The transversus abdominis plane (TAP) block is used to produce a dermatomal sensory block of the lower thoracic and upper lumbar afferents. Installation of local anesthetics in this plane anesthetizes the anterior abdominal wall on this side. This block can be used as a diagnostic tool or as a therapeutic modality via a continuous indwelling catheter for postoperative lower abdominal pain or chronic pain syndromes arising from the anterior abdominal wall. TAP block is a new technique for peripheral nerve block of the thoracolumbar nerves supplying the anterior abdominal wall. It was investigated for different applications for perioperative pain management following abdominal surgeries. With ultrasound imaging, the muscle layers are visible from the rectus medially through the aponeurotic area at the edge of the rectus to the three distinct layers of external, internal oblique, and transversus abdominis in the lateral abdominal wall. The introduction of ultrasound-guided regional anesthesia allows the successful installation of local anesthetics around the anterior branches of the thoracolumbar ventral rami, thereby blocking somatic sensations from the anterior abdominal wall. A single injection as well as continuous infusions can be used for the treatment of chronic pain syndromes following lower abdominal open and laparoscopic surgeries [1]. Abdominal pain is one of the most frequent complaints heard by a primary care physician, accounting for nearly 2.5 million office visits per year; in up to 50% of patients, no identifiable cause can be found [2]. Somatosensory pain (abdominal wall pain) can sometimes be confused with the visceral pain origin, and a differential epidural block is often performed to help differentiate between the two types of pain [3]. However, the interpretation of the differential epidural test sometimes is very confusing. It is time-consuming (takes a few hours), and it carries the limitations and disadvantages of neuroaxial blocks. The author found that the TAP block is very valuable in diagnosing pain stemming from the abdominal wall; it can thus help differentiate between the somatosensory (abdominal wall) and the visceral origin of pain [1].
1. ANATOMY
The abdominal wall consists of three muscle layers: the external oblique, the internal oblique, and the transversus abdominis and their associated fascial sheaths.
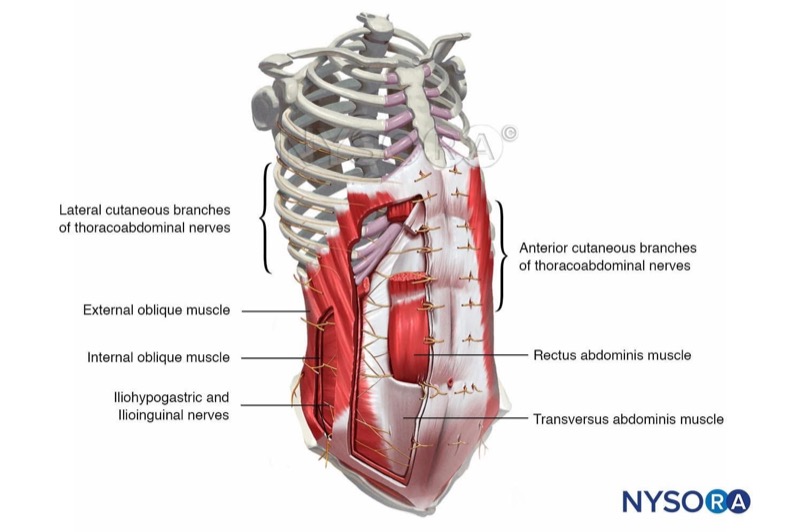
Cognitive aid: Muscles and innervation of the abdominal wall.
For additional information check NYSORA Compendium: Transversus Abdominis Plane Block.
