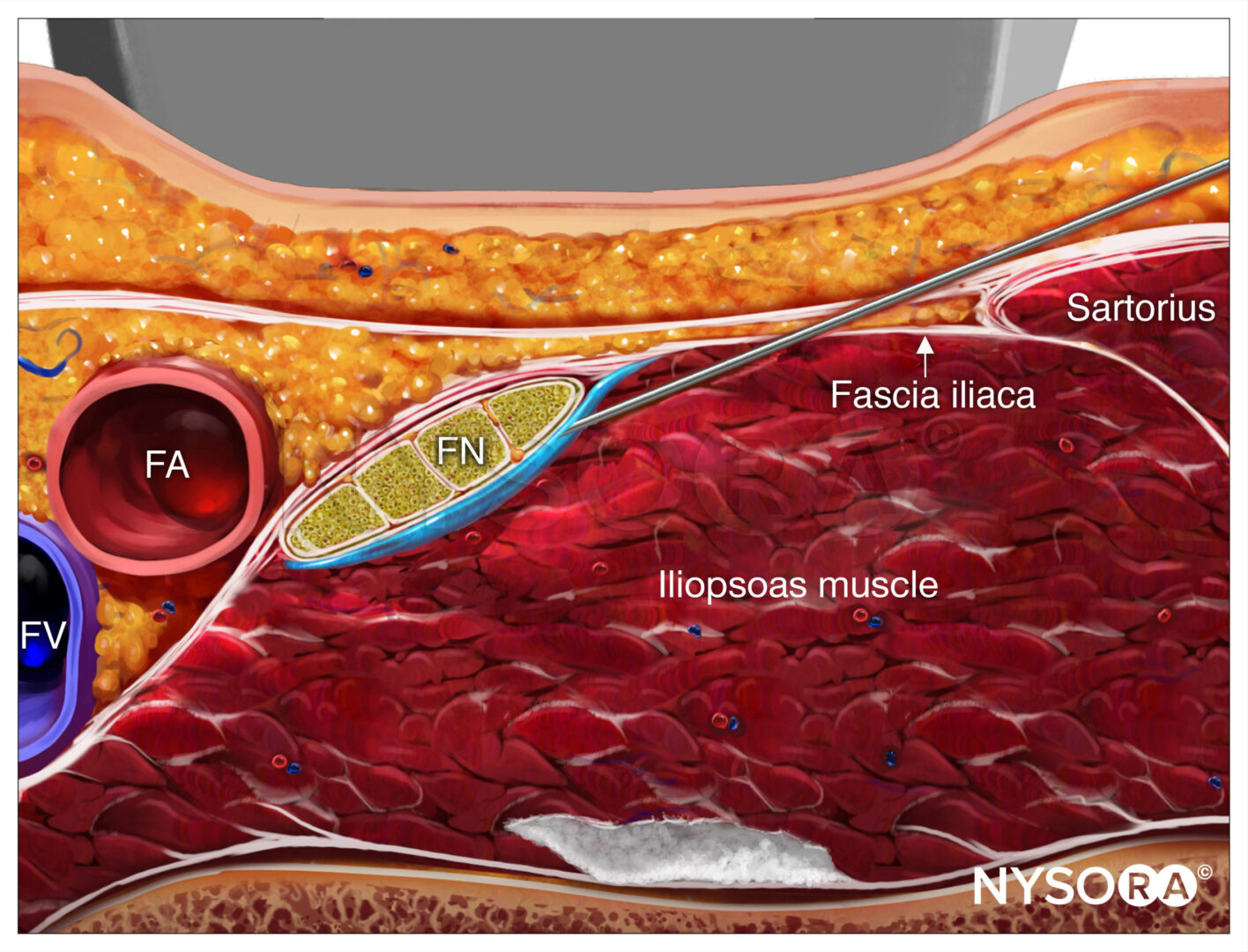
The goal of the ultrasound (US)-guided technique of superficial cervical plexus nerve block is to deposit local anesthetic within the vicinity of the sensory branches of the nerve roots C2, C3, and C4 (Figures 2 and 3). Advantages over the landmark-based technique include the ability to visualize the spread of local anesthetic in the correct plane, which therefore increases the success rate, and to avoid a needle insertion that is too deep and the inadvertent puncture of neighboring structures.
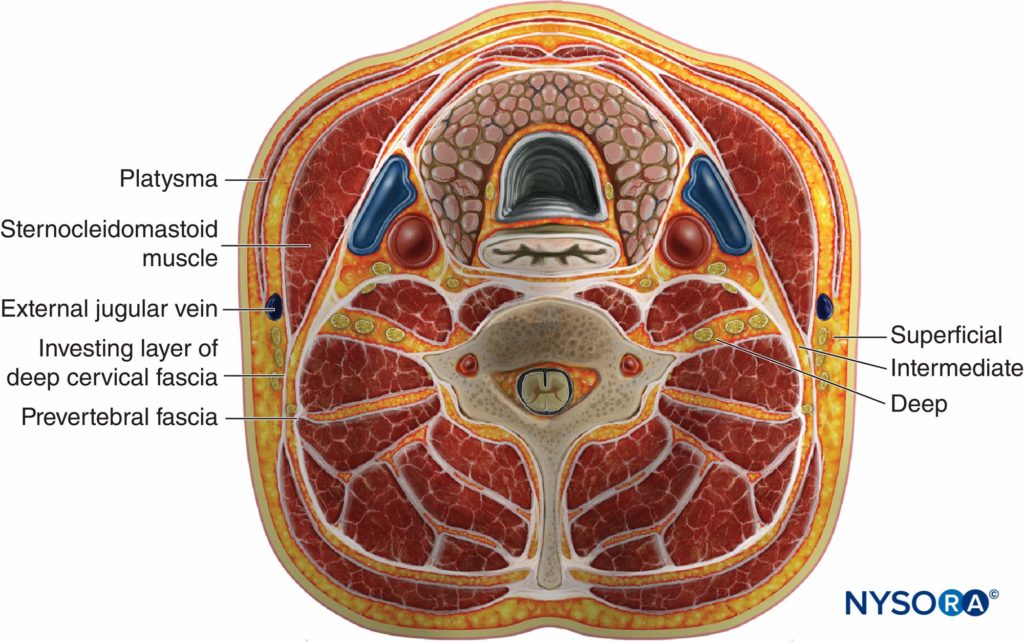
Figure 2. Site of injection of local anesthetic for superficial, intermediate, and deep cervical plexus nerve blocks.
