Learning objectives
- Define inflammatory bowel disease
- Describe the differences between Crohn’s disease and ulcerative colitis
- Anesthetic management of a patient with inflammatory bowel disease
Definition and mechanisms
- Inflammatory bowel disease (IBD) is a term for two conditions (Crohn’s disease and ulcerative colitis) that are characterized by chronic inflammation of the gastrointestinal (GI) tract
- Prolonged inflammation results in damage to the GI tract
- Caused by an interaction of environmental and genetic factors leading to immune responses and inflammation in the intestine → autoimmune disease
| IBD | Crohn’s disease | Ulcerative colitis |
|---|---|---|
| Affected location | Can affect any part of the GI tract (from mouth to anus), most often affects the portion of the small intestine before the large intestine (i.e., ileocecal region) | Restricted to the large intestine (colon) and rectum |
| Damaged areas | Damaged areas appear in patches that are next to areas of healthy tissue | Damaged areas are continuous (not patchy), usually starting at the rectum and spreading further into the colon |
| Inflammation | Inflammation may reach through the multiple layers of the walls of the GI tract → transmural inflammation leading to abscesses or granulomatous disease | Inflammation is present only in the innermost layer of the lining of the colon (i.e., mucosa) → loss of colonic mucosa |
Signs and symptoms
- Persistent diarrhea
- Fatigue
- Abdominal pain and cramping
- Rectal bleeding, bloody stools
- Reduced appetite
- Unintended weight loss
Complications
Both conditions
- Anemia (due to prolonged GI bleeding, often iron and/or vitamin B12 deficiency)
- Colorectal cancer
- Skin, eye, and joint inflammation (e.g., iritis/uveitis, ankylosing spondylitis)
- Medication side effects (e.g., infections, corticosteroids are associated with a risk of osteoporosis and hypertension)
- Primary sclerosing cholangitis
- Blood clots (i.e., venous thromboembolism [VTE])
- Severe dehydration
Crohn’s disease
- Bowel obstruction
- Malnutrition
- (Perianal) fistulas, may form an abscess
- Anal fissure
Ulcerative colitis
- Toxic megacolon
- Perforated colon
Risk factors
- Age
- Most people are diagnosed before 30 years of age
- Some people do not develop the disease until their 50-60s
- White ethnicity
- Family history
- Smoking
- NSAIDs medications (e.g., ibuprofen, naproxen sodium, diclofenac sodium)
Diagnosis
Combination of endoscopy (for Crohn’s disease) or colonoscopy (for ulcerative colitis) and imaging studies
- Contrast radiography
- MRI
- CT
- Stool samples
- Blood tests
Treatment
- Antidiarrheal medications (i.e., psyllium powder, methylcellulose, loperamide)
- Anti-inflammatory drugs (i.e., glucocorticoids, 5-aminosalicylic acids)
- Immunosuppressants (i.e., cyclosporine, azathioprine, mercaptopurine, methotrexate)
- Antibiotics (i.e., ciprofloxacin, metronidazole)
- Biologics (i.e., TNF-α inhibitor infliximab)
- Nutritional support
- Surgery to remove damaged parts of the GI tract
Management
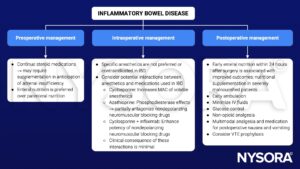
IBD medication management during the perioperative period
| Drug | Recommendation |
|---|---|
| Glucocorticoids | Continue; administer stress dose (see next table) |
| 5-aminosalicylic acid | Discontinue on day of surgery and resume 3 days after surgery if normal renal function |
| Azathioprine, 6-mercaptopurine | Discontinue on day of surgery and resume 3 days after surgery if normal renal function |
| Methotrexate | Continue unless previous poor wound healing or postoperative infections |
| Cyclosporine | Continue but carefully monitor for infectious complications |
| Infliximab | Continue without interruption |
Glucocorticoid management during the perioperative period
| Axis suppression | Minor surgical stress | Moderate surgical stress | Major surgical stress |
|---|---|---|---|
| No Prednisone < 5 mg/d Glucocorticoids < 3 weeks Negative corticotropin test | Daily dose No supplementation | Daily dose No supplementation | Daily dose No supplementation |
| Documented or suspected Prednisone > 10 mg/d for > 3 weeks Positive corticotropin test | Daily dose No supplementation | Hydrocortisone 50 mg IV (induction) 25 mg IV every 8 hours for 24-48 hours | Hydrocortisone 100 mg IV (induction) 50 mg IV every 8 hours for 24 hours 25 mg IV every 8 hours for 24-48 hours |
| Unknown Prednisone 5-10 mg ≥ 3 weeks | Daily dose No supplementation | Positive corticotropin test Hydrocortisone 50 mg IV (induction) 25 mg IV every 8 hours for 24-48 hours | Hydrocortisone 100 mg IV (induction) 50 mg IV every 8 hours for 24 hours 25 mg IV every 8 hours for 24-48 hours |
See also perioperative steroids considerations
Suggested reading
- Nickerson TP, Merchea A. Perioperative Considerations in Crohn Disease and Ulcerative Colitis. Clin Colon Rectal Surg. 2016;29(2):80-84.
- Kumar A, Auron M, Aneja A, Mohr F, Jain A, Shen B. Inflammatory bowel disease: perioperative pharmacological considerations. Mayo Clin Proc. 2011;86(8):748-757.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com