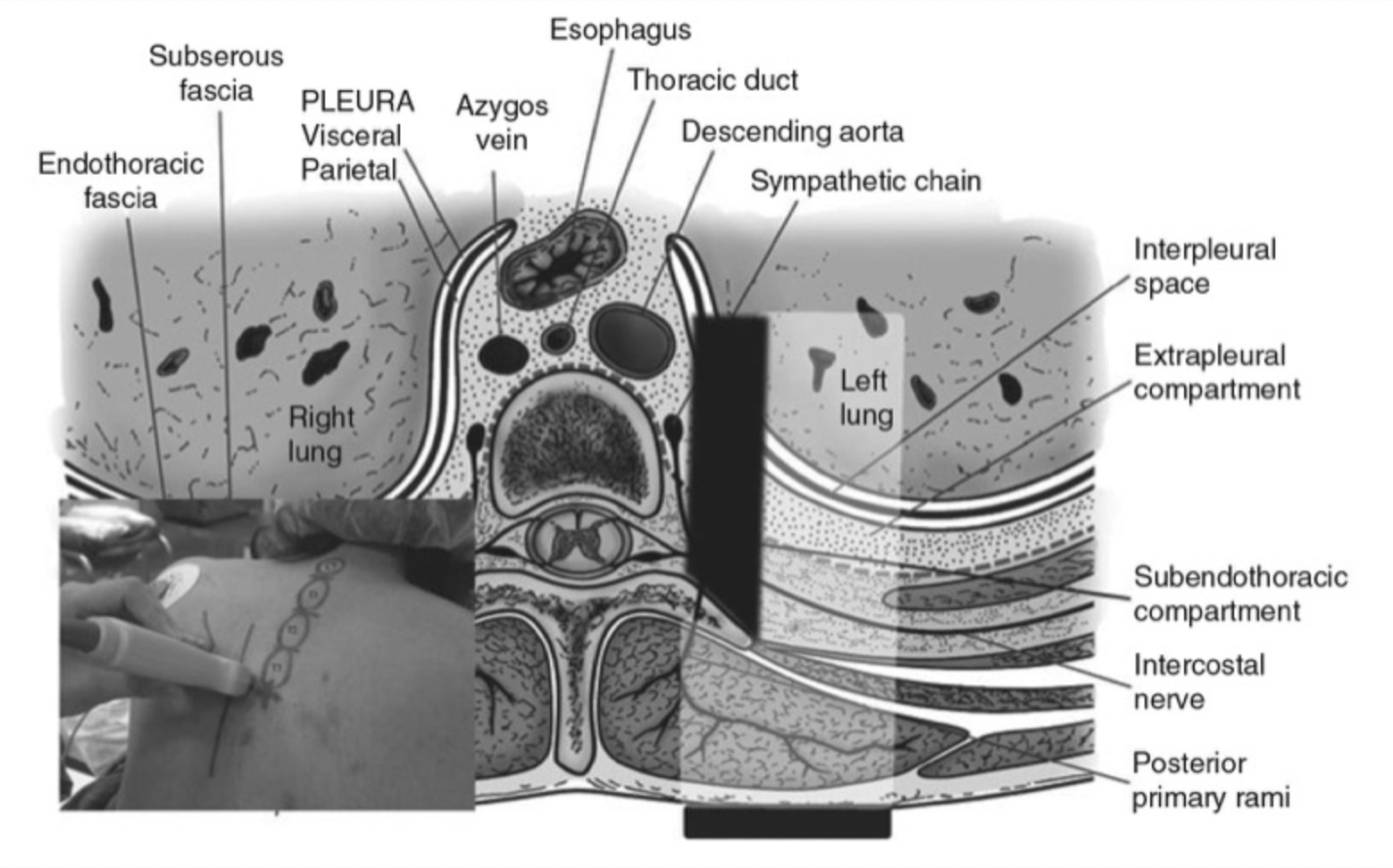
These muscles are mainly innervated via the ipsilateral ventral rami of T7 to L1 thoracolumbar nerves. After emerging through the intervertebral foramina, they follow a curvilinear course forward in the intercostal spaces toward the midline of the body. Along this course, they enter a fascial plane between the transversus abdominis and the internal oblique muscles accompanied by blood vessels in what is known as the TAP compartment. This neurovascular plan continues as far as the semilunar line. At the lateral border of the rectus abdominis muscle, the external oblique and the anterior lamella of the internal oblique aponeuroses pass anterior to the muscle, forming the anterior rectus sheath. The aponeuroses from the posterior lamella of the internal oblique and the transversus abdominis muscle pass posterior to the rectus muscle, forming the posterior layer of the sheath. At this point, the ventral rami of the thoracic spinal nerves are located between the posterior border of the rectus muscle and the posterior rectus sheath. They run medially within the sheath before perforating the muscle anteriorly, forming the anterior cutaneous branches.