Both US-guided superficial and deep cervical plexus nerve blocks have been well described. The deep cervical plexus nerve block is an advanced nerve block with a risk of potentially serious complications, such as intrathecal injection or injection into the vertebral artery. For this reason, we will focus primarily on the superficial cervical plexus nerve block technique. It is simpler, safer, and, for most indications, it is equally as suitable as the deep cervical plexus nerve block. An understanding of the fascial planes of the neck and the location of each of these nerve blocks is necessary (Figure 2). For the superficial cervical plexus nerve block, local anesthetic is injected superficially to the deep cervical fascia. For the superficial (intermediate) cervical plexus nerve block, the injection is made between the investing layer of the deep cervical fascia and the prevertebral fascia, whereas for the deep cervical plexus nerve block, local anesthetic is deposited deep to the prevertebral fascia.
ULTRASOUND ANATOMY
The sternocleidomastoid muscle (SCM) forms a “roof” over the nerves of the superficial cervical plexus (C2–4) (see Figure 2). The roots combine to form the four terminal branches (the lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves) and emerge from behind the posterior border of the SCM (Figures 3, 4 and 5). The plexus can be visualized as a small collection of hypoechoic nodules (honeycomb appearance or hypoechoic [dark] oval structures) immediately deep or lateral to the posterior border of the SCM (see Figure 5), but this is not always apparent.
Occasionally, the greater auricular nerve is visualized on the superficial surface of the SCM as a small, round, hypoechoic structure. The SCM is separated from the brachial plexus and the scalene muscles by the prevertebral fascia, which can be seen as a hyperechoic linear structure. The cervical plexus lies posterior to the SCM and immediately superficial to the prevertebral fascia overlying the interscalene groove (see Figure 5). Strictly speaking, the technique we describe, with an injection between the investing layer of the deep cervical fascia and the prevertebral fascia, is thus an intermediate cervical plexus nerve block.
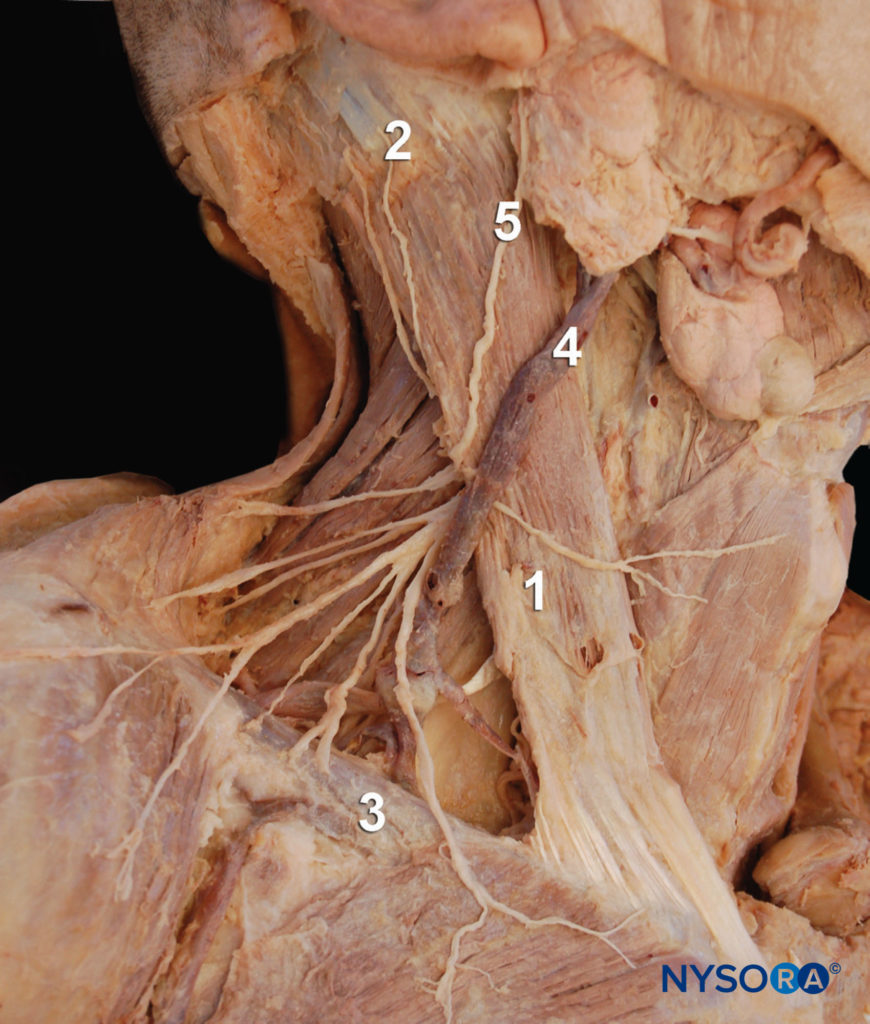
Figure 4. Anatomy of the cervical plexus. The cervical plexus is seen emerging behind the posterior border of the sternocleidomastoid muscle at the intersection of the muscle with the external jugular vein. 1: Sternocleidomastoid muscle. 2: Mastoid process. 3: Clavicle. 4: External jugular vein. 5: Greater auricular nerve. Supraclavicular nerves are seen rossing the clavicle.
