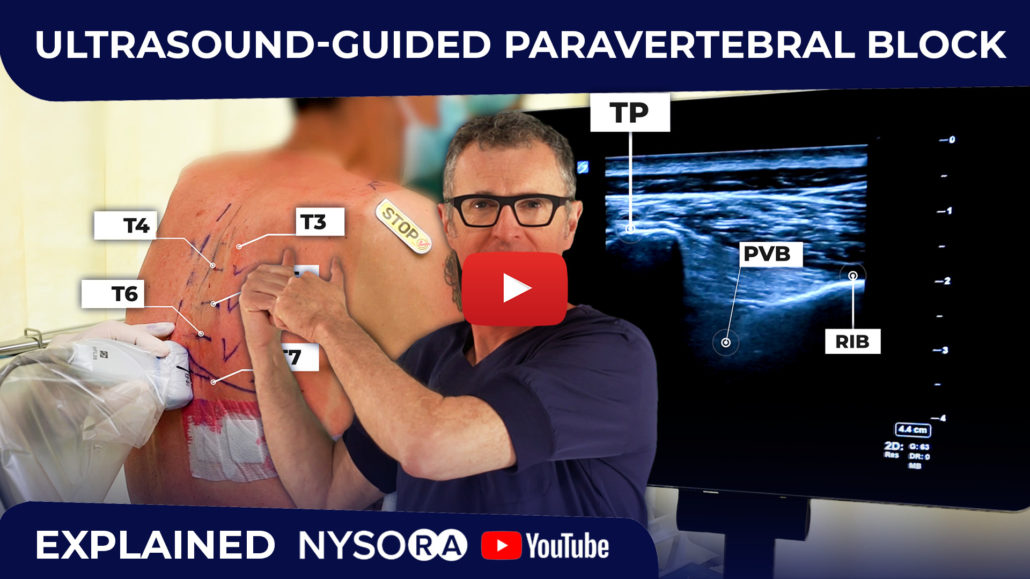
Why is an US-Guided Paravertebral Block Challenging?
In this newsletter and in the video on NYSORA YouTube channel, we feature an ultrasound-guided paravertebral block technique. Make sure you test-drive the NYSORA’s Compendium of Regional Anesthesia for full video and description of the paravertebral block. The paravertebral block is the most effective analgesic technique in patients having breast surgery, thoracotomy, procedures involving the thoracic and upper abdominal wall. Paravertebral and intercostal blocks are also very useful in patients with herpes zoster neuralgia. Conceptually, the technique is relatively simple, and it consists of an injection of local anesthetic into the paravertebral space where spinal nerves exit from the intervertebral foramen.
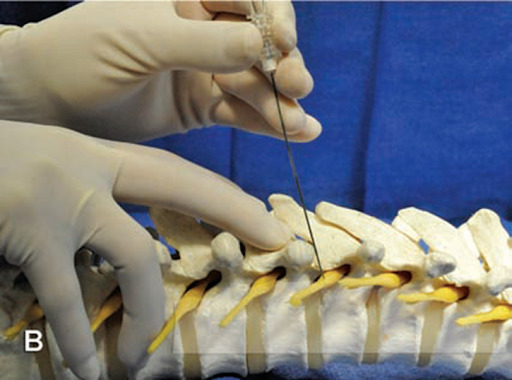
An image demonstrating needle placement into the paravertebral place where blocks of the spinal nerves takes place. From NYSORA’s Compendium of Regional Anesthesia.
We recommend one injection to be performed at the level of the incision or source of pain, and two levels above and two levels below. Typically, 4-5 mL of local anesthetic is injected for each level, which results in a spread in the paravertebral space, intercostal spaces, and often, epidurally.
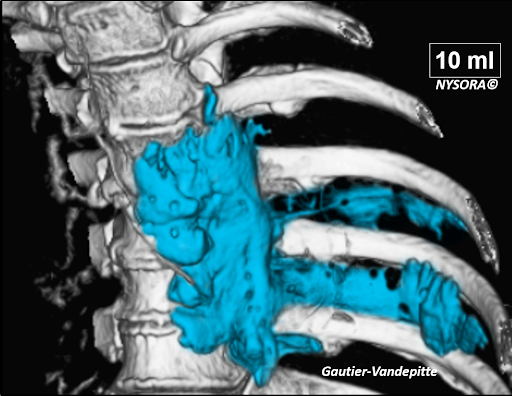
Spread of 10 mL of local anesthetic in the paravertebral space, epidural space and intercostal space after injection at one, single, thoracic paravertebral level.
Ultrasound guidance helps to identify the paravertebral space with more precision than the landmark-based technique. Ultrasound guidance also helps monitor the needle placement and the local anesthetic spread. However, it should be noted that ultrasound-guided PVB is one of the most challenging techniques which requires a high degree of skill due to the close proximity of highly vulnerable structures and the depth of the paravertebral space.
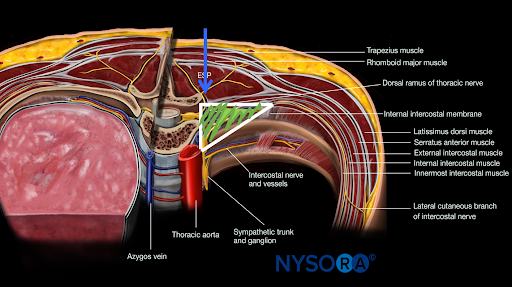
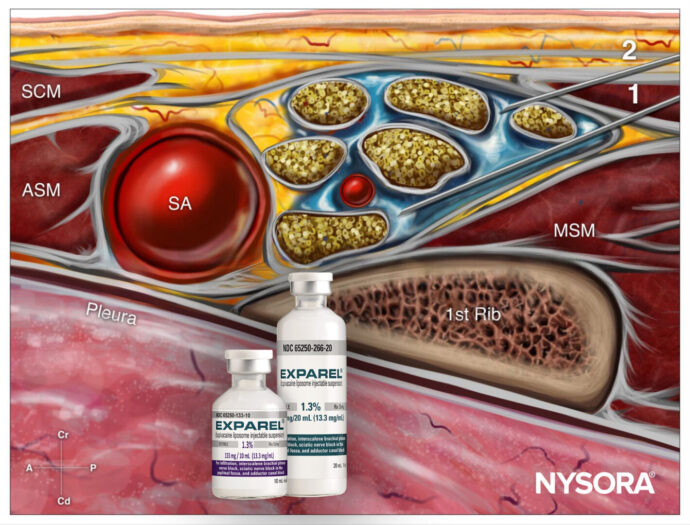
Anatomy of the paravertebral space and the shape of the paravertebral space (triangle).
Our recommendation is to utilize either ultrasound-assisted technique, or ultrasound-guided out-of-plane techniques as the safest. In both techniques, it is advisable that the operator uses a needle with depth markings, so that that depth of needle insertion is always objectively controlled, regardless of the ultrasound image quality.

The technique of ultrasound-guided paravertebral bock using an out-of-plane approach as featured in the video.