The anterior ramus of the 10th thoracic nerve reaches the skin at the level of the umbilicus, and the 12th thoracic nerve innervates the skin of the hypogastrium. The iliohypogastric and ilioinguinal nerves follow a similar course; however, they pierce the internal oblique muscle at different levels near the anterior superior iliac spine in order to supply the inguinal region.
2. THE CLASSIC APPROACH
The TAP block was first described by Rafi and McDonell as a blind “double-pop” technique using a blunt needle introduced through the external and internal oblique muscles and fascia at the iliolumbar triangle of Petit [5, 6]. This triangle is bounded posteriorly by the latissimus dorsi muscle and anteriorly by the external oblique muscle, with the iliac crest forming the base of the triangle. The introduction of ultrasound allows modification of this technique, and the TAP can be accessed anywhere between the iliac crest and costal margin behind the anterior axillary line.
3. ULTRASOUND-GUIDED TECHNIQUE
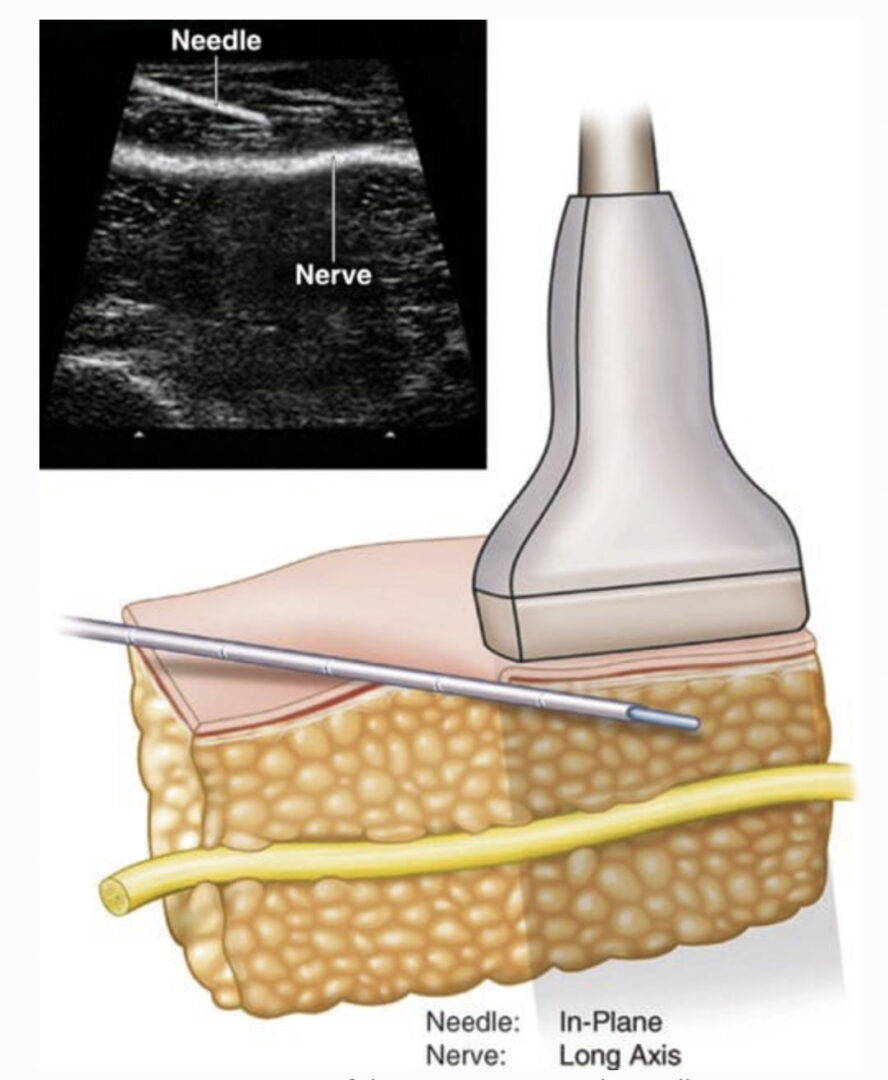
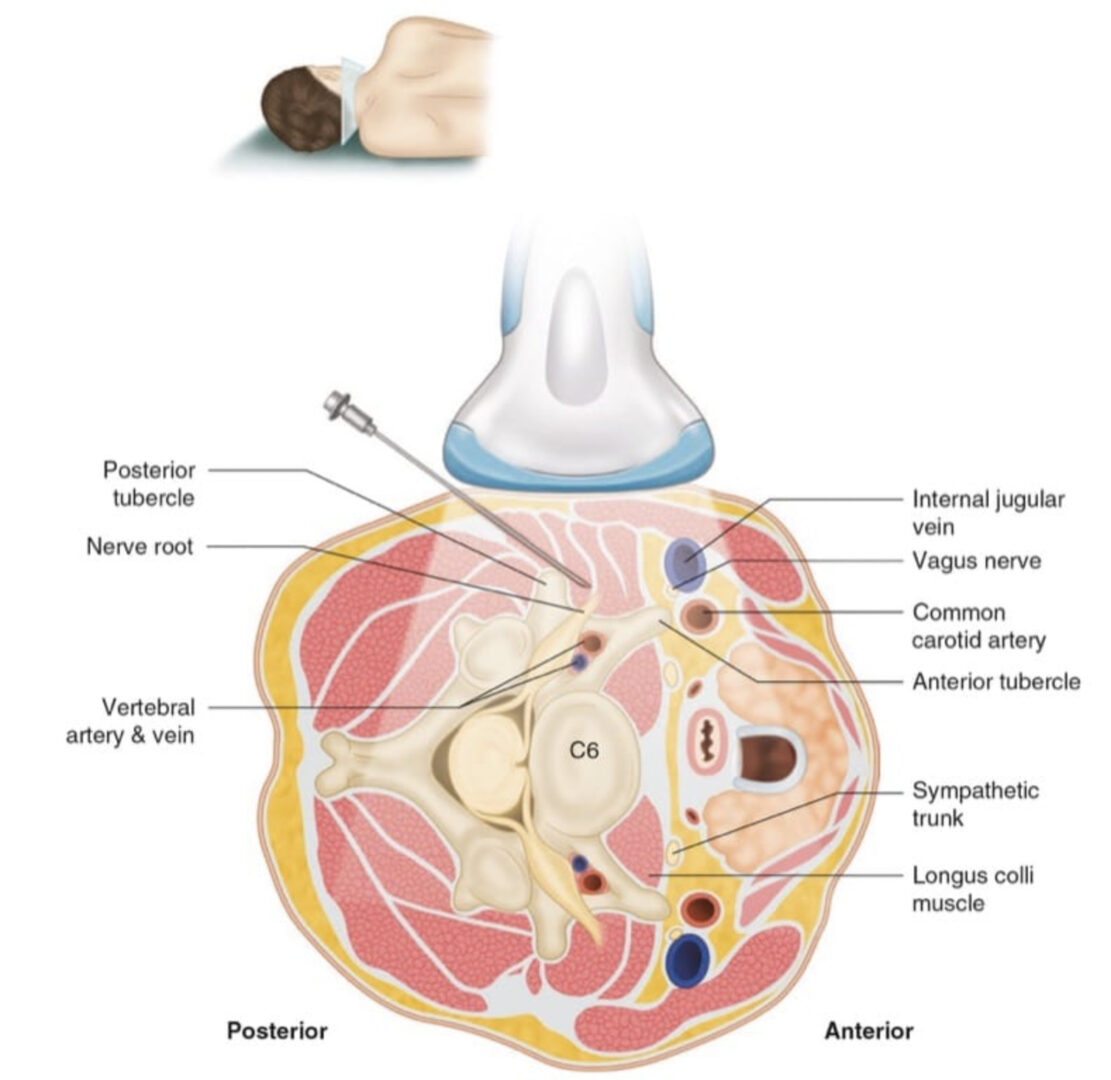
Ultrasound (US)-guided TAP block was first described more anterior to the Petit triangle, between the iliac crest and the subcostal margin via an in-plane approach in the midaxillary line. The patient is positioned in the lateral decubitus position with the