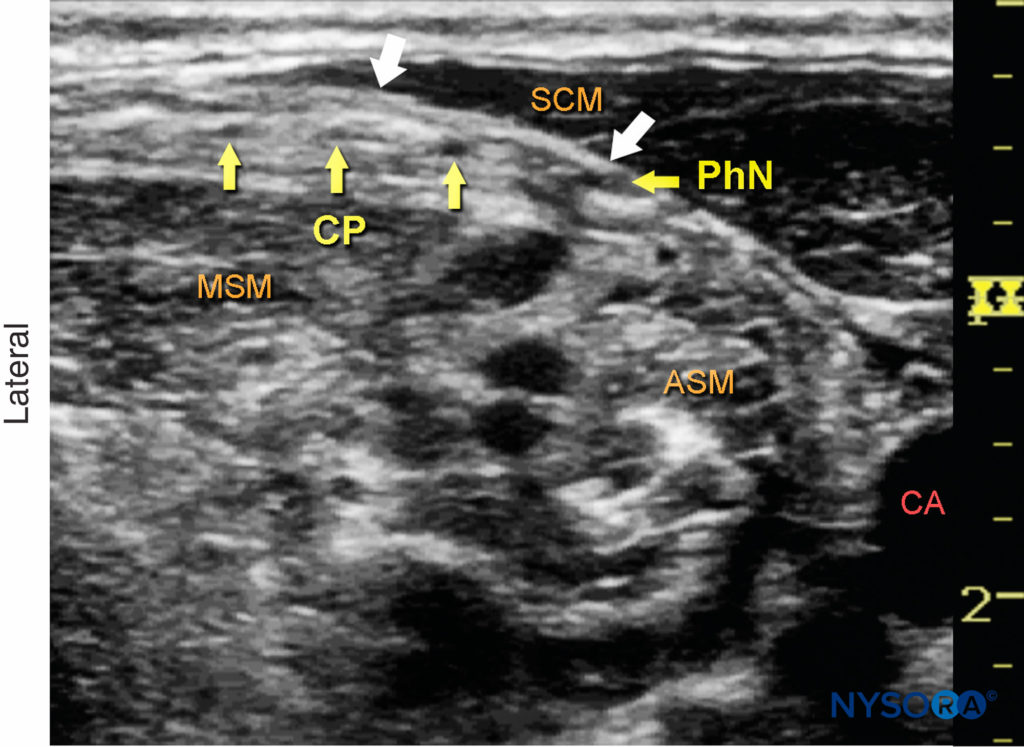
Figure 5. Cervical plexus (transverse view). Branches of the cervical plexus (CP) are seen superficial to the prevertebral fascia, which covers the middle (MSM) and anterior (ASM) scalene muscles, and posterior to the sternocleidomastoid muscle (SCM). White arrows, investing fascia of deep cervical fascia; CA, carotid artery; PhN, phrenic nerve.
DISTRIBUTION OF ANESTHESIA
From the Compendium of Regional Anesthesia: Cognitive priming for a cervical plexus block.
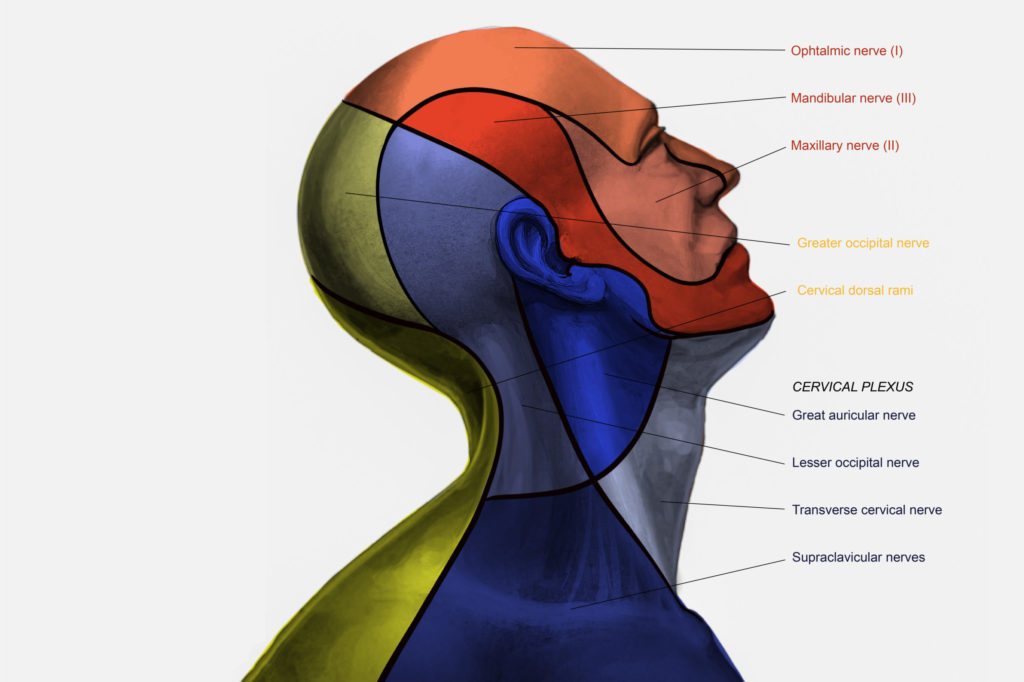
The superficial cervical plexus nerve block results in anesthesia of the skin of the anterolateral neck and the ante-auricular and retro-auricular areas, as well as the skin overlying and immediately inferior to the clavicle on the chest wall Figures 1 and 6). The mental, infraorbital, and supraorbital nerves are branches of the trigeminal nerve and are not blocked with cervical plexus nerve block.
The equipment needed for a cervical plexus nerve block includes the following:
• Ultrasound machine with a linear transducer (8–18 MHz), sterile sleeve, and gel
• Standard nerve block tray
• A 10-mL syringe containing local anesthetic
• A 5 cm, 23- to 25-gauge needle attached to low-volume extension tubing
• Sterile gloves
Learn more about Equipment for Regional Anesthesia.
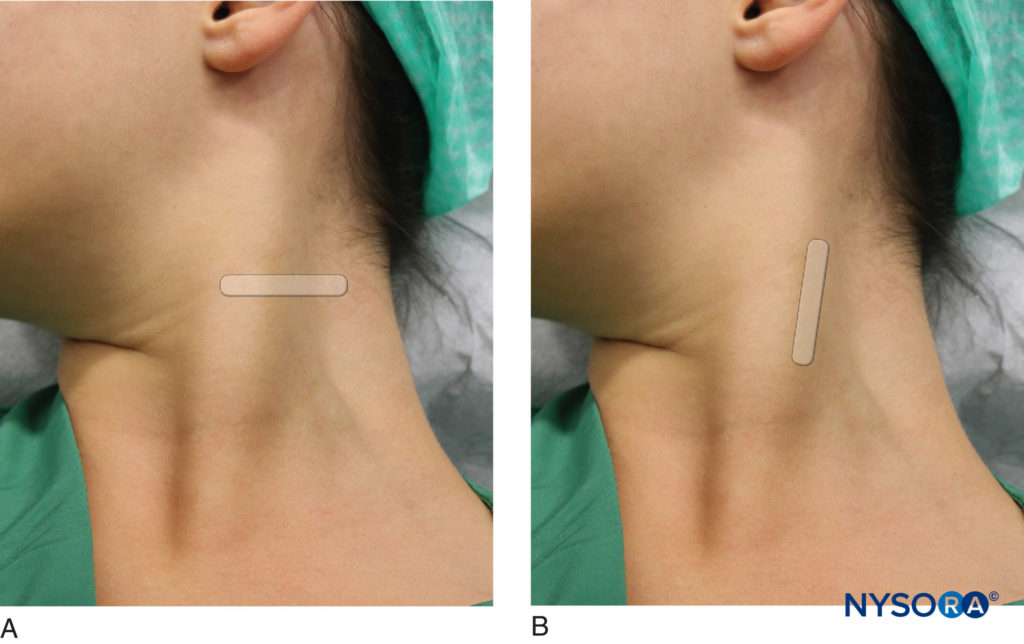
LANDMARKS AND PATIENT POSITIONING
Any patient position that allows for comfortable placement of the ultrasound transducer and needle advancement is appropriate. This nerve block is typically performed in the supine or semi-sitting position, with the head turned slightly away from the side to be blocked to facilitate operator access (Figure 7). The patient’s neck and upper chest should be exposed so that the relative length and position of the SCM can be assessed. The posterior border of the SCM can be difficult to locate, especially in obese patients. Asking the patient to lift his or her head off the bed can facilitate palpation of the posterior border of the SCM.
GOAL
The goal of this nerve block is to place the needle tip in the fascial layer underneath the SCM adjacent to the cervical plexus, which is contained within the tissue space between the Cervical fascia and posterior sheath of the SCM. If the elements of the cervical plexus are not easily visualized, the local anesthetic can be deposited in the plane immediately deep to the SCM and superficial investing layer of deep cervical fascia and superficial to the prevertebral fascia. A volume of 5-10 mL of local anesthetic usually suffices.
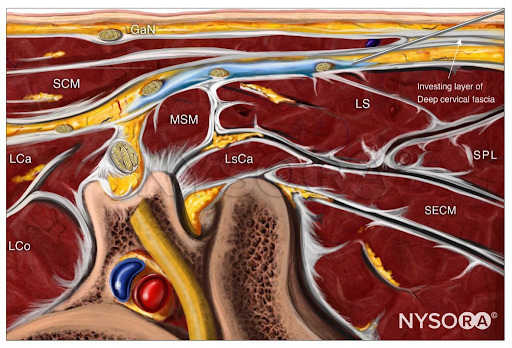
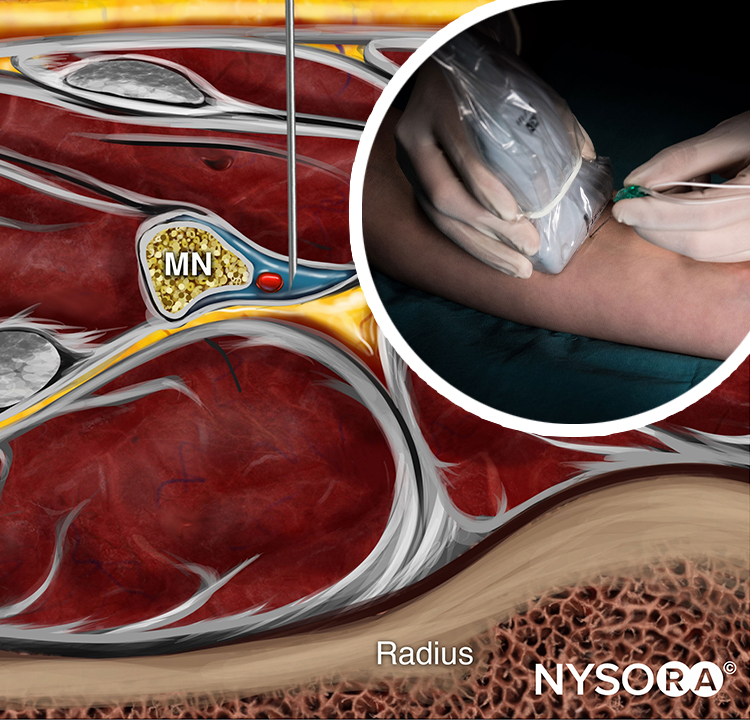
From the Compendium of Regional Anesthesia: Reverse Ultrasound Anatomy for a cervical plexus block with needle insertion in-plane and local anesthetic spread (blue). GaN, greater auricular nerve; SCM, sternocleidomastoid muscle; LCa, longus capitis muscle; LCo, longus Colli muscle; MSM, middle scalene muscle; LsCa, longissimus capitis muscle; LS, levator scapulae muscle; SPL, splenius capitis muscle; SECM, semispinalis capitis muscle.
TECHNIQUE
With the patient in the proper position, the skin is disinfected and the transducer is placed on the lateral neck, overlying the SCM at the level of its midpoint (approximately the level of the cricoid cartilage).
Once the SCM has been identified, the transducer is moved posteriorly until the tapering posterior edge is positioned in the middle of the screen. At this point, an attempt should be made to identify the brachial plexus and/or the interscalene groove between the anterior and middle scalene muscles. The cervical plexus is visible as a small collection of hypoechoic nodules (honeycomb appearance) immediately superficial to the prevertebral fascia that overlies the interscalene groove (see Figure 2 and 5).