side to be blocked facing upward. A wedge can be placed underneath the patient in order to stretch the flank on the upper side. A high frequency or lower frequency transducers may be used according to body habitus. Preprocedural scanning of the anterior abdominal wall along the midaxillary line is recommended in order to decide the best view of the three muscle layers. Care should be taken that scanning more medially may only show two layers of muscles, since the external oblique muscle forms an aponeurosis that joins the rectus sheath. From superficial to deep, the following structures are recognized: skin and subcutaneous fat and external oblique, internal oblique, and transversus abdominis muscles with their investing fasciae (Figs. 1 and 2). Deeper to the transversus abdominis and its fasciae, there is a fatty layer of preperitoneal fat separating it from the peritoneum and the bowels, which is often identified by its peristaltic movements. With ultrasound, the fascial layers appear as hyperechoic layers (whiter than the surrounding structures), and the muscles are identified by their relative hypoechoic structure with multiple striations. The neural structures are usually difficult to identify; however, scanning immediately cephalad to the ASIS can identify the iliohypogastric and ilioinguinal nerves.
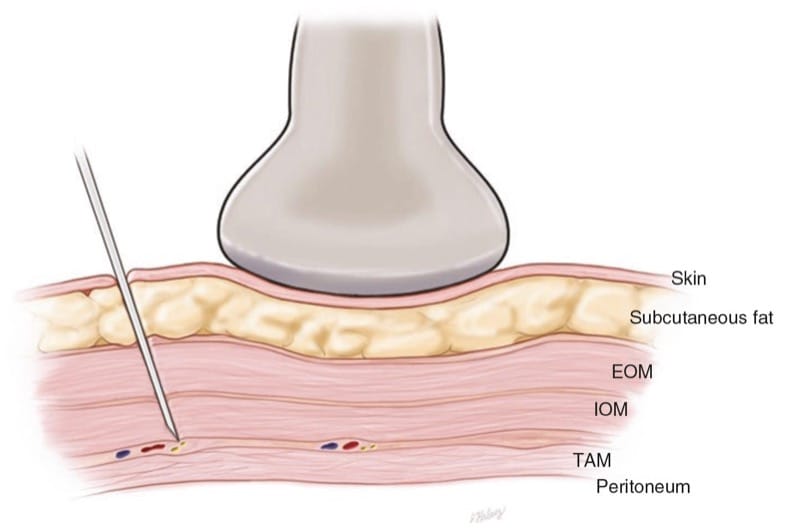