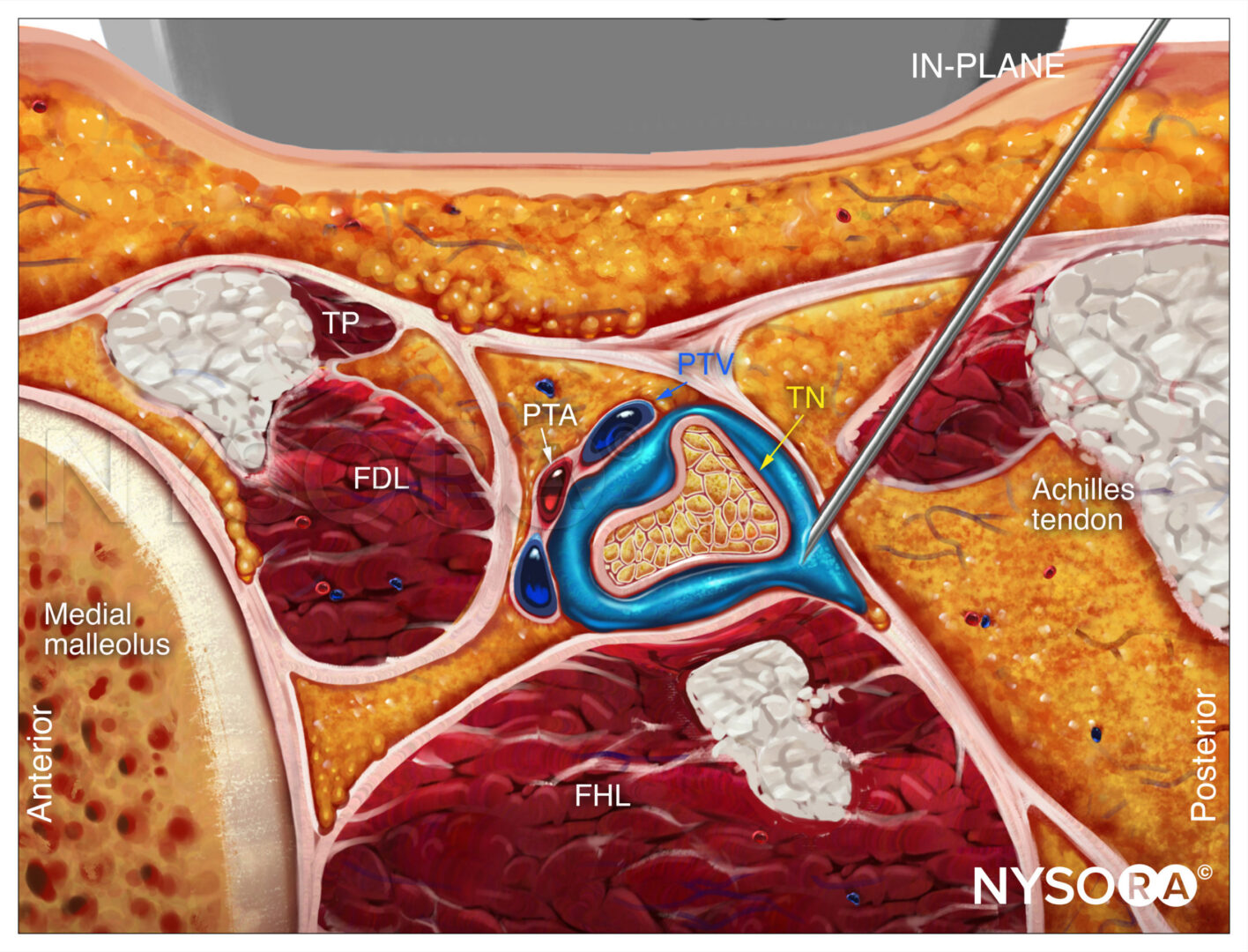
Once the plexus has been identified, the needle is passed through the skin, platysma, and investing layer of the deep cervical fascia, and the tip is placed adjacent to the plexus (Figure 8). Because of the relatively shallow position of the target, both in-plane (from the medial or lateral sides) and out-of-plane approaches may be used. Following negative aspiration, 1–2 mL of local anesthetic is injected to confirm the proper injection site. The remainder of the local anesthetic (5–15 mL) is administered to envelop the plexus (Figure 9).
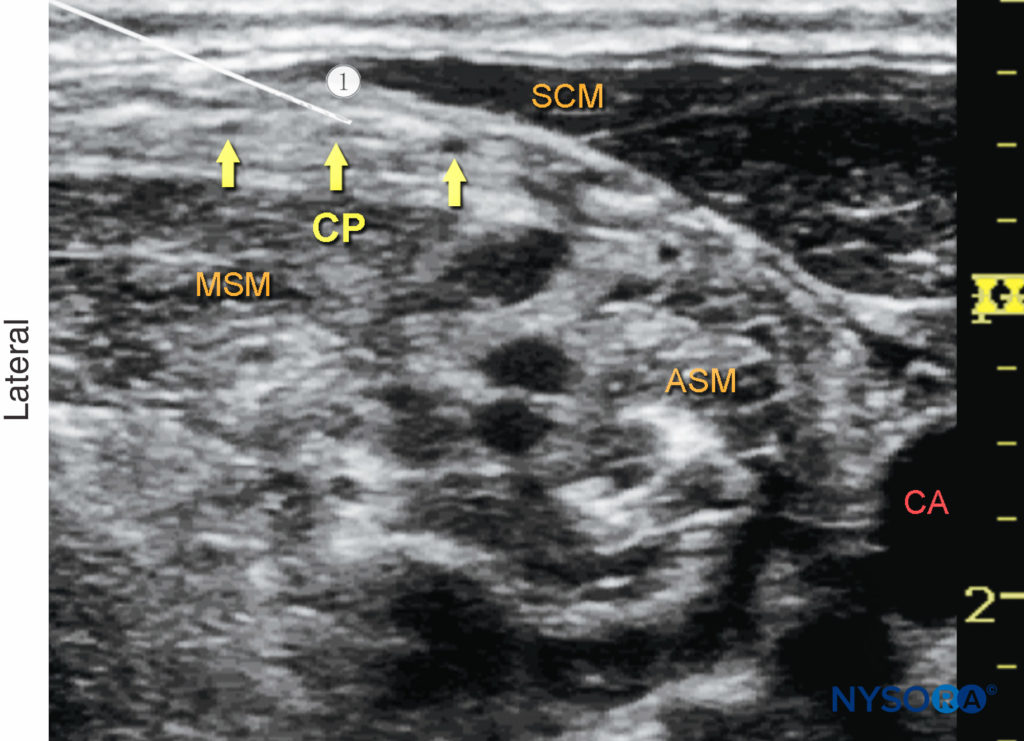
Figure 8. Superficial cervical plexus (transverse view): needle path (1) and position to nerve block the cervical plexus (CP).The needle is seen positioned underneath the lateral border of the sternocleidomastoid muscle (SCM) and superficial to the prevertebral fascia with the transducer in a transverse position (see Figure 7a). ASM, anterior scalene muscle; CA, carotid artery; MSM, middle scalene muscle.
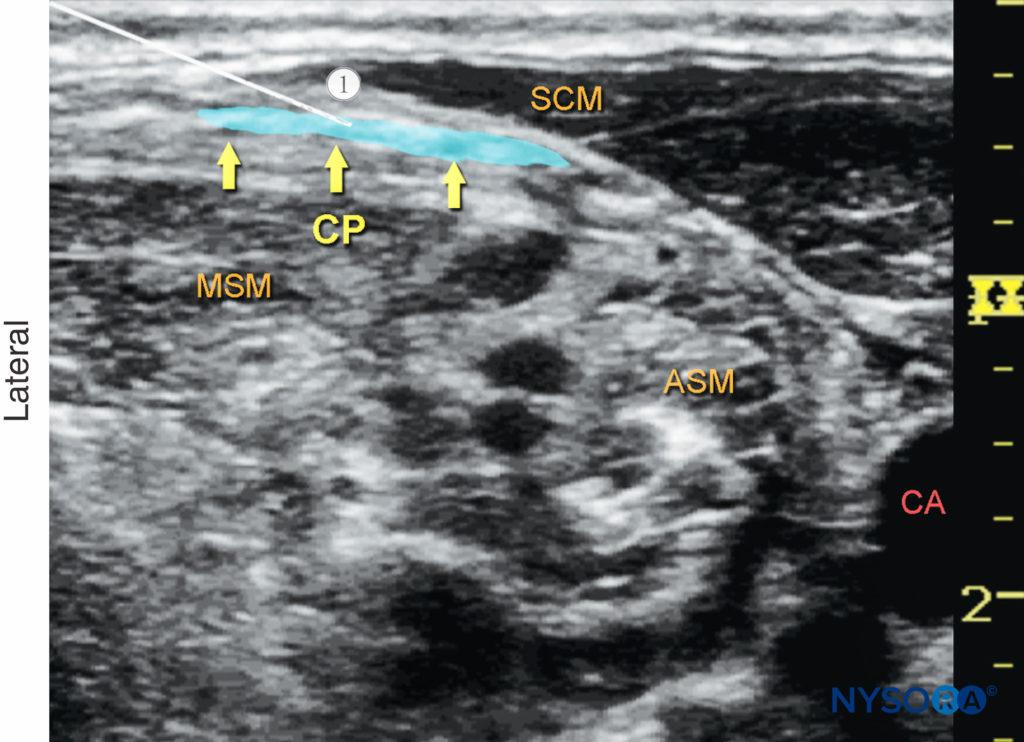
Figure 9. Cervical plexus (transverse view): desired distribution of local anesthetic (blue-shaded area) to nerve block the cervical plexus. Needle path: 1. ASM, anterior scalene muscle; CA, carotid artery; CP, cervical plexus; MSM, middle scalene muscle; SCM, sternocleidomastoid muscle.
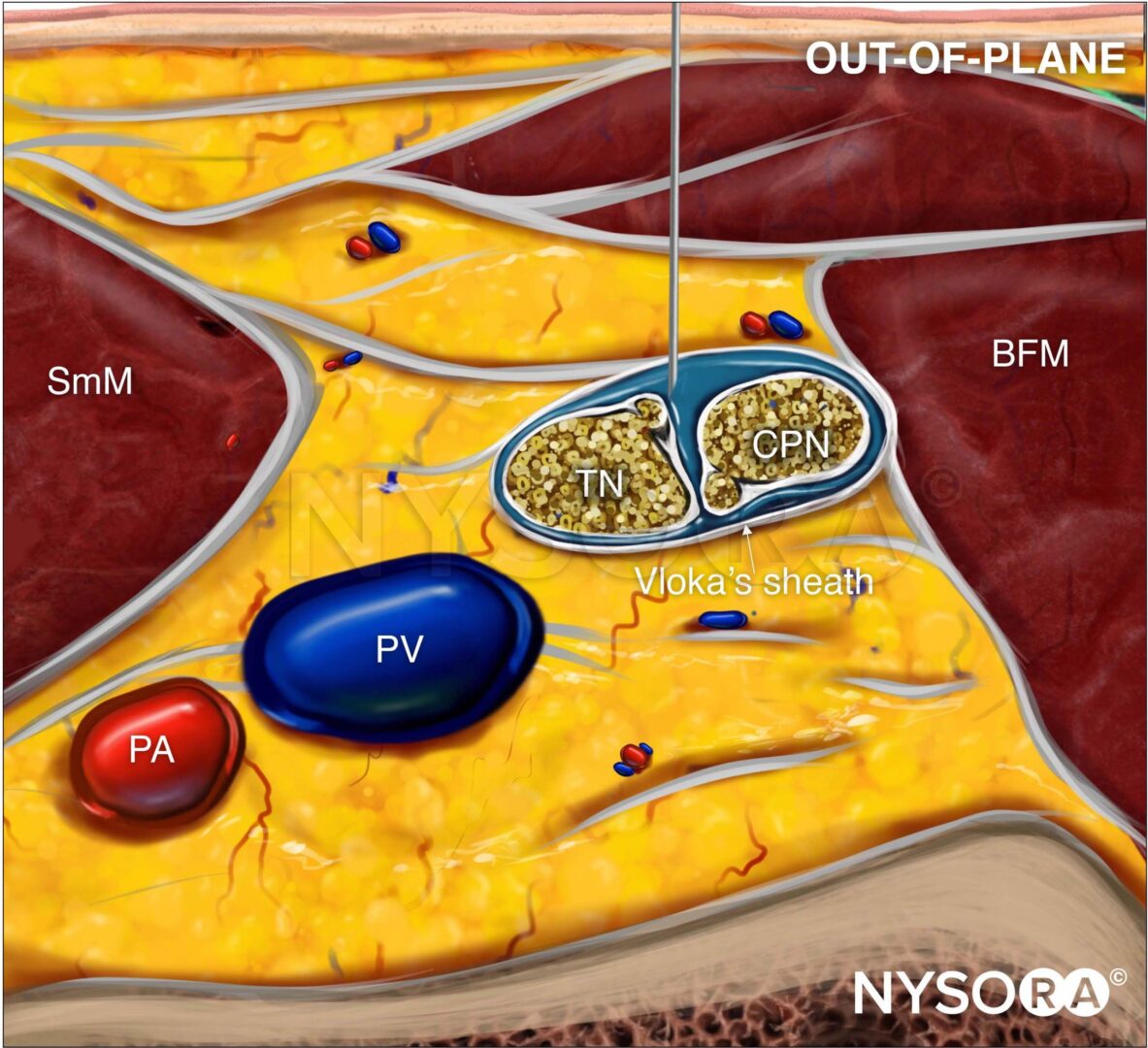
If the plexus is not visualized, an alternative sub sternocleidomastoid approach may be used. In this case, the needle is passed behind the SCM, and the tip is directed to lie in the space between the SCM and the prevertebral fascia, close to the posterior border of the SCM (Figures 7b, 10 and 11). Local anesthetic (5–15 mL) is administered and should be visualized layering out between