Fig.1 The abdominal wall muscles and the ultrasound transducer in place for performing TAP block are shown
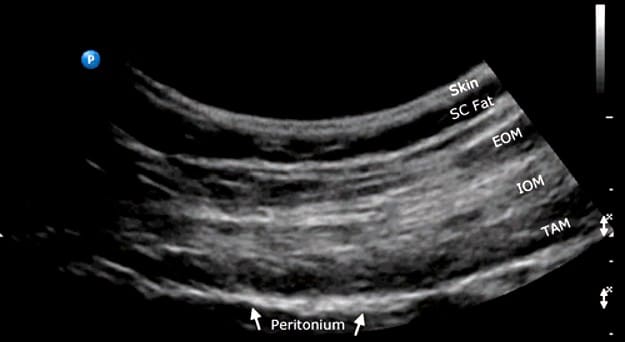
Fig.2 Preinjection short-axis sonogram showing the abdominal wall muscle layers. EOM external oblique muscle, IOM internal oblique muscle, TAM transversus abdominis muscle. (Reprinted with permission from Ohio Pain and Headache Institute)
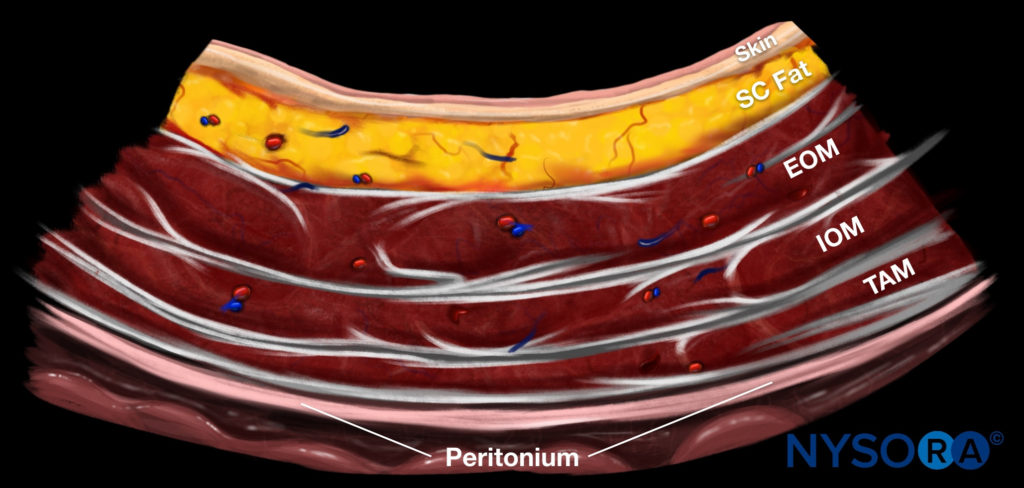
Reverse Ultrasound Anatomy illustration of figure 2. EOM, external oblique muscle; IOM, internal oblique muscle; TAM, transversus abdominis muscle.
The needle is inserted in-plane (parallel to the ultrasound beam) from the posterolateral side of the probe and is advanced in a medial and anterior direction. In order to have a clear picture of the needle, it is preferable to introduce it 1–2 inches farther from the probe to avoid a steep introductory angle that can be unfavorable for the reflection of the ultrasound beam. The needle is advanced through the different layers with a tactile feeling of a pop when crossing each fascial layer. Gentle tapping on the needle can help identify the tip advancing under ultrasound. Alternatively, the appropriate plane can be confirmed by injection of few millimeters of saline or local anesthetic (hydrolocalization). Correct placement is identified by the solution, separating the internal oblique muscle superficially from the deep transversus abdominis muscle (Fig. 3). Care should be taken to identify the injection along the appropriate plane as opposed to the intramuscular injection, which leads to swelling of the muscles instead of separation.

Fig.3 Postinjection short-axis sonogram showing the spread of the injectate in the plane between the internal oblique muscle (IOM) and the transversus abdominis muscle (TAM). Note that the TAM and the peritoneum were pushed away by the injectate. (Reprinted with permission from Ohio Pain and Headache Institute)
It is important to use a blunt-tip needle for the TAP block to appreciate the tactile feedback when crossing different layers and to minimize the chances of peritoneal and bowel perforation.
A higher subcostal approach (subcostal TAP block) may block the upper thoracolumbar nerves more effectively than a lower approach immediately above the iliac crest [7].
The needle is inserted in-plane from the anteromedial to the inferolateral direction with a local injection between the rectus abdominis and transversus abdominis, more medial than the anterior axillary line. This block covers the upper abdominal incision more adequately, corresponding to dermatomes T6 to T9 (i.e., laparoscopic cholecystectomy, gastric bypass, after liver transplant and resection).
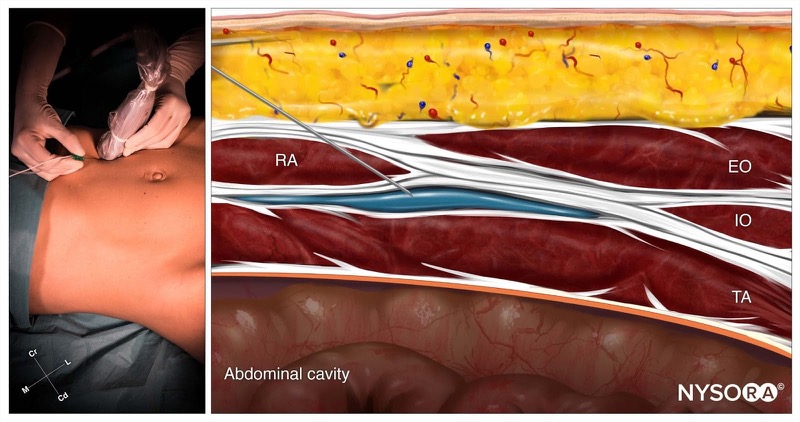
Cognitive aid: Subcostal TAP block; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). TA, transversus abdominis; RA, rectus abdominis; IO, internal oblique; EO, external oblique. For additional information check NYSORA Compendium: Transversus Abdominis Plane Block.
4. ULTRASOUND-GUIDED TAP CATHETER
A continuous TAP catheter has the advantages of prolonging the analgesic effect beyond the block coverage and also can be used in patients with preoperative coagulopathy, which precludes neuroaxial block. It is easy to perform preoperatively using the same technique described earlier for the block. However, instead of using a blunt 22-G needle, a Tuohy needle is used, and the space between the two muscles is dissected using 10 mL of saline followed by a catheter insertion for about 5–7 cm beyond the tip of the needle (Fig. 4). In case the catheter tip position cannot be identified under ultrasound, other methods such as hydrodissection, injection of 0.5 mL of air after negative aspiration from the catheter, or use of the Doppler to move the catheter stylet can give an idea about the tip position [8]. Some authors have described surgically assisted catheter placement under direct vision and use of an infusion device during procedure.
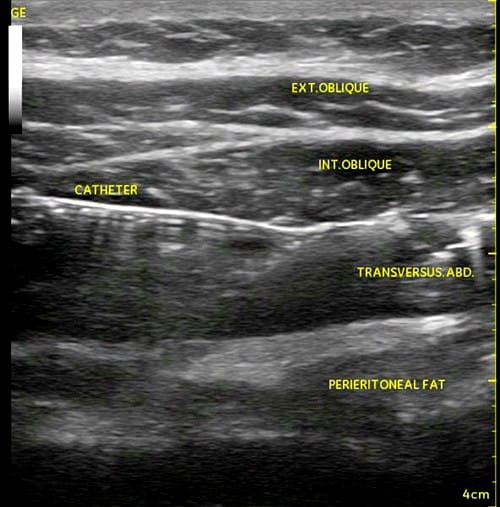
Fig.4 Showing the catheter between the IOM internal oblique muscle and TAM transversus abdominis muscle
Multiple recent trials showed equivalence and advantage of continuous TAP infusion versus epidural analgesia and single TAP injection in controlling abdominal postoperative pain [9].
5. SUMMARY
Ultrasound-guided TAP block is a novel block with multiple applications for pain control following various lower abdominal surgeries. It produces a unilateral analgesia between the coastal margin and the inguinal ligament. It may also have applications in the diagnosis and management of chronic abdominal pain syndromes [10]. Ultrasound-guided iliohypogastric and ilioinguinal nerve blocks are essentially a TAP block performed near the level of ASIS.