the SCM and the underlying prevertebral fascia (Figure 12). If the injection of local anesthetic does not appear to result in an appropriate spread, needle repositioning and further injections may be necessary. Because the cervical plexus is made up of purely sensory nerves, high concentrations of local anesthetic are usually not required; ropivacaine 0.25–0.5%, bupivacaine 0.25%, or lidocaine 1% is a sufficient
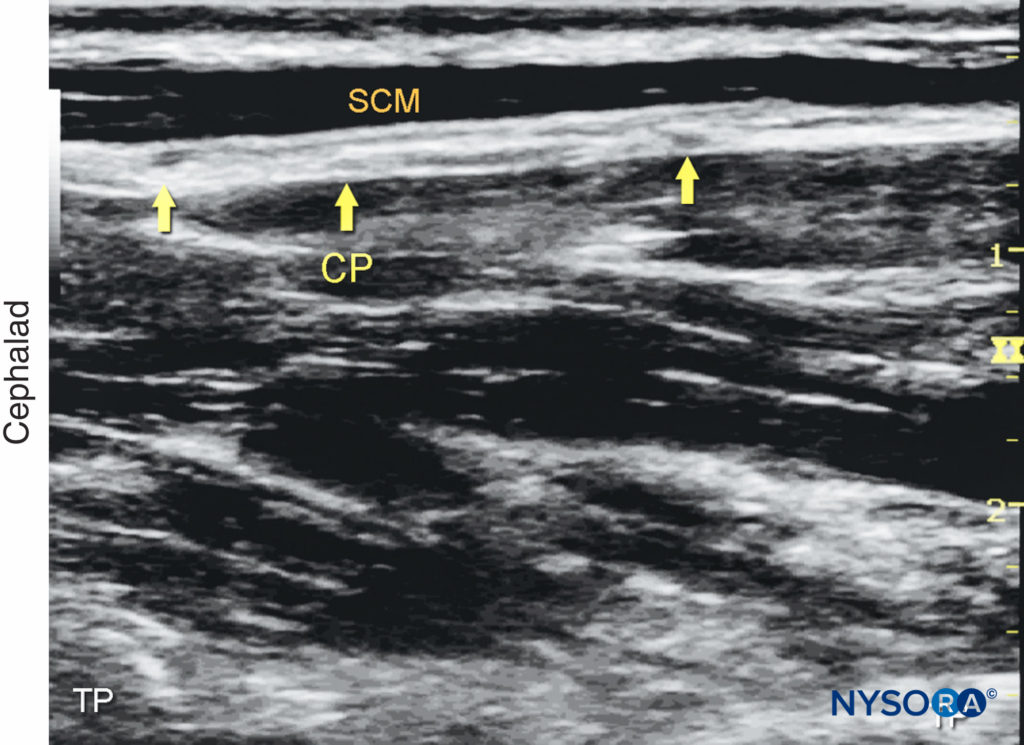
Figure 10. Cervical plexus (longitudinal view): Elements of the cervical plexus (CP) underneath the lateral border of the sternocleidomastoid muscle (SCM).
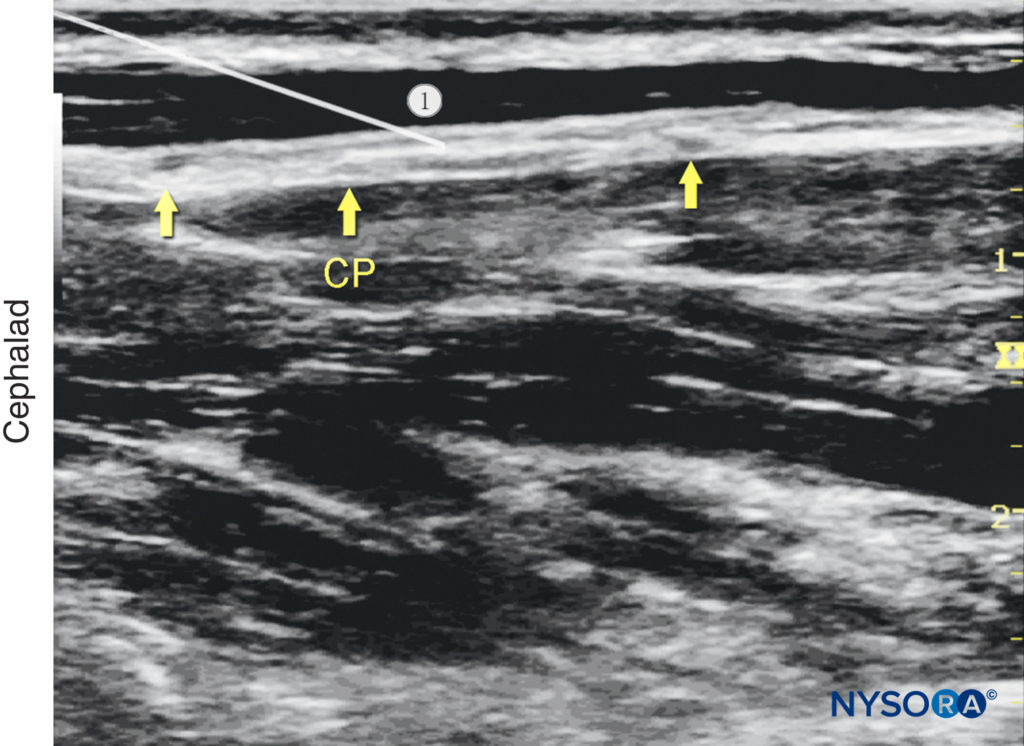
Figure 11. Cervical plexus (longitudinal view): needle position to nerve block the cervical plexus (CP).
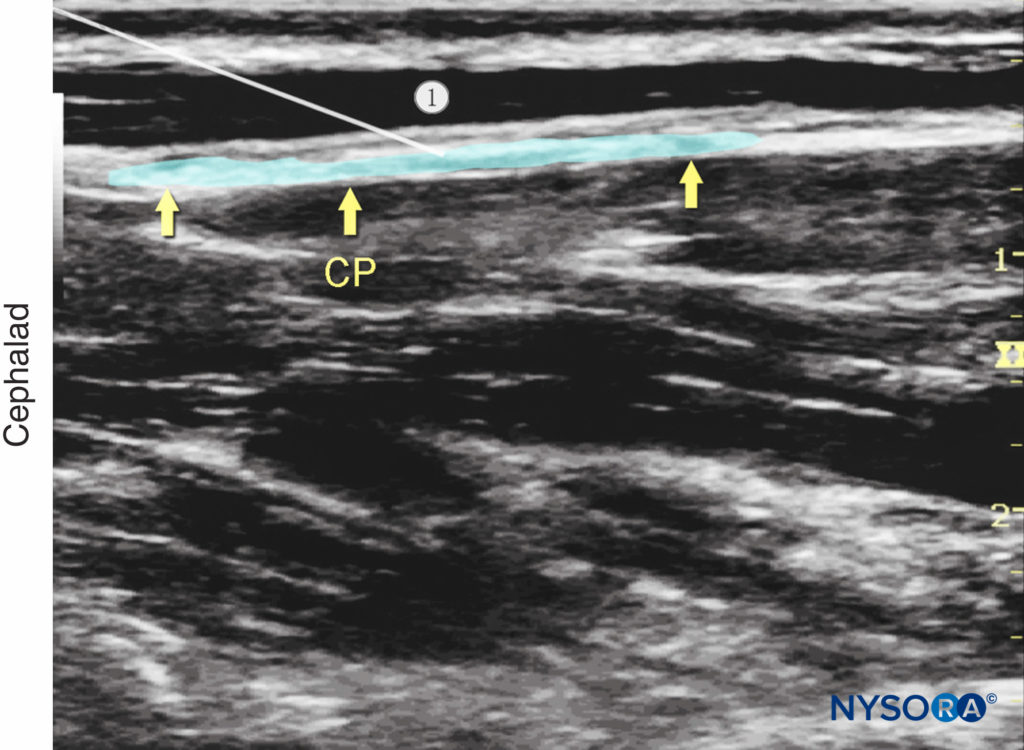
Figure 12. Cervical plexus (longitudinal view): desired spread of local anesthetic under the deep cervical fascia to nerve block the cervical plexus (CP).
TIPS
Visualization of the plexus is not necessary to perform this nerve block because the plexus may not always be readily apparent. Administration of 10 mL of local anesthetic deep to the SCM provides a reliable nerve block without the position of the plexus needing to be confirmed.
REFERENCES
- Aunac S, Carlier M, Singelyn F, De Kock M: The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg 2002;95:746–750.
- Christ S, Kaviani R, Rindfleisch F, Friederich P: Brief report: identification of the great auricular nerve by ultrasound imaging and transcutaneous nerve stimulation. Anesth Analg 2012;114:1128–1130.
- Demondion X, Herbinet P, Boutry N, et al: Sonographic mapping of the normal brachial plexus. Am J Neuroradiol 2003;24:1303–1309.
- Eti Z, Irmak P, Gulluoglu BM, Manukyan MN, Gogus FY: Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg 2006;102:1174–1176.
- Flaherty J, Horn JL, Derby R: Regional anesthesia for vascular surgery. Anesthesiol Clin 2014;32:639–659.
- Guay J: Regional anesthesia for carotid surgery. Curr Opin Anaesthesiol 2008; 21:638–644.
- Narouze S: Sonoanatomy of the cervical spinal nerve roots: implications for brachial plexus block. Reg Anesth Pain Med 2009;34:616.
- Roessel T, Wiessner D, Heller AR, et al: High-resolution ultrasound-guided high interscalene plexus block for carotid endarterectomy. Reg Anesth Pain Med 2007;32:247–253.
- Soeding P, Eizenberg N: Review article: anatomical considerations for ultrasound guidance for regional anesthesia of the neck and upper limb. Can J Anaesth 2009;56:518–533.
- Tran DQ, Dugani S, Finlayson RJ: A randomized comparison between ultrasound-guided and landmark-based superficial cervical plexus block. Reg Anesth Pain Med 2010;35:539–543
- Usui Y, Kobayashi T, Kakinuma H, Watanabe K, Kitajima T, Matsuno K: An anatomical basis for blocking of the deep cervical plexus and cervical sympathetic tract using an ultrasound-guided technique. Anesth Analg 2010;110:964–968
- Choquet O, Dadure C, Capdevila X: Ultrasound-guided deep or intermediate cervical plexus block: the target should be the posterior cervical space. Anesth Analg 2010;111:1563–1564
- Dhonneur G, Saidi NE, Merle JC, Asfazadourian H, Ndoko SK, Bloc S: Demonstration of the spread of injectate with deep cervical plexus block: a case series. Reg Anesth Pain Med 2007;32:116–119
- Seidel R, Schulze M, Zukowski K, Wree A: Ultraschallgesteuerte intermediäre zervikale Plexusanästhesie; Anatomische Untersuchung [Ultrasound-guided intermediate cervical plexus block: Anatomical study]. Anaesthesist 2015;64:446–450
- Calderon AL, Zetlaoui P, Benatir F, et al. Ultrasound-guided intermediate cervical plexus block for carotid endarterectomy using a new anterior approach: a two-centre prospective observational study. Anaesthesia 2015; 70:445–451
- Saranteas T, Kostopanagiotou GG, Anagnostopoulou S, Mourouzis K, Sidiropoulou T: A simple method for blocking the deep cervical nerve plexus using an ultrasound-guided technique. Anaesth Intensive Care 2011;39:971–972
- Perisanidis C, Saranteas T, Kostopanagiotou G: Ultrasound-guided combined intermediate and deep cervical plexus nerve block for regional anaesthesia in oral and maxillofacial surgery. Dentomaxillofac Radiol 2013;42:29945724
- Sandeman DJ, Griffiths MJ, Lennox AF: Ultrasound guided deep cervical plexus block. Anaesth Intensive Care 2006;34:240–244.